Category: Critical Care
Posted: 5/26/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Stress-Induced Cardiomyopathy
Boland TA, et al. Stress-induced cardiomyopathy. Crit Care Med 2015; 43:868-93.
Category: Visual Diagnosis
Posted: 5/25/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Do you need to get stuff out of the thorax (like fluid or air) and don't want to place a HUGE chest tube? Consider a pigtail catheter; don't know how to place one? Well check out this video and learn how.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 5/24/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Reperfusion Ventricular Fibrillation
Ventricular fibrillation during reperfusion in STEMI is an infrequent, but serious complication.
Among ~4000 with STEMI between 2007-2012, 71 (1.9%) had reperfusion Vfib.
Increased risk for reperfusion Vfib is associated with: history of MI, aspirin and b-blocker use, Vfib before PCI, left main CAD, inferior MI, symptom-to-balloon time <360 minutes, maximal ST-segment elevation in a single lead >300 μV, and sum of ST-segment deviations in all leads >1,500 μV.
The sum of ST-segment deviations in all leads >1500 μV was an independent predictor of reperfusion Vfib.
Demidova M, Carlson J , et al. Am J Cardiol 2015;115:417e422
Category: Orthopedics
Keywords: shoulder pain, bursitis (PubMed Search)
Posted: 5/23/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Sx: pain to lateral arm, worse with overhead activity and sleeping/lying on arm
Anatomy: Pain generating structures include the rotator cuff, subacromial bursa, labrum and biceps tendon.
http://www.ortho-md.com/images/proceduresImg/SHOULDER2.jpg
Testing: Neer and Hawking tests
https://www.youtube.com/watch?v=U8-yLHQ_JaM
https://www.youtube.com/watch?v=OYK5qL2om-c
Done indepedently, Hawkings is more sensitive, however best to combine both tests.
Imaging: not indicated
Tx: rest, ice, physical therapy (modalities), subacromial steroid injection
Category: Pediatrics
Posted: 5/22/2015 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
1) Fox, S. (2012, August 17). Post-Tonsillectomy Hemorrhage. Retrieved April 8, 2015, from http://pedemmorsels.com/post-
2) Isaacson G. Tonsillectomy Care for the Pediatrician. Pediatrics. 2012; 130(2): pp. 324-334.
3) Perterson J, Losek JD. Post-tonsillectomy hemorrhage and pediatric emergency care. Clin. Pediatr. Jun 2004; 43(5): pp. 445-448.
Category: Toxicology
Keywords: methemoglobinemia, methylene blue (PubMed Search)
Posted: 5/20/2015 by Hong Kim, MD
(Updated: 5/21/2015)
Click here to contact Hong Kim, MD
Methemoglobin (MetHb) is produce when Fe+2 in heme is oxidized to Fe+3 under oxidative stress (caused by mediation and chemicals). MetHb does not bind to oxygen and thus decrease RBC’s O2 carrying capacity.
Among medication, overdose of local anesthesia - benzocaine, dapsone, and phenazopyridine are often implicated. (Table 1)
Think about methemoglobinemia in presence of low pulse oximetry (~85%) with lack of response to supplemental oxygen, cyanosis, dyspnea, etc. (see Table 2 – signs and symptoms of MetHb) in patients who are taking or overdosed on medication listed in Table 1.
Diagnosis: CO-oximetry detects toxin-induced hemoglobinopathies, including COHb and MetHb.
Treatment: Methylene blue (1 mg/kg over 5 min) in symptomatic patients or MetHb level > 25%. Resolution of methemoglobinemia should be noted in 30 – 60 min.
G6PD deficiency: Prevalence in the U.S. is 4-7% with highest prevalence in African American population (11%). Methylene blue causes hemolytic anemia in patients with G6PD deficiency within 24 hours of administration. However, G6PD status is often unknown in ED patients. When caring for patients with known G6PD deficiency and methemoglobinemia, providers must carefully consider the risk and benefit of treating MetHb (including severity of poisoning/MetHb) with methylene blue.
Table 1. Causes of MetHb
| Medication
| Chemicals |
| Benzocaine, Lidocaine, Prilocaine | Aniline dye |
| Dapsone | Chlorobenzene |
| Phenazopyridine | Organic nitrites (e.g. isobutyl nitrite) |
| Nitroglycerin | Naphthalene |
| Nitroprusside | Nitrates (well water contamination) |
| Quinones (Primaquine & Chloroquine) | Nitrites (food preservatives) |
| Sulfonamides | Silver nitrate |
| Nitric oxide | Trinitrotoluene |
| Amyl nitrite |
|
Table 2. Signs and symptoms
| MetHb level (%) | Signs and symptoms |
| 1-3% (normal)
| · None |
| 3-15% | · Low pulse oximetry (<90%) · Gray cutaneous coloration |
| 15-20% | · Chocolate brown blood · Cyanosis |
| 20-50% | · Dizziness, syncope · Dyspnea · Weakness · Headache |
| 50-70% | · CNS depression, coma, seizure · Dysrhythmias · Tachypnea · Metabolic acidosis |
| >70% | · Death · Hypoxic injury |
Category: International EM
Keywords: Diarrhea, infectious diseases, pediatrics, global health (PubMed Search)
Posted: 5/20/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background:
While diarrhea in adults can be inconvenient and briefly debilitating, in children it can be fatal. Globally, diarrheal diseases are the second leading cause of death for children under five.
Clinical types of Diarrhea (with common infectious causes):
Clinical assessment:
*Best indicators of hydration status
Next week: Prevention and Treatment
http://www.who.int/mediacentre/factsheets/fs330/en/
http://www.cdc.gov/healthywater/global/diarrhea-burden.html
http://emedicine.medscape.com/article/906999-clinical#a0217
Category: Critical Care
Keywords: Pulmonary Embolism (PubMed Search)
Posted: 5/19/2015 by John Greenwood, MD
Click here to contact John Greenwood, MD
Advances in Catheter-Directed Therapy for Acute PE - The PERFECT Registry
Earlier this month, initial results from the multicenter PERFECT registry (Pulmonary Embolism Response to Fragmentation, Embolectomy, and Catheter Thrombolysis) were released. In this study, 101 consecutive patients with massive or submassive PE were prospectively enrolled to receive early catheter-directed therapy.
Inclusion criteria:
Therapy provided:
Outcomes: Clinical success (stabilization of hemodynamics, improvement in pulmonary hypertension and/or right heart strain, and survival to discharge) was achieved in 86% of patients with massive PE and 97% of patients with submassive PE. There were no major procedure-related complications or major bleeding events.
Bottom Line: In patients with massive or submassive pulmonary embolism, there is growing evidence that early catheter-directed therapy may become first-line therapy for selected patients.
1. Kuo WT, Banerjee A, Kim PS, et al. Pulmonary Embolism Response to Fragmentation, Embolectomy, and Catheter Thrombolysis (PERFECT): Initial Results from a Prospective Multicenter Registry. Chest. 2015 (ePub April, 2015)
For more Critical Care pearls, follow me on Twitter @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 5/17/2015 by Haney Mallemat, MD
(Updated: 5/19/2015)
Click here to contact Haney Mallemat, MD
5 year-old with no past medical history, complains of a limp and mild left knee pain. No history of trauma. Physical exam is significant for a low-grade fever and is otherwise normal. What’s the diagnosis?
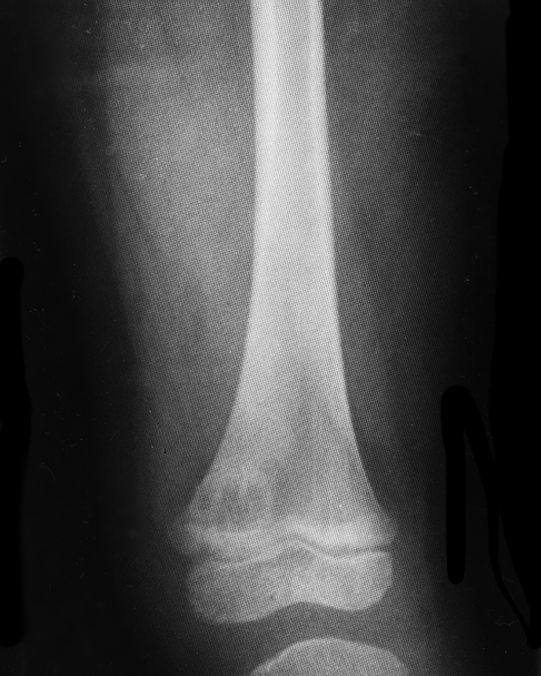
Brodie's abscess a.k.a subacute osteomyelitis
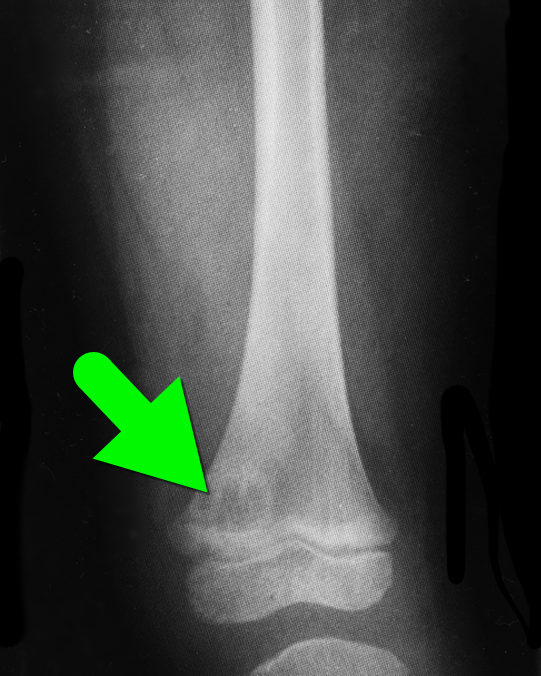
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: tensor fascia latae, hip, pain (PubMed Search)
Posted: 5/16/2015 by Michael Bond, MD
Click here to contact Michael Bond, MD
Tensor Fascia Latae (Iliotibial Band) Pain Syndrome:
Some patients will complain of hip and back pain and can have multiple visits before somebody considers Tensor Fascia Latae Pain Syndrome AKA Iliotibial Band Syndrome.
The tensor fascia latae helps with thigh flexion at the hip, abduction, and medial rotation; and stabilizes the knee laterally
When this muscle/fascia gets tight and overcontracted it will lead to dysfunction of the gluteus and rectus femoralis muscles leading to increased hip pain due to abnormal movement of the joint.
Patients often complain of increased pain with running, especially downhill and exam is notable for local tenderness (approx. 2cm above lateral joint line) & occasional swelling over the distal lateral thigh.
Most patients respond to conservative treatment involving NSAIDs, stretching of the iliotibial band, physical therapy, strengthening of the gluteus medius, and altering their running regimens.
Category: Pediatrics
Keywords: head lice (PubMed Search)
Posted: 5/15/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Lice are spread through direct contact as they crawl. Indirect contact (through brushes or hats) is less likely. One study showed that live lice were found in only 4% of infested volunteers pillowcases.
During an initial infestation, lice can reside on the head for up to 4 to 6 weeks before becoming symptomatic. Therefore, when lice are detected at school, there is no need to send the child home (or to the ED). Children also do not need to be kept out of school while receiving treatment.
Bonus: First line treatment is 1% Permethrin applied on day 0 and 9. The patient should wash their hair first with a non conditioned shampoo, apply Permethrin for 10 minutes and then rinse.
Devore CD and Schutze G. Head Lice. Pediatrics. 2015; 135 (5) e1355 -e1365.
Category: Toxicology
Keywords: Dabigatran, Hemodialysis, Renal Replacement Therapy (PubMed Search)
Posted: 5/14/2015 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Dabigatran is an orally administered, potent, direct thrombin inhibitor approved for the prevention of stroke and systemic embolism in patients with nonvalvular atrial fibrillation, and for the treatment and secondary prevention of venous thromboembolism.
Several pharmacokinectic studies have suggested that dabigatran possesses a number of ideal properties for expedited removal via extracorporeal methods. Dabigatran has low oral bioavailability (3-7%) and is predominantly cleared (80%) by the kidneys. It is not significantly protein bound, low-to-moderate steady state volume of distribution, and has a low molecular weight. All of these attributes make it a candidate for extracorporeal removal. Low protein binding may suggest redistribution into the plasma post extracorporeal removal.
Dabigatran is a substrate for the multidrug efflux transporter P-glycoprotein. Administration of the drug with potent P-glycoprotein inhibitors (ketoconazole, verapamil, amiodarone, quinidine) may significantly increase risk of toxicity, i.e. bleeding.
Most of the current evidence is based on case reports/case series where HD was the primary mode of removal.
Caution: Redistribution effect in plasma dabigatran concentration was also observed in several cases within 20 min to 12 hours post cessation of renal replacement therapy. Other limitations include:
1) Hemodynamic instability such as hypotension that may make initiation of extracoporeal removal difficult
2) Availability of indicators demonstrating effectiveness of extracorporeal removal
3) Amount of time needed to prepare patient to receive extracorporeal therapy
4) Use of extracorporeal removal as a treatment modality has not been prospectively evaluated
Bottom line: Extracorporeal removal may be an option for patients in the setting of life-threatening bleeding but with consideration of several limitations and should not preclude or delay use of other supplemental hemostatic therapies.
Awad NI, Brunetti L, Juurlink DN. Enhanced Elimination of Dabigatran Through Extracorporeal Methods. J Med Toxicol 2015;11:85-95.
Category: Neurology
Keywords: Glasgow Coma Scale, GCS, traumatic brain injury, TBI, survey (PubMed Search)
Posted: 5/13/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Are We Using the Glasgow Coma Scale Reliably?
| Reported by Responders | |
| Patient population in which GCS is used | Traumatic brain injury (96%) Other neurological disorders (78%) |
| Intended purpose of GCS | Classification of severity of injury (51%) Serial evaluation of patient over time (33%) Clinical decision making (44%) Prognostication (17%) |
| Application of stimulus | Both arms and legs (62%) Only arms (37%) |
| Type of stimuli used | Nail bed pressure (57%) Lateral side of finger (22%) Supra-orbital nerve pressure (52%) Trapezius or pectoralis pinch (50%) Sternal rub (53%) Retromandibular stimulation (24%) Earlobe stimulation (16%) |
| Reporting of GCS | Description in words, e.g. no eye opening, no motor (19%) Numerical report, e.g. E1V1M1 (46%) Sum score, e.g. EVM=3 (35%) |
Bottom line: There are variations in the application, assessment, and reporting of the GCS. A standardized approach is needed for it to be a reliable assessment and communication tool.
Reith FCM, Brennan PM, Maas AIR, Teasdale GM. Lack of standardization in the use of the Glasgow Coma Scale: Results of international surveys. J Neurotrauma. 2015; May 7. [Epub ahead of print]
Category: Critical Care
Posted: 5/12/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There is little debate that ultrasound-guided central lines are safer, faster, and more reliable compared to a landmark technique; there is some debate, however, as to whether the short axis (SA) or long axis (LA) approach is the best (see clips below).
The referenced study compared the SA and the LA technique for both the internal jugular (IJ) and subclavian (SC) venous approach. The authors measured number of skin breaks, number of needle redirections, and time to cannulation for each method.
This study demonstrated that the LA technique for subclavian placement had fewer redirections, decreased cannulation time, and fewer posterior wall punctures as compared to the SA. With respect to the IJ approach, the LA was also associated with fewer redirections than the SA view.
Bottom line: Consider the long-axis technique the next time you place an ultrasound guided central line.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/11/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
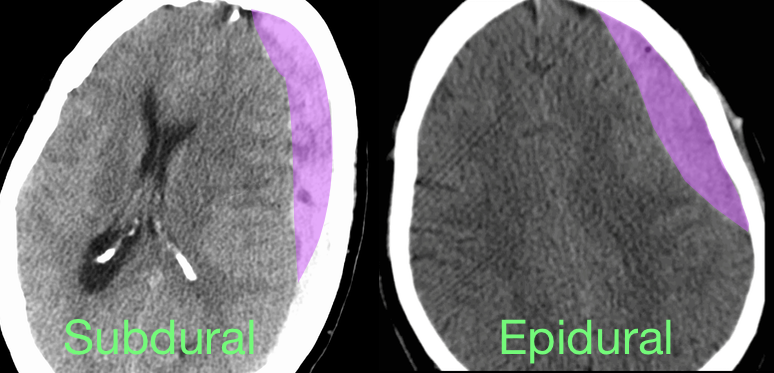
40 year-old male sustains a blunt force injury the left side of his lead. What's the diagnosis and what structure was injured?
Epidural Hematoma with mid-line shift from middle meningeal artery injury; see image below for comparison of subdural and epidural
Epidural hematoma
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 5/10/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Ischemic ECG Findings: Significance of the U-wave
The U-wave is a small deflection immediately following the T-wave, commonly with the same polarity as the T-wave and most prominently seen in precordial leads V2–V3.
Prominent U-waves are most often seen with bradycardia and hypokalemia, but can also be secondary to other electrolyte imbalances and medications.
Typically, T- and U-wave polarities are concordant; discordant U-waves have been identified several hours prior to other ECG changes in acute myocardial infarction.
Some studies note that exercise induced U-wave inversion is highly predictive of CAD; negative U -waves in the precordial leads during exercise had a higher specificity (88% vs. 70%) & positive predictive value (77% vs. 61%) for ischemia than ST-depression.
Reinig et al. 2005 showed that negative concordance of T- and U-waves have poor prognosis & is quite specific for ischemia.
· ECG’s were divided into 3 groups:
o Type 1 T-U discordance (negative T waves + positive U waves)
o Type 2 T-U discordance (positive T waves + negative U waves)
o Negative T-U concordance (both T & U waves negative)
* Significantly higher rate of CAD (88% vs. 58%) (P-value <. 0001) in the negative T-U concordance group
Sovari AA, Farokhi F, et al. Inverted U-wave, a specific electrocardiographic sign of cardiac ischemia. Am J Emerg Med. 2007 Feb;25(2):235-7.
Reinig MG, Harizi R, et al. Spodick Electrocardiographic T- and U-wave discordance. Ann Noninvasive Electrocardiol. 10 (1) (2005), pp. 41–46.
Category: Orthopedics
Keywords: Radiology, orthopedics, shoulder (PubMed Search)
Posted: 5/9/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Posterior Shoulder Dislocations are uncommon (strong supporting structures vs. anterior)
But commonly missed by physicians
Mechanism: Direct blow anterior shoulder/FOOSH with shoulder internally rotated and ADDucted)
May also see with seizure/electric shock (tetanic contraction)
Clinical findings subtle
Shoulder held in ADDuction and internal rotation. Patient unable to externally rotate arm from this position. If habitus allows, anterior shoulder depression/posterior fullness.
Radiology: Decreased overlap between humeral head and glenoid fossa. Proximal humerus fixed in internal rotation looks like a light bulb on a stick.
Y view will show subtle posterior displacement of humeral head (not as dramatic as is in anterior dislocations!)
http://cdn.lifeinthefastlane.com/wp-content/uploads/2009/06/posterior_shoulder_dislocation_005.jpg
http://eorif.com/Shoulderarm/Images/Shoulder-dislocationP1.jpg
Category: Toxicology
Keywords: ketamine, alcohol withdrawal, ethanol (PubMed Search)
Posted: 4/10/2015 by Bryan Hayes, PharmD
(Updated: 5/7/2015)
Click here to contact Bryan Hayes, PharmD
In addition to the down regulation of GABA receptors in chronic ethanol users, there is an upregulation in NMDA receptor subtypes. Although the pathophysiology is much more complex, when ethanol abstinence occurs, there is a shortage of GABA-mediated CNS inhibition and a surplus of glutamate-mediated CNS excitation. If GABA agonists are the mainstay of treatment, why not also target the NMDA receptor? Enter ketamine.
Only one study exists and was published recently.
While the dexmedetomidine studies should not be using reduction in benzodiazepine requirements as an endpoint, it may be acceptable for ketamine since it actually works on the underlying pathophysiology. More studies are needed but it's good to see we’re starting to look at it.
Wong A, et al. Evaluation of adjunctive ketamine to benzodiazepines for management of alcohol withdrawal syndrome. Ann Pharmacother 2015;49(1):14-9. [PMID 25325907]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Death, communicable diseases, noncommunicable diseases (PubMed Search)
Posted: 5/6/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Introduction:
There were approximately 56 million deaths worldwide in 2012. The causes of death vary significantly based upon the income level of the country.
High-income Countries:
Low-income Countries:
Bottom Line:
Acute care services in the US and high-income countries need to acknowledge the growing number of individuals with chronic diseases and the rapidly growing elderly population. In low-income countries, acute care services still need to primarily address maternal/child infections and problems as well as infectious diseases.
www.who.int. Fact sheet- Death: Top 10 causes
Category: Critical Care
Keywords: thoracentesis, pleural effusion, critical care (PubMed Search)
Posted: 5/4/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Safety of Thoracentesis
Results after 24 hours of followup post-procedure
Other interesting points:
Bottom line: Use your ultrasound to direct your tap and dont take out more than 1500 mL routinely
Ault MJ et al. Thoracentesis outcomes: a 12-year experience. Thorax 2015;70:127-132.
