Category: Cardiology
Posted: 12/28/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Holiday Heart
- Holiday heart commonly refers to alcohol use and rhythm disturbances, particularly supraventricular tachydysrhythmias.
- The most common rhythm disorder is atrial fibrillation (AF), which usually converts to normal sinus rhythm within 24 hours and antiarrhythmic therapy is typically not indicated.
- Analyses of ECGs in patients who have consumed a large quantity of alcohol show prolongation of the PR, QRS, and QT intervals.
- 2014 AHA/ACC/HRS updated guidelines for nonvalvular AF utilize the CHA2DS2-VASc (congestive heart failure, hypertension, age ≥75 years [doubled], diabetes mellitus, prior stroke or TIA or thromboembolism [doubled], vascular disease, age 65 to 74 years, and sex category) score for assessment of stroke risk.
Tonelo D, Providência R, Gonçalves L. Holiday heart syndrome revisited after 34 years. Arq Bras Cardiol. Aug 2013;101(2):183-9.
2014 AHA/ACC/HRS Guideline for the Management of Patients with Atrial Fibrillation: Executive Summary. JACC Vol 64, Issue 21, Dec 2014.
Category: Orthopedics
Keywords: knee dislocation, vascular and nerve injury, vascular emergency (PubMed Search)
Posted: 12/26/2014 by Brian Corwell, MD
(Updated: 12/27/2014)
Click here to contact Brian Corwell, MD
Knee Dislocation
Following reduction and immobilization, a thorough vascular assessment should follow. Any signs of vascular injury should prompt immediate vascular consultation (pallor, absent or diminished pulses)
1) Palpate popliteal and distal pulses
2) Measure ankle-brachial index (*ABI) (<0.9 = abnormal)
3) Duplex ultrasound (if available)
*ABI ratio of SBP in lower (DP/PT) and upper (brachial) extremities.
**Evaluation is often institutional specific. Discuss with your consultants.
A) If strong pulses normal ABI and normal u/s admit patient for observation with serial vascular examinations.
B) If the limb is still well perfused but the pulses are asymmetric or ABI is abnormal or US is abnormal then consult vascular surgery and obtain arteriogram (expanding role for CTA here).
C) If pulses are weak or absent or distal signs of ischemic limb then obtain emergent vascular consultation for surgical repair.
Category: Pediatrics
Posted: 12/27/2014 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Cyanotic (right to left shunt) Congenital Heart Disease (CHD) lesions can be easily remembered with the 1,2,3,4,5 method.
1- Truncus Arteriosis (ONE trunk)
2- Transposition of the Great Vessels (TWO vessels flipped)
3- TRIcuspid Atresia
4-TETRAlogy of Fallot
5- Total Anomolous Pulmonary Venous Return (TAPVR=5 words/letters)
A few other important DUCTAL-DEPENDENT lesions: Coarctation of the Aorta, Hypoplastic Left Heart Syndrome, and Pulmonary Atresia.
Patients present to the emergency department within the first week of life in severe distress, including hypoxia, tachypnea, and hypotension. The above cyanotic CHD all reflect DUCTAL-DEPENDENT lesions, meaning they need a widely open PDA (which closes in the first week of life) to maintain sufficient oxygenation for viability.
These patients will not survive without timely intervention with prostaglandin (PGE1), so be sure to initiate this life-saving medication as soon as possible! Side effects include apnea…be prepared to intubate your neonate!
Category: Neurology
Keywords: delirium, geriatric, elderly, pitfall (PubMed Search)
Posted: 12/25/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Delirium has long been recognized as a common disorder of the geriatric ED population (seen in up to 20% of patients above the age of 65 years), but how good are we at detecting it?
Studies show that the diagnosis of delirium is made in the ED in only 11-46% of patients, which means that more than half go undiagnosed. The problem is, the risk of death at 3 months increases by 11% for every 48 hours of delirium the patient experiences, and so does their length of stay and functional decline. It is mostly missed in patients who have a baseline cognitive dysfunction, such as dementia.
So what can we do about that?
Treat delirium as a neurolgical emergency; be vigilant about diagnosing it and treating it. There are a lot of neurocognitive tests that can be used for diagnosis (such as the mini-mental status exam), but they are usually too cumbersome to use in an ED setting. The CAM (Confusion Assessment Method) has been extensively studied and has a sensitivity and specifity of about 95% to diagnose delirium. It includes the acuity of onset, fluctuant course, inattention (the hallmark), disorganized thinking and/or altered level of consciousness.
Bottom Line? Don't forget to screen your elderly patients for delirium and treat them accordingly!
1. Wilber ST, Han JH. Altered Mental Status in the Elderly. Geriatric Emergency Medicine Principles and Practice. Edited by Kahn JH, Maguaran Jr BG, Olshaker JS. New York: Cambridge University Press; 2014: 102-113
2. Barron EA, Holmes J. Delirium within the emergency Care setting, occurence and detection: a systematic review. EMJ 2013; 30(4) 263-268
3. Wei LA, BA, Fearing MA et al. The Confusion Assessment Method: A Systematic Review of Current Usage J Am Geriatr Soc 56:823 830, 2008
Category: Critical Care
Posted: 12/23/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Treating ischemic strokes with interventional therapies (e.g., clot retrievers, stents, intra-arterial tPA, etc.) is nothing new, but there has never been a randomized control trial demonstrating benefit until recently.
The prospective MR CLEAN trial evaluated whether interventional therapies (i.e., either mechanical intervention or intra-arterial tPA) would confer benefit; patients were included if there was an acute occlusion within the proximal intracranial portion of the anterior cerebral circulation.
90% of patients received alteplase prior to randomization; there were 233 patients in the intervention group (alteplase + intraarterial intervention) and 267 patients in the usual care care arm (alteplase only); all patients were treated within 6 hours of symptoms onset
The primary outcome was functional independence at 90 days; an absolute difference of 13.5 percentage points favoring the intervention group was found. There were no significant differences in mortality or symptomatic intracerebral hemorrhage.
Despite these exciting results, we must pause and ask why this was this the first randomized trial demonstrating benefit when previous trials could not? Here are three blogs posts that deep dive this question and raise even more questions:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/21/2014 by Haney Mallemat, MD
(Updated: 12/23/2014)
Click here to contact Haney Mallemat, MD
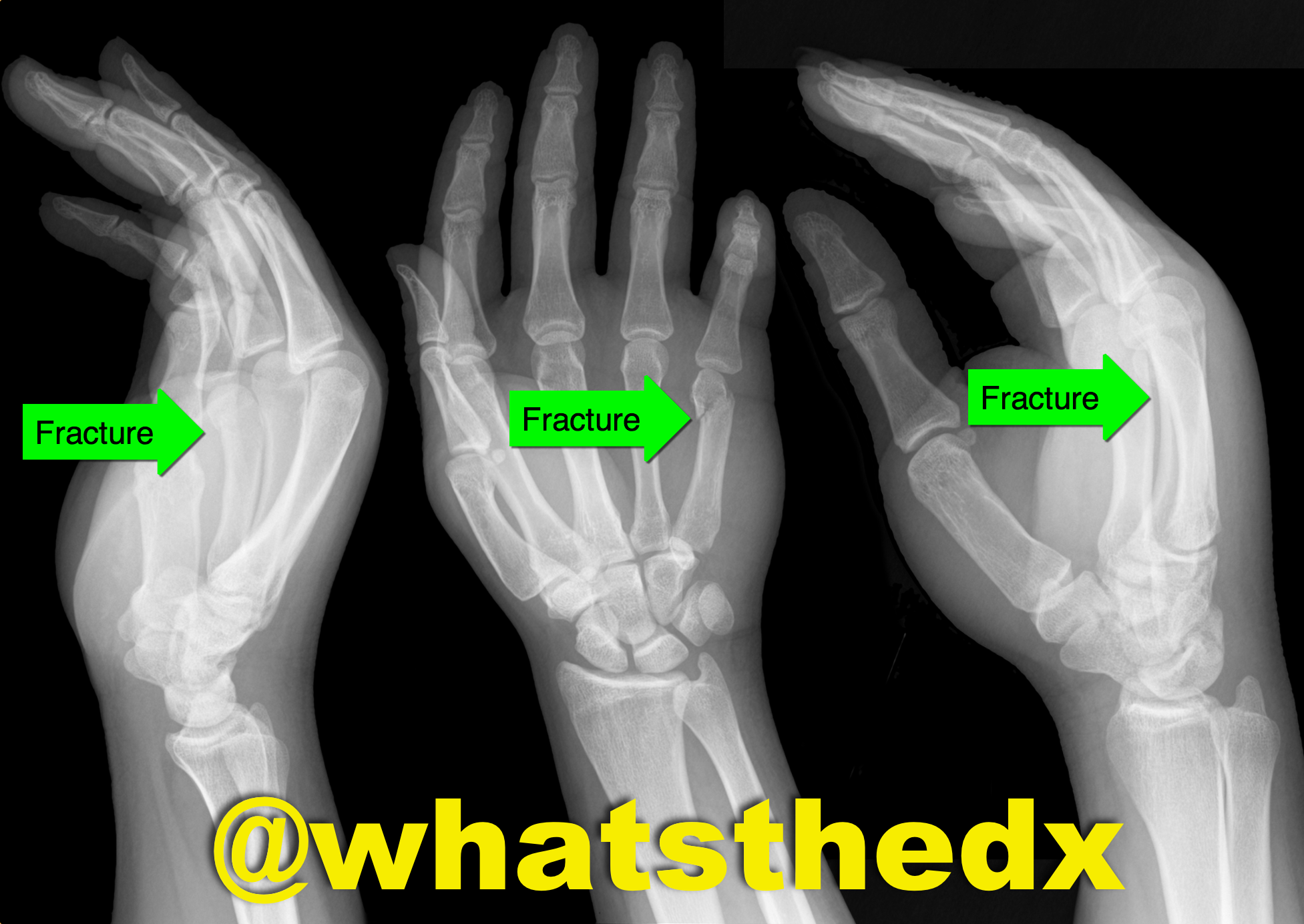
Hand pain following fist versus face. What's the diagnosis and what nerve block would you use?

Boxer's fracture. Read more here.
Pain control can be achieved with an ulnar nerve block (e.g., reducation if if angulated). A video for the technique using ultrasound can be found here.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Brugada (PubMed Search)
Posted: 12/21/2014 by Semhar Tewelde, MD
(Updated: 1/19/2015)
Click here to contact Semhar Tewelde, MD
Brugada Syndrome
Brugada syndrome is an inherited arrhythmogenic channelopathy described by ST-segment elevation in the right precordial leads and an increased risk of sudden cardiac death.
There are 3 electrocardiographic patterns:
Type 1 – Coved morphology w/ST-elevation >2 mm, followed by a negative T wave in at least 1 right precordial lead
Type 2 - Saddleback morphology w/ST-elevation >2mm, with a positive or biphasic T wave
Type 3 - Either coved, or saddleback morphology with <2mm ST-elevation
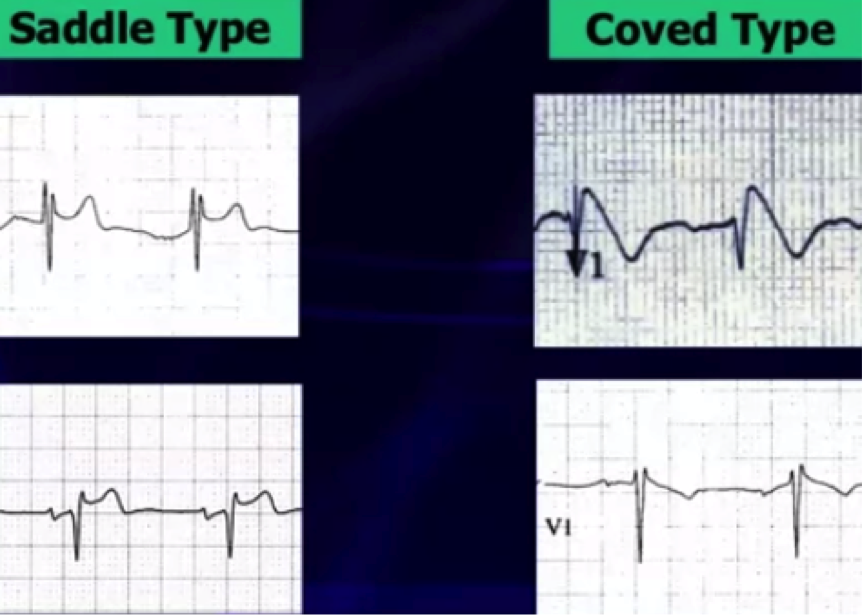
Type 1 pattern is often underestimated because of its sporadic/fluctuating appearance on ECG, which can be either spontaneously occurring or drug-induced (drug-induced variant has a more favorable prognosis).
Fever has been a well-documented culprit in unmasking Brugada pattern by increasing the sodium channel dysfunction & accelerating the late sodium current inactivation.
A recent study in a large population of patients with type 1 Brugada attempted to identify other patterns unmasking Brugada using 24-hour holter monitoring. * There is now evidence that there is a higher prevalence of type 1 Brugada pattern from 12pm-6pm & unmasking by fast and a large meal, showing influence by glucose intake and insulin levels.
Cerrato N, Giustetto C, et al. Prevalence of Type 1 Brugada Electrocardiographic Pattern Evaluated by Twelve-Lead Twenty-Four-Hour Holter Monitoring. The American Journal of Cardiology.Vol 115, Issue 1, 1 Jan. 2015, pgs. 52-56.
Category: Pediatrics
Keywords: Bronchiolitis, wheezing (PubMed Search)
Posted: 12/19/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Now that respiratory season is upon us, we are faced with an increasing number of bronchiolitis children. The updated clinical practice guidelines for managing these kids were recently published and emphasize supportive care only.
Some of the key points:
-When clinicians diagnose bronchiolitis on the basis of history and physical examination, radiographic or laboratory studies should not be obtained routinely.
-Medications such as albuterol, nebulized epinephrine or steroids should not be administered routinely in children with a diagnosis of bronchiolitis.
-Nebulized hypertonic saline should not be administered to infants with a diagnosis of bronchiolitis in the emergency department
-Clinicians may choose not to administer supplemental oxygen if the oxyhemoglobin saturation exceeds 90% in infants and children with a diagnosis of bronchiolitis
-Clinicians may choose not to use continuous pulse oximetry for infants and children with a diagnosis of bronchiolitis.
Check out the full guidelines for the quality of evidence and rational behind these recommendations.
The bottom line is that not much really works, and we just need to support their respiratory effort and ensure hydration.
Ralston et al. Clinical Practice Guideline: The diagnosis, Management and Prevention of Bronchiolitis. Pediatrics 2014; 134: e1474-e1502.
Category: Toxicology
Keywords: cocaine chest pain, "unopposed alpha effect," beta-blocker (PubMed Search)
Posted: 12/18/2014 by Hong Kim, MD
(Updated: 2/8/2026)
Click here to contact Hong Kim, MD
It is believed that administration of beta-blocker administration in patients with cocaine chest pain will produced increased vasoconstriction due to “unopposed alpha effect.”
Several retrospective studies on the use of beta-blocker in patients with cocaine-induced chest pain concluded the use of beta-blocker to be safe.
So is the unopposed alpha effect just a theory?
Lange RA et al. 1990 Ann Internal Med
Design: randomized, double-blind, placebo controlled trial.
30 (38- 68 years old) patients undergoing cardiac catherization for chest pain evaluation were studied.
Cocaine (intranasal administration) resulted in:
Administration of propranolol (intracoronary infusion) resulted in additional:
Complete coronary occlusion observed in 1 patient with ST elevation
Epicardial coronary arterial segment constriction >10% in 5 patients.
Bottom Line: Lange RA et al. 1990 demonstrates that the “unopposed alpha effect” does occur in coronary artery when beta-blocker is administered in a setting of acute cocaine exposure. Overall, the use of beta-blocker in the ED management of cocaine-induce acute chest pain is not a prudent option. It is unknown if the cocaine dose, last use of cocaine (days), or CAD history influence the “safety” of beta-blocker initiation/use during inpatient hospitalization.
Lange RA, Cigarroa RG, et al. Pontetiation of cocaine-induced coronary vasoconstriction by beta-adrenergic blockade. Ann Internal Med 1990;112:897-903
Category: International EM
Keywords: Influenza, 2014, CDC (PubMed Search)
Posted: 12/18/2014 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Background: As discussed previously, influenza (flu) is a common respiratory disease that causes significant morbidity and mortality worldwide (see pearl from October 1. 2014). We are now in the midst of the current flu season.
Current Update: This year’s vaccine was only a partial match (<50%) for the current influenza A (H3N2) circulating virus, so there is a significant potential for a “bad” flu season with widespread disease and severe illness. Currently, influenza is now widespread throughout the US, with some states reporting more activity than others. The CDC has a weekly surveillance map that highlights current disease spread.
Bottom Line:
CDC Weekly Influenza Map: http://www.cdc.gov/flu/weekly/usmap.htm
CDC 2014-2015 Flu Season Webpage: http://www.cdc.gov/flu/about/season/index.htm
Category: Critical Care
Keywords: influenza, tamiflu, (PubMed Search)
Posted: 12/16/2014 by Feras Khan, MD
Click here to contact Feras Khan, MD
How does it present?
Who cares…I got my vaccine! Does the vaccine work this year?
Can I test for this?
The CDC is recommending treatment...wait I thought we were done with Tamiflu?
Who is at risk/who deserves consideration for treatment?
Pearls of treatment
What are the side effects of anti-viral agents?
http://www.cdc.gov/flu/index.htm
Category: Visual Diagnosis
Posted: 12/15/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A patient is intubated for respiratory failure and the post-intubation CXR is shown on the left. 30 minutes later the patient desaturates and another CXR is obtained (the one on the right). What’s the diagnosis and what should you do?
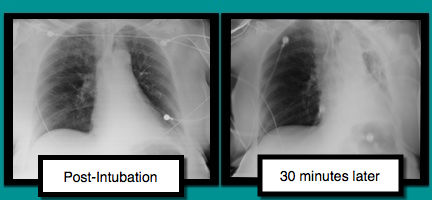
Mucus plug
There are several conditions to consider when patients are having difficultly being ventilated. The approach to such a patient can be remembered with a mnemonic found here.
In this case, conditions to consider are:
Treating mucus plugs can usually be treated as follows:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 12/14/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Not So Benign: Benign early repolarization (BER) effects in STEMI
- Benign early repolarization (BER) has been associated with increased risk of sudden cardiac death and ventricular fibrillation (VF) in patients with and without structural heart disease.
- Acute STEMI is associated with high incidence of ventricular arrhythmias and the most frequent cause of sudden cardiac death in the adult population.
- BER has been associated with arrhythmogenicity, however the prognostic importance of this ECG finding in patients with STEMI has not been well elucidated.
- In a recent prospective study of STEMI patients, BER was associated with higher rates of in-hospital ventricular arrhythmias and mortality; It is an independent predictor of long-term mortality beyond well-known other parameters.
Ozcan K, et al. Presence of early repolarization on admission electrocardiography is associated with long-term mortality and MACE in patients with STEMI undergoing primary percutaneous intervention. Journal of Cardiology, Volume 64, Issue 3, September 2014, Pages 162-163.
Category: Pediatrics
Posted: 12/13/2014 by Rose Chasm, MD
(Updated: 2/8/2026)
Click here to contact Rose Chasm, MD
NMS Pediatrics. Lippincott Williams and Wilkins. 4th Edition. Paul Dworkin editor.
Category: Toxicology
Keywords: cocaine, chest pain, beta blocker (PubMed Search)
Posted: 12/1/2014 by Bryan Hayes, PharmD
(Updated: 12/11/2014)
Click here to contact Bryan Hayes, PharmD
Should beta blockers be withheld in cocaine-chest pain patients?
A new study retrospectively compared patients who received beta blockers as an inpatient to those who did not. Even though the beta blocker group had higher risk clinical characteristics, there was no difference in the composite primary end point of myocardial infarction, stroke, ventricular arrhythmia, or all-cause mortality within 24 hours of beta blocker use.
Important Limitations
The potentially dangerous interaction between beta blockers and cocaine is likely a much larger issue in patients with very recent cocaine use in the setting of a catecholamine surge. A retrospective analysis likely doesn't include those patients.
Application to Clinical Practice
While this study doesn't answer the question about beta blocker use in acute cocaine toxicity, it does provide some reassurance about the safety of beta blockers given for cocaine-related chest pain.
Fanari Z, et al. Comparison of in-hospital outcomes for beta-blocker use versus non-beta blocker use in patients presenting with cocaine-associated chest pain. Am J Cardiol 2014;113(11):1802-6. [PMID 24742472]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: clinical decision support, clinical decision rules, head CT, mild traumatic brain injury (PubMed Search)
Posted: 12/10/2014 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Does clinical decision support help reduce head CT utilization in mild traumatic brain injury related ED visits?
Are we utilizing clinical decision rules adequately to help us appropriately select patients for CT imaging?
Can clinical decision support (CDS) help us reduce head CT utilization in mTBI related ED visits?
Take Home Point:
Clinical decision support may be a useful tool to help reduce CT utilization in mild TBI related ED visits.
Ip IK, Raja AS, Gupta A, et al. Impact of clinical decision support on head CT use in patients with mild traumatic brain injury in the emergency department. Am J Emerg Med 2014; Nov 13 [epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 12/9/2014 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
The Critically Ill Patient with Ebola Virus Disease
Fowler RA, et al. Caring for Critically Ill Patients with Ebola Virus Disease. Am J Resp Crit Care Med 2014; 190:733-37.
Category: Visual Diagnosis
Posted: 12/8/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient was found in a house fire and was given a certain medication in the Emergency Room. The patient’s urine turned this color (red), what’s the diagnosis?

Hydroxocobalamin (i.e., Cyanokit)
Cyanide toxicity
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 12/7/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Predictors of Cardiac Rupture After AMI
- In the era of revascularization and aggressive cardiac care there has been a continual decline in acute myocardial infarction (AMI) mortality rates; however one of the most deadly complications, cardiac rupture (left ventricular free wall, ventricular septum, or papillary muscle rupture), still remains relatively stable.
- Cardiac rupture is an increasingly more frequent cause of death during AMI, thus a recent study retrospectively assessed the clinical and morphologic variables in those with and without cardiac rupture that were hospitalized for AMI.
- Cardiac rupture overwhelmingly complicates a first AMI.
- Cardiac rupture occurs most often in patients with an immense quantity of cardiac adipose tissue, the size of the left ventricular cavity is typically normal, and the area of the infarct is small.
- Heart failure patients with prior AMI have healed scar tissue and are at nominal risk of complications such as rupture if a subsequent AMI occurs.
Roberts W, et al. Commonalities of Cardiac Rupture (Left Ventricular Free Wall or Ventricular Septum or Papillary Muscle) During Acute Myocardial Infarction Secondary to Atherosclerotic Coronary Artery Disease. The American Journal of Cardiology. Volume 115, Issue 1, Pages 125-140 (1 January 2015).
Category: Pharmacology & Therapeutics
Keywords: antibiotic, IV, diarrhea (PubMed Search)
Posted: 11/25/2014 by Bryan Hayes, PharmD
(Updated: 12/6/2014)
Click here to contact Bryan Hayes, PharmD
Many of the oral antibiotics prescribed in the ED have good bioavailability. So, a one-time IV dose before discharge generally won't provide much benefit.
In fact, a new prospective study found that a one-time IV antibiotic dose before ED discharge was associated with higher rates of antibiotic-associated diarrhea and Clostridium difficile infection. [1] One-time doses of vancomycin for SSTI before ED discharge are also not recommended (see Academic Life in EM post).
Bottom Line
Though there are a few exceptions, if a patient has a working gut, an IV dose of antibiotics before ED discharge is generally not recommended and may cause increased adverse effects. An oral dose is just fine.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
