Category: Critical Care
Keywords: AKI, critical care, ICU, cancer, renal failure, acute kidney injury (PubMed Search)
Posted: 6/21/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Cancer patients admitted to ICUs with AKI or who develop AKI during their ICU stay have increased risk of morbidity and mortality. AKI in cancer patients is typically multi-factorial:
Causes indirectly related to malignancy
Septic, cardiogenic, or hypovolemic shock (most common)
Nephrotoxins:
Aminoglycosides
Contrast-induced nephropathy
Chemotherapy
Hemolytic-Uremic Syndrome
Causes directly related to malignancy
Tumor-lysis syndrome
Disseminated Intravascular Coagulation
Obstruction of urinary tract by malignancy
Multiple Myeloma of the kidney
Hypercalcemia
Because AKI increases the already elevated morbidity and mortality in these patients, prevention (e.g., using low-osmolar IV contrast, avoiding nephrotoxins), early identification (e.g., strict attention to urine output and renal function), and aggressive treatment (e.g., early initiation of renal replacement therapy) is essential.
Benoit D. Acute kidney injury in critically ill patients with cancer. Critical Care Clinics 2010 Jan; 26(1): 151-79
Follow me on Twitter @Criticalcarenow
Category: Vascular
Keywords: Aortic Dissection (PubMed Search)
Posted: 6/20/2011 by Rob Rogers, MD
(Updated: 2/8/2026)
Click here to contact Rob Rogers, MD
There are several complications of acute aortic dissection that emergency physicians must be familiar with.
These include:
*Key Pearl: If a patient with suspected or confirmed acute aortic dissection suddenly arrests consider cardiac tamponade.
Category: Cardiology
Keywords: NSAIDS, NSTE-ACS, acute coronary syndrome, non-steroidal anti-inflammatory medications (PubMed Search)
Posted: 6/19/2011 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Patients with Non-STE-ACS should not be given any NSAIDs aside from aspirin...that includes COX-2 agents. These medications in patients with acute or recent NSTE-ACS have been associated with an increased risk of hypertension, reinfarction, heart failure, myocardial rupture, and death.
ACC/AHA Focused Update of the 2007 Non-STE-ACS Guidelines (Circulation 2011)
Category: Orthopedics
Keywords: kocher, septic arthri (PubMed Search)
Posted: 6/18/2011 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Kocher Criteria for Septic Arthritis in Children:
Septic arthritis should be suspected in children that have a painful joint especially if they do not want to weight bear. Orthopedics uses the Kocher Criteria to determine the probability of whether the joint is infected.
Four elements make up the criteria:
If only one sign is present there is a 3% chance the child has a septic joint.
Category: Toxicology
Keywords: hyperglycemia, acidosis, seizures (PubMed Search)
Posted: 6/16/2011 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
The true incidence of drug-induced seizure is very difficult to determine, however, a nice poison center study attempted to determine clinical factors associated with complications (potentially life-threatening) of drug-induced seizures. They found 3 predictors that demonstrated statistically significant associations:
They found a 60% complication rate in drug-induced seizures which is much higher than epileptic seizures. Makes sense since these patients are often sedated/altered or vomiting.
Stimulant Exposure is much more prominent in this population and has increased in mortality.
Interesting point with hyperglycemia, may be a novel marker for poor prognosis. Several studies have confirmed an association between hyperglycemia and increased neuronal injury and mortality in other settings like CVA and TBI.
Take home point - Drug-induced Seizure has a high complication rate in the ED. Watch for the 3 predictors as that may clue you in to the increased risk.
Thundiyil JG et al. J Med Toxicol (2011) 7:16-23
Category: Neurology
Keywords: ischemic stroke, thrombolytic, blood pressure control (PubMed Search)
Posted: 6/15/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 6/14/2011 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
AKI in the Critically Ill Cancer Patient
Benoit DD, Hoste EA. Acute kidney injury in critically ill patients with cancer. Crit Care Clin 2010;26:151-79.
Category: Visual Diagnosis
Posted: 6/12/2011 by Haney Mallemat, MD
(Updated: 6/13/2011)
Click here to contact Haney Mallemat, MD
13 y.o. with shoulder trauma (during basketball game). Arm held in adduction and exquisite scapular tenderness. Diagnosis?
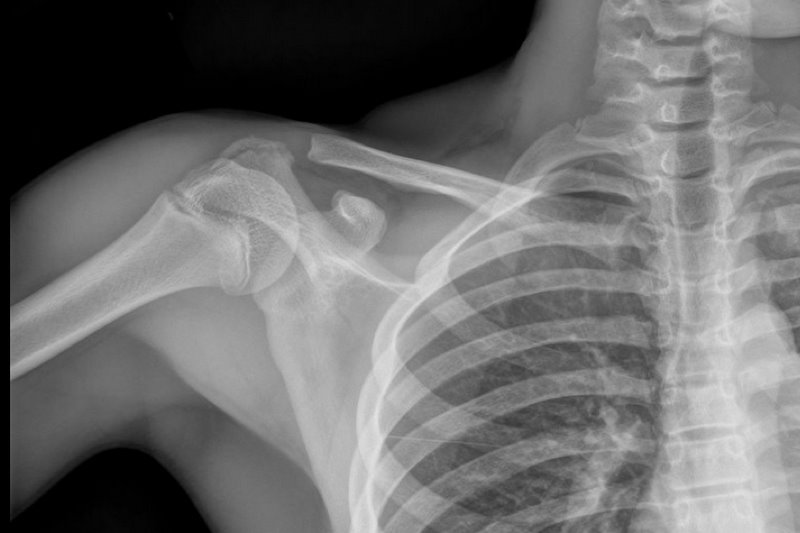
Answer: Scapular Fracture
Scapular Fracture
Uncommon (1% of all fractures)
Extensive force required; high probability of associated injuries (pneumothorax, shoulder dislocation).
5 types: body/spine, acromion, neck, glenoid, and coracoid
Arm held in adduction and pain with shoulder movement; may mimic rotator cuff tear.
Obtain X-rays (AP shoulder and lateral scapula) or CT (if displaced).
Conservative management for non-displaced fractures; Orthopedic reduction for displaced fractures.
Complications include post-traumatic arthritis or bursitis.
NSAIDs are first-line analgesics.
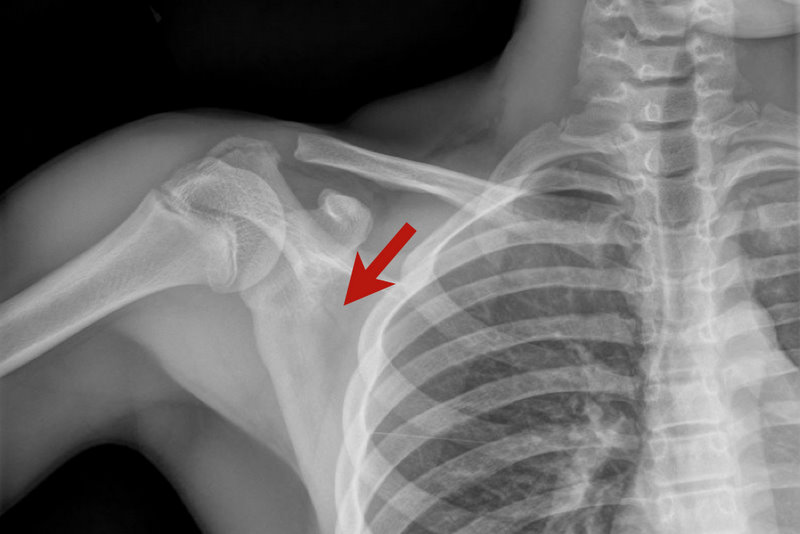
Rosen P, Barkin R. Emergency Medicine: Concepts and Clinical Practice. Mosby Year Book; 2010:573-574.
Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA. Treatment of scapula fractures: systematic review of 520 fractures in 22 case series. J Orthop Trauma. Mar 2006;20(3):230-3.
Category: Cardiology
Keywords: clopidogrel, acute coronary syndrome, proton pump inhibitors (PubMed Search)
Posted: 6/12/2011 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Proton pump inhibitors should be avoided in patients being treated with clopidogrel. PPIs appear to attenuate the effect of clopidogrel, and there's even some suggestion that the addition of PPIs to the medication regimen of patients taking clopidogrel may be associated with an increased risk of rehospitalization or death.
ACC/AHA Focused Update of the 2007 Non-STE-ACS Guidelines (Circulation 2011)
Category: Orthopedics
Keywords: Kienb ck's disease, wrist, avascular necrosis (PubMed Search)
Posted: 6/11/2011 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Kienbock’s disease is a rare entity involving collapse of the lunate due to avascular necrosis and vascular insufficiency.
Occurs most commonly in young adults aged 15 to 40 years.
Cause is unknown but believed to be due to remote trauma or repetitive microtrauma in at risk individuals.
Patients complain of wrist pain, stiffness and swelling
On exam, limited range of motion, decreased grip strength and passive dorsiflexion of the 3rd digit produces pain.
Dx: plain film in the ED and with MRI as an outpatient.
Tx: Wrist immobilization with splint and refer to orthopedics. Ultimate treatment is individualized and there is no clear consensus.
Lunate sclerosis seen on plain film
http://orthoinfo.aaos.org/figures/A00017F02.jpg
AVN of the lunate seen on MRI
http://www.assh.org/Public/HandConditions/PublishingImages/KeinbocksMRI_figure3.JPG
Category: Pediatrics
Keywords: Magnet, Foreign body, pediatric, nose, nasal, perforation (PubMed Search)
Posted: 6/10/2011 by Adam Friedlander, MD
(Updated: 6/11/2011)
Click here to contact Adam Friedlander, MD
If there is a single truth of pediatric emergency medicine, it is that kids love to stuff things into their noses. A particular danger (aside from batteries, covered in a previous pearl) is the magnet.
Specifically, two magnets (as seen with magnet ear and nose rings, frequently worn by children and teens whose pesky parents won't allow piercings), attracted across the nasal septum can cause necrosis and perforation within hours.
Here's how to save yourself (and some noses):
Category: Toxicology
Keywords: lithium, digoxin, colchicine, narrow therapeutic index (PubMed Search)
Posted: 6/6/2011 by Bryan Hayes, PharmD
(Updated: 6/9/2011)
Click here to contact Bryan Hayes, PharmD
Dehydration and subsequent prerenal acute kidney injury can result when temperatures begin to rise in the summer months. As a result, medications with narrow therapeutic indices that are primarily renally excreted may accumulate. Here are the specific ones to look out for:
Category: Neurology
Keywords: nystagmus, visual fixation, peripheral nystagmus, central nystagmus (PubMed Search)
Posted: 6/8/2011 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: uremia, bleeding, ddavp, estrogens, epogen, cryoprecipitate (PubMed Search)
Posted: 6/6/2011 by Haney Mallemat, MD
(Updated: 6/7/2011)
Click here to contact Haney Mallemat, MD
Bleeding associated with uremia is a spectrum, from mild cases (e.g., bruising or prolonged bleeding from venipuncture) to life-threatening (e.g., GI or intracranial bleed). The exact pathologic mechanisms are not understood, but are likely multi-factorial (e.g., dysfunctional von Willebrand’s Factor (vWF) and factor VIII, increased NO, etc.)
Besides dialysis, treatments for uremic bleeding include:
Hedges, SJ. Evidence-based treatment recommendations for uremic bleeding.NatClinPractNephrol.2007 Mar;3(3):138-53.
Category: Visual Diagnosis
Posted: 6/6/2011 by Rob Rogers, MD
Click here to contact Rob Rogers, MD
A 20 year-old female presents with bilateral neck pain that occurred at rest. No other complaints. See if you can find the subtle clue on the x-ray...
The x-ray shows air in the soft tissue of the right neck and supraclavicular area. Close inspection of the mediastinum reveals subtle air along the heart border. Diagnosis: pneumomediastinum.
Often the first clue of pneumomediastinum is air in the neck and supraclavicular area on plain film. So, always look at the soft tissues on chest x-ray.
Category: Cardiology
Keywords: prasugrel (PubMed Search)
Posted: 6/5/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Prasugrel is a new thienopyridine alternative to clopidogrel and is now listed as an option in the 2011 ACC/AHA Non-STEMI ACS Guidelines. Studies comparing it versus clopidogrel show a slight benefit in terms of adverse cardiac events, but at the expense of a slight increase in bleeding complications. Though the guidelines state no preference between prasugrel vs. clopidogral for NSTEMI ACS patients, prasugrel is finding a role in patients who appear to have a genetic resistance to the effects of clopidogrel (unlikely you'll know this in the ED, but you'll start seeing more patients started on this medication in the outpatient setting).
Prasugrel is contraindicated in patients with a history of TIA or stroke and it should not be given before cath is performed (in contrast, some protocols push for clopidogrel as early as possible, even before cath).
Category: Pharmacology & Therapeutics
Keywords: angioedema, angiotensin, ACE inhibitor (PubMed Search)
Posted: 5/12/2011 by Bryan Hayes, PharmD
(Updated: 6/4/2011)
Click here to contact Bryan Hayes, PharmD
Pathophysiology: Angiotensin converting enzyme (ACE) catalyzes the conversion of angiotensin I to angiotensin II. It also degrades bradykinin. Thus, ACE inhibitors have the effects of decreasing angiotensin II and increasing bradykinin. In the presence of ACE inhibition, bradykinin can accumulate and interact with vascular bradykinin B2 receptors, causing vasodilation, increased vascular permeability, increased c-GMP, and release of nitric oxide.
Treatment: Even though we generally treat with standard allergic reaction medications, none counteract the mechanism causing the problem. Steroids, H1-blockers, and H2-blockers should still be considered but may not alter the progression. Airway monitoring and management is paramount.
Category: Toxicology
Keywords: alopecia, acneiform (PubMed Search)
Posted: 6/2/2011 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Certain medications can cause a certain dermatologic pattern. Many fall into a generic waste basket of "contact dermatitis" but here are some more characteristic findings and the drugs that can cause them:
Alopecia - anticoagulants, chemo, phenytoin, retinoids, selenium, thallium
Erythema multiforme - allopurinol, barbiturates, carbamazepine, cimetidine, some antibiotics
Toxic Epidermal Necrolysis (TEN) - allopurinol, bactrim (sulfonamides), mithramycin, PCN, sulfasalazine, nitrofurantoin, phenytoin, prazocin
Category: Neurology
Keywords: nystagmus, vertigo (PubMed Search)
Posted: 6/1/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
| PERIPHERAL | CENTRAL | |
| Nystagmus | ||
| Direction | Fast phase away from lesion; never reverses direction | Sometimes reverses direction if looking in direction of slow phase |
| Type | Horizontal with torsional component, never purely torsional or vertical | Can be in any direction |
| Other neurologic signs | Absent | Often present |
| Postural instability | Unidirectional instability, walking preserved | |
| Effect of visual fixation | Suppressed | Not Suppressed |
| Deafness or tinnitus | May be present | Absent |
Category: Critical Care
Posted: 5/31/2011 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Cardiovascular Complication of ESLD
Al-Khafaji A, Huang DT. Critical care management of patients with end-stage liver disease. Crit Care Med 2011; 39:1157-66.
