Category: Visual Diagnosis
Posted: 5/30/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
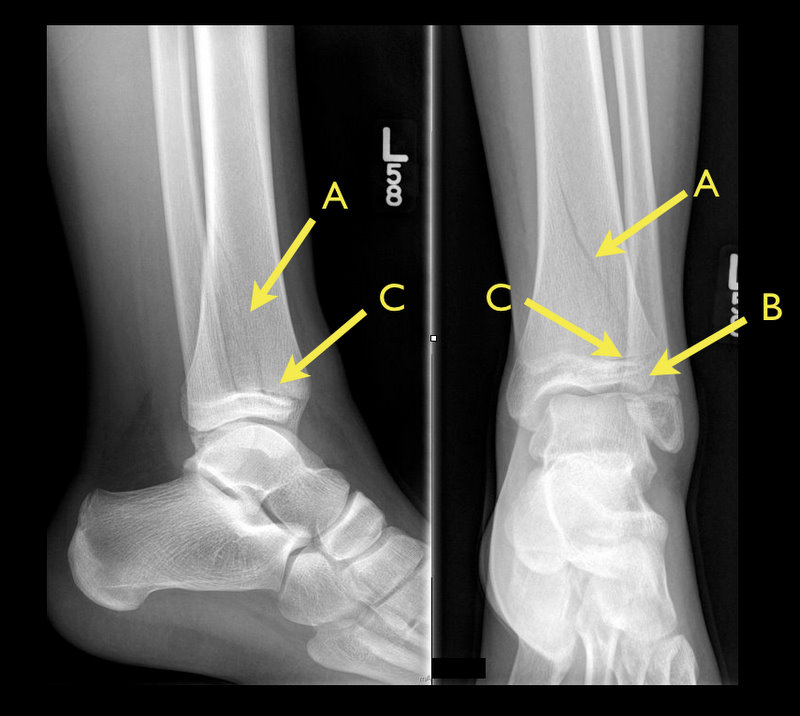
13 y.o. female with ankle pain following fall down escalator. What's the diagnosis? (Hint: Look very closely)

Answer: Tri-plane ankle fracture
Tri-plane Fractures (Submitted and written by Dr. Michael Santiago)

Category: Cardiology
Keywords: therapeutic hypothermia, cardiac arrest, hypothermia, midazolam (PubMed Search)
Posted: 5/29/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Therapeutic hypothermia in post-cardiac arrest patients with return of spontaneous circulation + coma (GCS < 8) is now well-accepted, and the current recommendations are for continued sedation of these patients. Consider avoiding the use of midazolam for sedation in these patients. Midazolam is metabolized more slowly in hypothermic patients, resulting in accumulation and the potential for longer ventilation and ICU time.
Holzer M. Targeted temperature management for comatose survivors of cardiac arrest. N Engl J Med 2010;363:1256-1264.
Category: Orthopedics
Keywords: Brachial plexus, stinger, burner (PubMed Search)
Posted: 5/28/2011 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Transient brachial plexopathies aka Burners and Stingers
Brachial plexus injuries are the most common peripheral nerve injuries seen in athletes.
49-65% of all college football players have experienced at least one burner with a 87% recurrence rate.
Injuries most commonly occur at C5-C6 but may involve any root level.
3 Mechanisms: Commonly due to
1) Traction caused by lateral flexion of the neck away from the involved side
2) Compression of the upper plexus between shoulder pads and scapula
3) Nerve compression caused by neck hyperextension and ipsilateral rotation.
CC: Burning or numbness in the neck, shoulder and/or arm
Symptoms are UNILATERAL and tend to usually last seconds to minutes
Symptoms are reproduced by the Spurling maneuver.
Function gradually returns from the proximal muscle groups to the distal muscle groups.
Because most burners are self-limited, the most important goal is to rule out an unstable cervical injury.
Category: Neurology
Keywords: cerebellar strokes, nystagmus, vertigo, PICA (PubMed Search)
Posted: 5/25/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: neutropenia, sepsis, abdominal pain, necrotizing enterocolitis (PubMed Search)
Posted: 5/23/2011 by Haney Mallemat, MD
(Updated: 5/24/2011)
Click here to contact Haney Mallemat, MD
TIP: Suspect when abdominal pain presents 10-14 after chemotherapy (when PMNs are lowest).

Blijlevens NM, et al. Mucosal barrier injury: biology, pathology, clinical counterparts and consequences of intensive treatment for haematological malignancy: an overview. Bone Marrow Transplant 2000 Jun;25(12):1269-78
http://emedicine.medscape.com/article/375779-overview
Category: Visual Diagnosis
Posted: 5/23/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
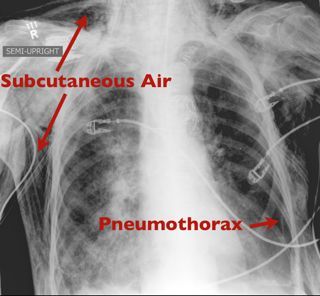
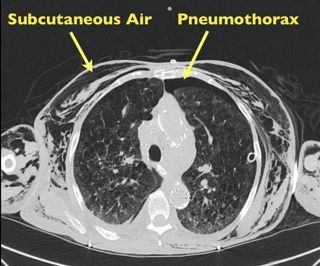
50 yo female s/p motor vehicle crash. Diagnosis?
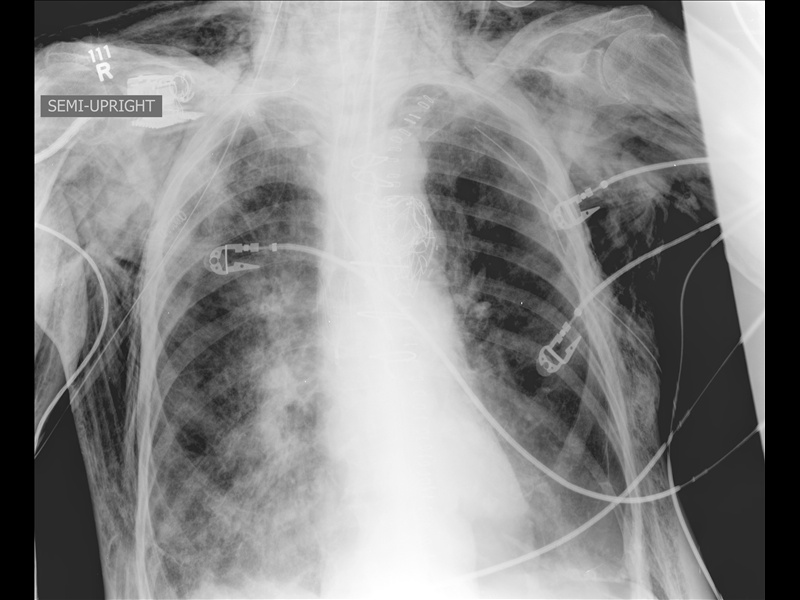
Answer: Pneumomediastinum from pneumothorax
Pneumomediastinum
Mediastinal air has multiple causes:
Listen for Hamman's sign ("crunching" with cardiac auscultation) and feel for crepitus (distinct feeling on palpation).
Treat the precipitating cause.
Usually resolves without mediastinal decompression; air travels along tissue planes decompressing increased mediastinal pressure.
Category: Orthopedics
Keywords: Iliopsoas, tendonitis, syndrome (PubMed Search)
Posted: 5/21/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Iliopsoas tendonitis and Iliopsoas Syndrome
Category: Toxicology
Keywords: lupus, anticoagulants, thrombosis (PubMed Search)
Posted: 5/19/2011 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
The following list of medications have been associated with the development of Lupus Anticoagulants. Though it sounds like they should anticoagulate, they interfere with the Protein C system which means that they could induce a pro-thrombotic state - good short list to know:
Chlorpromazine (Thorazine
Procainamide (sorry Amal, I know you love that drug)
Hydralazine
Quinidine
Phenytoin
Category: Neurology
Keywords: iv tpa, stroke, elderly, intracranial hemorrhage (PubMed Search)
Posted: 5/18/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
(1) do not have increased risk for clinically significant ICH,
(2) have early clinical improvement similar to younger patients, and
(3) have poor outcomes related to increased mortality (odds ratio 30% versus 12%), rather than
to higher rates of functional dependence (i.e. Modified Rankin Score 3 to 5).
Category: Critical Care
Posted: 5/17/2011 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Acute Liver Failure (ALF)
Larsen FS, Bjerring PN. Acute liver failure. Curr Opin Crit Care 2011; 17:160-4.
Category: Airway Management
Posted: 5/16/2011 by Rob Rogers, MD
(Updated: 2/8/2026)
Click here to contact Rob Rogers, MD
Ever see that patient who shows up in the ED with blue painful toes? You look at the foot (or feet) and quickly determine that clot has embolized into the foot.
What is the differential diagnosis to consider in patients with evidence of embolic phenomenon in the feet (i.e. blue, painful toes)?
Things to consider:
Clearly we can't do the complete workup of embolic foot lesions, and many if not most of these patients will need to be admitted to complete their workup.

Medscape images
http://img.medscape.com/pi/emed/ckb/vascular_surgery/459840-463354-3592.jpg
Category: Cardiology
Keywords: therapeutic hypothermia, cardiac arrest, hypothermia (PubMed Search)
Posted: 5/15/2011 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
It is now well-accepted that induction of hypothermia should be initiated in victims of cardiac arrest who regain spontaneous circulation and remain unresponsive. Studies are now being performed and published that suggest that the earlier that hypothermia is induced, the better the neurological outcome. With this in mind, some experts are now recommending that cool IVF be the initial resuscitation fluid that these patients receive when resuscitation is initiated. It appears that aggressive use of cool IVF right from the initiation of attempted resuscitation results in improvements in survival to hospital admission and discharge.
The bottom line here is that when caring for victims of primary cardiac arrest, we should be certain to cool the patients fast and early!
Garrett JS, et al. The association between intra-arrest therapeutic hypothermia and return of spontaneous circulation among individuals experiencing out of hospital cardiac arrest. Resuscitation 2011;82:21-25.
Category: Orthopedics
Keywords: Meralgia Paresthetica, lateral hip pain (PubMed Search)
Posted: 5/14/2011 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Meralgia Paresthetica - caused by entrapment of the lateral femoral cutaneous nerve (LFCN)
The LFCN is responsible for sensation of the anteriorlateral thigh.
http://www.chiropractic-help.com/images/Meralgia-Paresthetica.jpg
NOTE* It has no motor component!
Associated with pregnancy, wearing tight pants, belts, girdles, and in diabetic and obese patients.
Symptoms include numbness, paresthesias and pain (not weakness). Worse w walking, standing. Better w sitting.
Diagnosis is clinical but may be confirmed with nerve conduction studies
Treatment includes, NSAIDs, injection and surgery for refractory cases.
Category: Pediatrics
Keywords: Airway, Intubation, Pediatric, Positioning (PubMed Search)
Posted: 5/13/2011 by Adam Friedlander, MD
(Updated: 8/28/2014)
Click here to contact Adam Friedlander, MD
"Ear to sternal notch" positioning has gained wide acceptance in the emergency medicine and anesthesia literature. Most often, this teaching is brought up with respect to obese adult patients whose large body habitus requires the raising of the neck and head to achieve airway alignment.
However, the correct anatomic positioning principle applies to all ages. Specifically, with regard to neonates, a shoulder roll is often placed indiscriminately to put the patient into the now out-dated "sniffing position," usually worsening the view of the airway.
Though this positioning is frequently misused, it can be easily adapted to apply ear to sternal notch positioning to neonates, whose misaligned airway is the result of a large occiput rather than a large torso. In all ages, if you follow these positioning principles, you will improve your view of the airway:
1. Align the ear to the sternal notch
2. Keep the face parallel to the ceiling (do NOT hyperextend the neck, as in the sniffing position)
3. In adults, the head usually needs to be raised (Image 1), while in infants, the torso usually needs to be raised (image 3).


Category: Toxicology
Keywords: tapentadol, nucynta, opioid (PubMed Search)
Posted: 5/12/2011 by Bryan Hayes, PharmD
(Updated: 2/8/2026)
Click here to contact Bryan Hayes, PharmD
Several patients have recently presented with a medication history including tapentadol (Nucynta), the newest opioid formulation. It is approved for treatment of acute moderate-severe pain. Here are some key points:
Category: Neurology
Keywords: pulsatile tinnitus, tinnitus, idiopathic intracranial hypertension, carotid artery diessection, ruptured tympanic membrane (PubMed Search)
Posted: 5/11/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Causes of Pulsatile Tinniitus
Category: Critical Care
Keywords: Clostridium difficile, diarrhea, critical, ICU, sepsis, abdominal pain, vanocmycin,metronidazole, fidaxmicin (PubMed Search)
Posted: 5/10/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Although oral metronidazole is indicated for mild to moderate Clostridium difficile associated diarrhea, oral vancomycin should be considered first-line therapy in critically-ill patients with moderate to severe disease. Vancomycin dosing should begin at 125mg PO q6 and increased to 250mg q6 if poor enteral absorption exists. Consider adding metronidazole IV if either reduced enteral absorption or severe disease exists.
Recently, fidaxomicin has been shown to be non-inferior to oral vancomycin in the treatment of mild to moderate C. difficile. While promising, the study population was not critically-ill and extrapolation should be avoided.
Riddle, D. Clostridium difficile infection in the intensive care unit. Infect Dis Clin North Am. 2009 Sep;23(3):727-43.
Category: Visual Diagnosis
Posted: 5/9/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
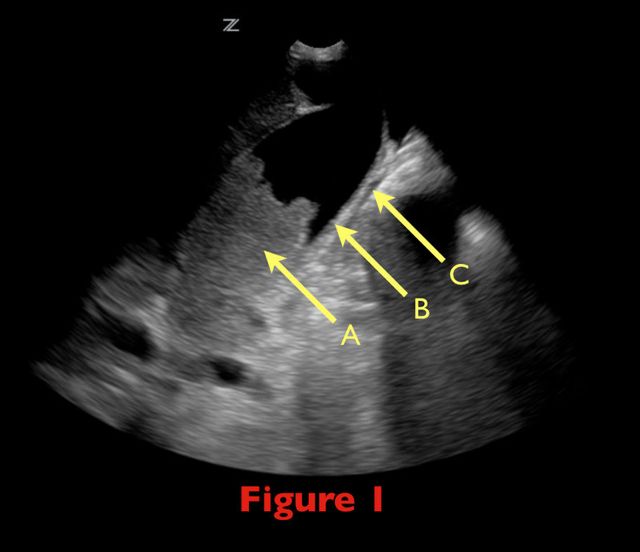
70 yo female from nursing home with fever. RUQ ultrasound is shown below. Diagnosis?

Acalculous Cholecystitis
Acalculous cholecystitis is due to gallbladder (GB) wall ischemia and GB stasis (reduced GB contraction from reduced PO intake)
which all leads to “sludging” (Figure 1; A), thickened GB walls (B), and pericholecystic fluid (C).
Risk factors include critical illness (especially sepsis), acute cholecystitis, total parenteral nutrition, diabetes, and GB dysmotility.
Treatment includes antibiotics covering enteric / biliary pathogens and cholecystectomy (if a surgical candidate) or percutaneous
cholecystostomy if unsuitable for the OR.
Complications include perforation, GB gangrene, and extrabiliary abscess.
Category: Cardiology
Keywords: Beck's triad, tamponade (PubMed Search)
Posted: 5/8/2011 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Beck's triad is well known to many physicians, but here's some simple things you may not have known.
Beck actually described two triads, one for acute and one for chronic tamponade.
The triad for chronic tamponade consists of increased CVP (JVD), ascites, and a small quiet heart (muffled heart sounds).
The triad for acute tamponade consists of JVD hypotension, and muffled heart sounds.
Almost 90% of patients have at least 1 of the signs, but only one-third have all 3. Furthermore, it appears that the simultaneous occurrence of all 3 signs is a very late manifestation of tamponade, usually preceding cardiac arrest.
Harper RJ. Pericardiocentesis. In Clinical Procedures in Emergency Medicine, 5th ed. Roberts JR, Hedges JR, et al. eds. Saunders, Philadelphia, 2010.
Category: Orthopedics
Keywords: Tendon, laceration (PubMed Search)
Posted: 5/7/2011 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Tendon Lacerations:
A reasonable approach to all tendon lacerations is to close the wound and splint in the hand in the position of function until the patient can be seen by a hand surgeon in the next 1-3 days. These injuries do not require immediate surgical repair.
Wheeless Textbook of Orthopaedics. http://www.wheelessonline.com/ortho/extensor_tendon_lacerations
