Category: Neurology
Keywords: stroke, seizure (PubMed Search)
Posted: 2/3/2011 by Aisha Liferidge, MD
(Updated: 2/7/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: hemoglobin, anemia, transfusions, hemorrhage, conservative, liberal, hemorrhaging (PubMed Search)
Posted: 2/1/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The optimal hemoglobin concentration during critical illness is unknown. Although a liberal transfusion strategy (Hb 10-12 g/dL) was once believed to be beneficial for hemodynamics, evidence suggests targeting a conservative strategy (Hb 7-9 g/dL) does not increase mortality, while the unnecessary transfusion of blood products can cause harm (transfusion associated lung injury, infection, etc.) in the non-hemorrhaging patient.
1. Harder, L. Et al. The Optimal Hematocrit. Critical Care Clinics (2010) vol. 26 (2) pp. 335-354
2. Hebert P, Wells G, Blajchman M, et al. A multicenter, randomized, controlled clinical trial of transfusion requirements in critical care. N Engl J Med 1999; 340(6):409–17
Category: Trauma
Keywords: Apical cap, dissection, blunt aortic injury, chest xray, radiology (PubMed Search)
Posted: 1/31/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
44 y/o female restrained driver s/p motor vehicle crash complaining of chest pain and shortness of breath.
Answer: Left pleural apical cap.
The Apical Cap
An apical cap is a unilateral or bilateral irregular density over the apex of the lung, generally less than 5mm. The lower border is often sharp but undulating.
Differential diagnosis:
Fabian TC, Richardson JD, Smith JS Jr, et al. Prospective study of blunt aortic injury: multi-center trial of the American Association for the Surgery of Trauma. J Trauma 1997;42:374-383.
McLoud TC, Isler RJ, Novelline RA, et al. The apical cap. Amer J Rad 1981; 137:299-306.
Rivas LA, Fishman JE, Munera F, et al. Multislice CT in thoracic trauma. Radiol Clin North Am2003; 41:599-616.
Category: Toxicology
Keywords: Dabigatran, anti-coagulation, toxicology, coumadin (PubMed Search)
Posted: 1/27/2011 by Fermin Barrueto
Click here to contact Fermin Barrueto
Dabigatran (Pradaxa), an antithrombin medication, was discussed in an earlier pearl and thought I would play devil's advocate and explain the possible concerns:
Toxicology Mantra: You never want to be the first person or the last person to use a drug
Category: Neurology
Posted: 1/26/2011 by Aisha Liferidge, MD
(Updated: 2/7/2026)
Click here to contact Aisha Liferidge, MD
|
Kittner SJ, Stern BJ, Feeser BR, Hebel R, Nagey DA, Buchholz DW, Earley CJ, Johnson CJ, Macko RF, Sloan MA, Wityk RJ, Wozniak MA. Pregnancy and the risk of stroke. N Engl J Med. 1996;335:768-774.
Category: Critical Care
Posted: 1/26/2011 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Valproic Acid in Status Epilepticus
Pillow MT, Malani N. Best practices for seizure management in the emergency department. ACEP News 2011; 30(1):14-16.
Category: Cardiology
Keywords: Coumadin (PubMed Search)
Posted: 1/24/2011 by Rob Rogers, MD
Click here to contact Rob Rogers, MD
Well, there may finally be a replacement for patients with atrial fibrillation who take warfarin (Coumadin).
In late 2010, the FDA approved the drug Dabigatran (Pradaxa) for use in patients with atrial fibrillation.
Dabigatran is an oral direct thrombin inhibitor that has been approved for stroke prevention in patients with A Fib. The drug does not need monitoring like warfarin, and has been deemed to be safer than warfarin.
Be on the lookout for Dabigatran...
Category: Cardiology
Keywords: bretylium, hypothermia, ventricular fibrillation (PubMed Search)
Posted: 1/23/2011 by Amal Mattu, MD
(Updated: 2/7/2026)
Click here to contact Amal Mattu, MD
Bretylium was touted for many years as the drug of choice for patients with ventricular dysrhythmias in the setting of hypothermia...in fact it still is recommended by some. Bretylium was actually touted to be effective based on animal studies in which the dogs were PRE-treated with bretylium and then hypothermia was induced. It was found that dogs that were pretreated had fewer episodes of ventricular fibrillation than dogs that were not pretreated. On the other hand, if bretylium was used as a treatment for VFib rather than a prophylactic, it was ineffective. The bottom line....don't bother with bretylium.
Category: Orthopedics
Keywords: iliotibial band, knee pain (PubMed Search)
Posted: 1/22/2011 by Brian Corwell, MD
(Updated: 2/19/2011)
Click here to contact Brian Corwell, MD
Iliotibial band syndrome (ITBS)
http://footcarexpress.com/foot-orthotics/wp-content/uploads/2009/01/iliotibial-band-syndrome.jpg
Hx -
PE-
Tx
Category: Neurology
Keywords: parkinson's disease, movemnt disorder, levodopa (PubMed Search)
Posted: 1/20/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: Apnea test, brain death, brain stem death, coma, death, cardiopulmonary death (PubMed Search)
Posted: 1/17/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Brain death is the permanent absence of cerebral and brainstem functions (coma, absent pupillary reflexes, no spontaneous respiration, etc.). Legally, brain death is equivalent to cardiopulmonary death.
If brain death is suspected, confirmation is necessary. The apnea test is most commonly used, evaluating for spontaneous breaths when disconnected from the ventilator. If apnea testing is not possible (e.g., ambiguous clinical exam or cardiopulmonary instability) ancillary testing is needed:
Wijdicks EF, The diagnosis of brain death. N Engl J Med. 2001 Apr 19;344(16):1215-21.
Category: Visual Diagnosis
Keywords: boxer's, fracture, orthopedics, hand, brawler's, radiology, xray (PubMed Search)
Posted: 1/17/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD

Boxer's (or Brawler's) Fracture
Many thanks to Dr. George Kochman for submitting this case!
Category: Cardiology
Keywords: infective endocardtiis, neurological, deficits (PubMed Search)
Posted: 1/16/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Up to 30-40% of patients with infective endocarditis have neurological symptoms as a result of embolization. This is a good reminder of the frequency of embolization, and also that infective endocarditis should always be part of the differential when you are evaluating a patient with fever + neurological abnormalities.
Limkakeng AT Jr., Stahmer SA. Cardiovascular II. In Harrigan RA, Ufberg JW, Tripp ML (eds). Emergency Medicine Review: Preparing for the Boards. Elsevier, St. Louis 2010.
Category: Orthopedics
Keywords: Shoulder, Dislocation, FARES (PubMed Search)
Posted: 1/15/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
FARES Method for Reduction of Anterior Shoulder Dislocations.
This method that was recently highlighted in a publication had a ~78% success rate with the authors able to reduce the shoulder in an average of 2.36 ±1.24 minutes without having to give the patients any analgesics or sedatives. The technique is done by:
Consider trying this with your next shoulder dislocation. No single method of reduciton is 100% successful, but methods like this that only require a single provider and do not require analgesics are extremely helpful in improving patient flow as they do not utilize a lot of ED resources..
Category: Toxicology
Keywords: acetaminophen, rumack-matthew nomogram (PubMed Search)
Posted: 1/13/2011 by Bryan Hayes, PharmD
Click here to contact Bryan Hayes, PharmD
The Rumack-Matthew nomogram is a well studied and validated tool to help assess the potential for liver toxicity following acute acetaminophen poisoning. Here is a brief review of when it is best utilized.
Outside-the-box situations:
Category: Neurology
Keywords: dysmetria, ataxia, cerebellum (PubMed Search)
Posted: 1/12/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 1/11/2011 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Dexmedetomidine for Sedation in Acute Neurologic Disease
Mirski MA, Lewin JL. Sedation and analgesia in acute neurologic disease. Curr Opin Crit Care 2010; 16:81-91
Category: Neurology
Keywords: Image, CT scan, head trauma (PubMed Search)
Posted: 1/10/2011 by Rob Rogers, MD
Click here to contact Rob Rogers, MD
FILE RESEND. This was tested via email and will hopefully work. I apologize for errors - Dlemkin (webmaster)
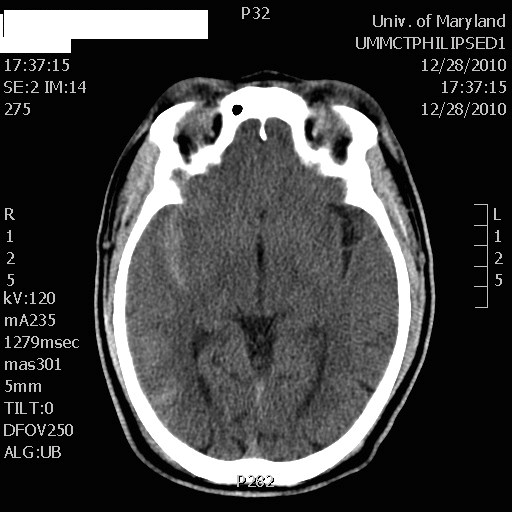
What is the diagnosis? (DON'T LOOK DOWN AT THE ANSWER)
50 year-old male prisoner s/p assault, + LOC
CT shows right-sided traumatic subarachnoid hemorrhage
Category: Cardiology
Keywords: therapeutic hypothermia, hypothermia, saline, cardiac arrest (PubMed Search)
Posted: 1/9/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Therapeutic hypothermia is generally accepted as a useful intervention that should be employed in patients that are resuscitated after cardiac arrest. Many protocols for cooling are relatively complicated, involving endovascular catheters, cooling blankets, cooling helmets, or other devices that are expensive and not widely available. The cooling process can actually be fairly simple, however, with ice and cool IV fluids. The most recent study that demonstrated this used nothing more than application of ice to the groin, neck, and axillae; and administration of 4o C IVF infused at 30cc/kg at 100ml/min via two peripheral catheters. Sedation or paralysis + intubation was used as per the norm.
Patients receiving this simple intervention were able to achieve goal temperature of 32o-34o C within 3-4 hours, and hypothermia was maintained for a full 24 hours before rewarming.
The study shows that expensive equipment and complicated protocols are not necessary for therapeutic hypothermia.
Larsson IM, Wallin E, Rubertsson S. Cold saline infusion and ice packs alone are effective in inducing and maintaining therapeutic hypothermia after cardiac arrest. Resuscitation 2010;81:15-19.
Category: Orthopedics
Posted: 1/8/2011 by Brian Corwell, MD
(Updated: 2/19/2011)
Click here to contact Brian Corwell, MD
Involves an avulsion of the flexor digitorum profundus (FDP) tendon from its insertion on the distal phalanx.
Ring finger is most commonly involved.
Usually occurs from a grabbing attempt (resulting in forced DIP extension during maximal FDP contraction) as would occur while attempting to grab someone’s jersey such as in football or rugby.
Clinically, there is normal passive DIP ROM with loss of active flexion. Examine this by asking the patient to flex the fingertip at the DIP while the PIP joint is held in extension.
*Remember that patients with a 90% full-thickness tendon laceration may still have normal (albeit painful) range of motion. The examiner must evaluation the strength of the tendon against resistance. This injury is commonly missed as it is diagnosed as a “jammed” finger.
Plain films may show a bony avulsion, but are often negative.
Treatment is primary repair especially with large bony fragments. Partial ruptures can be treated nonoperatively at the discretion of the hand surgeon.
