Category: Orthopedics
Keywords: Sciatica, radiculopathy, imaging (PubMed Search)
Posted: 9/19/2014 by Brian Corwell, MD
(Updated: 9/27/2014)
Click here to contact Brian Corwell, MD
Back pain with radiculopathy can be very distressing to a patient and they have heard from their medically savvy neighbor that a MRI is the way to go. Now, armed with this knowledge, they are in your ED with earplugs in hand...
A few minutes of reassurance and education can save in both cost and ED throughput.
In one study researchers performed MRIs on asymtomatic adult patients.
Almost two-thirds (64%) had abnormal discs
Just over half (52%) had bulging discs
Almost a third (31%) had disc protrusions
Further, finding a bulging disc already suggested by your history and physical examination does not change management. The majority of these patients improve with conservative treatment within four to to six weeks.
Restrict ED MRI use for the evaluation of suspected cauda equina, epidural abscess and spinal cord compression.
Category: Pediatrics
Keywords: E. coli, O0157:H7, hematochezia, diarrhea (PubMed Search)
Posted: 9/26/2014 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
There are numerous different causes of pediatric hemorrhagic diarrhea. Consider a pediatric patient with bloody diarrhea as being at risk for developing hemolytic uremic syndrome. Most cases of hemolytic uremic syndrome are caused by O157:H7 strains of E Coli that release Shiga-like toxin from the gut. Systemic release of the toxin causes microvascular thromboses in the renal microvasculature. The characteristic microangiopathic hemolysis results with anemia, thrombocytopenia and peripheral schistocytes seen on laboratory studies, in addition to acute renal failure.
Antibiotics have been controversial in the treatment of pediatric hemorrhagic diarrhea due to concern that they worsen toxin release from children infected with E Coli O157:H7 and thus increase the risk of developing hemolytic uremic syndrome. Numerous previous studies have provided conflicting data regarding the true risk (1). A recent prospective study showed antibiotic treatment increases the risk (2). Most recommendations warn against using antibiotics to treat pediatric hemorrhagic diarrhea unless the patient is septic.
Bottom line: Avoid treating pediatric hemorrhagic diarrhea with antibiotics
References:
1. Systematic review: are antibiotics detrimental or beneficial for the treatment of patients with Escherichia coli O157:H7 infection? Alimentary Pharmacology & Therapeutics. Volume 24, Issue 5, pages 731–742, September 2006
2. Risk factors for the hemolytic uremic syndrome in children infected with Escherichia coli O157:H7: a multivariable analysis. Clin Infect Dis. 2012 Jul;55(1):33-41. doi: 10.1093/cid/cis299. Epub 2012 Mar 19.
Category: Toxicology
Keywords: disulfiram (PubMed Search)
Posted: 9/25/2014 by Fermin Barrueto
(Updated: 2/7/2026)
Click here to contact Fermin Barrueto
When you prescribe certain medications, it may require some further instructions to avoid ethanol or a disulfiram like reaction (nausea, vomiting, flushing) may occur. Keep this short list in your brain:
1) Particular cephalosporins: cefotetan is a the one more likely
2) Nitrofurantoin
3) Sulfonylureas: chlorpropamide and tolbutamide
4) Metronidazole
5) Trimethoprim-sulfamethoxazole
Goldfranks 8th Edition, p1179
Category: Neurology
Keywords: meningitis, clinical exam (PubMed Search)
Posted: 9/25/2014 by Danya Khoujah, MBBS
(Updated: 2/7/2026)
Click here to contact Danya Khoujah, MBBS
Jolt accentuation, the exacerbation of a headache with horizontal rotation of the neck, or shaking of the stretcher in the less cooperative patient, has been promoted for the past few years as the "go-to" test to assess for meningeal irritation in patients with headache. Previous studies have quoted sensitivities as high as 97.1%. (1)
A new prospective study in AJEM challenges this belief by looking at a total of 230 patients with headaches and subsequent LPs. 197 of them had the jolt accentuation test done, which had a sensitivity of only 21% for pleocytosis (defined as greater than or equal to 5 cells/high power field in the 4th CSF tube). Kernig's and Brudzinski's signs both did even more poorly, with a sensitivity of 2% each. (2)
(1) Uchihara T. Jolt accentuation of headache: the most sensitive sign of CSF pleocytosis. Headache. 1991 Mar;31(3):167-71
(2) Nakao JH et al. Jolt accentuation of headache and other clinical signs: poor predictors of meningitis in adults. Am J Emerg Med. 2014 Jan;32(1):24-8
Category: Critical Care
Keywords: massive transfusion, bleeding (PubMed Search)
Posted: 9/23/2014 by Feras Khan, MD
(Updated: 2/7/2026)
Click here to contact Feras Khan, MD
What is a massive transfusion?
When would I use this?
Indications:
-Systolic Blood pressure < 100
-Unable to obtain blood pressure
AND
-Penetrating torso trauma
-Positive FAST
-External blood loss
-Plans to go to the OR
How do I give it?
Does this apply for just traumatic bleeding?
Are there other agents I can use?
What am I trying to do with this protocol?
Murthi SB, Stansbury LG, Dutton RP, et al. TRAnsfusion medicine in trauma patients: an update. Expert Rev Hematol. 2011 Oct;4(5):527-37.
Hess JR, et al. The coagulopathy of trauma: a review of mechanisms. J Trauma. 2008 Oct; 65(4):748-54.
University of Maryland SHOCK Trauma Massive Transfusion Protocol. 2011.
Category: Pediatrics
Keywords: Macklin Phenomenon, asthma, pneumomediastinum (PubMed Search)
Posted: 9/22/2014 by Ashley Strobel, MD
Click here to contact Ashley Strobel, MD
16 yo M with pleuritic right upper chest pain that started today. He is suffering from an asthma exacerbation currently in the setting of URI with cough. He is afebrile, tachycardic to 140-150s, respiratory rate 20, and sats 98% on room air. ECG was performed which incidentally diagnosed this patient WPW and he went for ablation as an outpatient. His chest x-ray showed:
Besides a bad day, what do we call this chest x-ray finding?
Macklin Phenomenon
-asthma exacerbation rupture of the alveoli causing pneumomediastinum
-typically a young man
-most common chief complaint is chest pain
Physical Exam: Hamman’s sign may be present (crackle with heartbeat) or subcutaneous emphysema
Etiology: Esophagus, lungs, or bronchial tree
Rupture of alveoli: asthma exacerbation (bronchial hyper-reactivity/constriction), barotrauma, valsalva maneuvers (lifting, childbirth), deep respiratory maneuvers/Valsalva (strenuous exercise or FVC breathing), drug use (crack cocaine causing bronchial constriction, marijuana), vomiting, blunt thoracic/abdominal trauma, scuba diving with rapid ascent
Aerodigestive tract injuries: bronchoscopy tracheobronchial injuries, laryngeal fx, bronchial fx, tracheal neoplasm, esophageal injuries (Boerhaave syndrome, paripartum, asthma exacerbation, esophageal neoplasm)
Extension from neck: head/neck sx, RPA/PTA, dental abscess/extractions
Extension from RP/chest wall: rupture RP hollow viscus
Management:
-self -limited
-treat underlying condition
-swallow study for all cases following emesis to rule out Boerhaave’s syndrome
-no repeat CXR, advance diet as tolerated, 23 hour observation
-Al-Mufarrei, et al suggest without trauma, pleural effusion, hemodynamic instability, pneumoperitoneum, or severe vomiting, the finding of spontaneous pneumomediastinum (with or without Meckler’s triad of esophageal rupture: vomiting, lower chest pain, and cervical subcutaneous emphysema after overindulgence) usually leads to unnecessary radiologic investigations, dietary restriction, and antibiotic administration
-surgery for decompression
Gray JM and Hanson GC. Mediastinal emphysema: aetiology, diagnosis, and treatment. Thorax. 1966; 21: 325-332.
Al-Mufarrej F, Badar J, Gharagozloo F, Tempesta B, Strother E, Margolis M. Spontaneous pneumomediastinum: diagnostic and therapeutic intervnetions. Journal of Cardiothoracic Surgery. November 2008; 3: 59.
Category: Orthopedics
Keywords: Tendon, Laceration, Repair (PubMed Search)
Posted: 9/19/2014 by Michael Bond, MD
(Updated: 9/20/2014)
Click here to contact Michael Bond, MD
Tendon Lacerations:
A reasonable approach to all tendon lacerations is to loosly reapproximate the wound and splint the hand in the position of function until the patient can be seen by a hand surgeon in the next 1-3 days. These injuries do not require immediate surgical repair, and with the high rate of complications it is probably best to discuss with your hand surgeon before attempting a repair.
Wheeless Textbook of Orthopaedics. http://www.wheelessonline.com/ortho/extensor_tendon_lacerations
Category: Pediatrics
Keywords: cervical spine, pediatrics, NEXUS (PubMed Search)
Posted: 9/19/2014 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
The NEXUS criteria is widely applied to adults who present with neck pain due to trauma. While this study did include about 2000 pediatric patients, there were not enough young children to draw definitive conclusions. For more information on the evaluation of the cervical spine, see Dr. Rice's pearl from 9/7/12. A 2003 study piloted an algorithm for cervical spine clearance in children < 8 years.
Patients were spine immobilized if: unconscious, abnormal neurological exam, history of transient neurological symptoms, significant mechanism of injury, neck pain, focal neck tenderness or inability to assess based on distracting injury (extremity or facial fractures, open wound, thoracic injuries, or abdominal injuries), physical exam findings of neck trauma, unreliable exam due to substance abuse, significant trauma to the head or face, or inconsolable children.
When the 2 pathways (see attached) were implemented, there was a decrease in time to cervical spine clearance. There were no missed injuries in the study period prior to implementation of the pathway or once it was implemented. There was no significant difference in the amount of xrays, CT scans or MRIs.
Lee S, Sena M, Greenholtz, S, Fledderman M. A Multidisciplinary Approach to the Development of a Cervical Spine Clearance Protocol: Process, Rationale, and Initial Results. Journal of Pediatric Surgery 2003; 38 (3): 358-362.
Category: Toxicology
Keywords: ciguatera, scromboid, tetrodotoxin (PubMed Search)
Posted: 9/18/2014 by Hong Kim, MD
Click here to contact Hong Kim, MD
Food poisoning can occur with many different food groups/items, as well as how the food is prepared, handled or stored.
There are three specific “food poisonings” associated with fish consumption can cause serious toxicity/illness beyond GI symptoms: Ciguatera, Scrombroid, tetrodotoxin (puffer fish)
Ciguatera
Symptoms:
May progress to develop…
Treatment: supportive care and mannitol in presence of severe neurologic symptoms (limited evidence).
Scrombroid
Symptoms:
Tx: H1/H2 blockers and supportive care
Serious reactions: treat like allergic/anaphylactic reaction
Tetrodotoxin
Symptoms:
Treatment: supportive care and intubated if needed.
Category: International EM
Keywords: deep venous thrombosis, plane travel, blood clots (PubMed Search)
Posted: 9/16/2014 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 9/17/2014)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
While sitting on an international flight, ever wonder what your risks are for a blood clot?
General Background:
It is estimated that the risk for a deep venous thrombosis (DVT) is 3-12% on a long-haul flight. However, the real incidence is difficult to evaluate, due in part to the lack of consensus about 1) diagnostic tests, and 2) the appropriate time frame to relate a venous thromboembolic event (VTE) to travel.
Risks Factors for VTEs on long-haul flights:
Bottom Line:
http://www.cdc.gov/ncbddd/dvt/travel.html
Gavish I, Brenner B. Air travel and the risk of thromboembolism. Intern Emerg Med 2011 Apr;6(2):113-6.
Category: Critical Care
Posted: 9/16/2014 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Infectious Risks Associated with TTM
Kuchena A, et al. Postcardiac arrest temperature management: infectious risks. Curr Opin Crit Care 2014; 20:507-15.
Category: Visual Diagnosis
Posted: 9/15/2014 by Haney Mallemat, MD
(Updated: 10/1/2014)
Click here to contact Haney Mallemat, MD
Football player complains of sudden foot pain after begin tackled. What’s the diagnosis?

Lisfranc fracture-dislocation
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 9/14/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Optimal Revascularization in Complex Coronary Artery Disease
- A multicenter trial 4,566 patients with NSTEMI, unstable angina, and multi-vessel coronary artery disease were enrolled comparing outcomes of cardiac stenting versus coronary artery bypass.
- Cardiac stenting was associated with improved outcomes and lower mortality in the following subgroups: age >65 years, women, unstable angina, TIMI score >4, and 2 vessel disease.
- Despite high clinical risk patients who underwent cardiac stenting compared to surgical revascularization did better in this prospective registry.
Buszman P, Buszman P, Bochenek A, et al. Comparison of Stenting and Surgical Revascularization Strategy in Non-ST Elevation Acute Coronary Syndromes and Complex Coronary Artery Disease (from the Milestone Registry). JACC Oct 2014 Vol 114, Issue 7, pages 979-987.
Category: Orthopedics
Keywords: back pain, x-ray (PubMed Search)
Posted: 9/13/2014 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Back pain accounts for more than 2.6 million visits
30% of ED patients receive X-rays as part of their evaluation
Imaging can be avoided in a majority of these patients by focusing on high risk (red flags) findings in the history and physical exam.
Patients who can identify a an acute inciting event without direct trauma likely have a MSK source of pain.
Imaging rarely alters management
Attempt to avoid imaging in patients with nonspecific lower back pain of less than 6 weeks duration, with a normal neurologic exam and without high risk findings (fever, cancer, IVDA, bowel or bladder incontinence, age greater than 70, saddle anesthesia, etc)
Patients with radiculopathy (sciatica) and are otherwise similar to the above also do not require emergent imaging
Category: Pediatrics
Posted: 9/12/2014 by Rose Chasm, MD
(Updated: 2/7/2026)
Click here to contact Rose Chasm, MD
Severe Respiratory Illness Associated With Enterovirus D68--Missouri and Illinois, 2014. CDC MMWR. Vol 63. September 2014.
Category: Toxicology
Keywords: digoxin, digoxin-specific antibody fragments, digoxin-Fab (PubMed Search)
Posted: 9/9/2014 by Bryan Hayes, PharmD
(Updated: 9/11/2014)
Click here to contact Bryan Hayes, PharmD
Digoxin-specific antibody fragments (Fab) are safe and indicated in all patients with life-threatening dysrhythmias and an elevated digoxin concentration. However, full neutralizing doses of digoxin-Fab are expensive and may not be required (not to mention cumbersome to calculate).
Based on pharmacokinetic modeling and published data, a new review suggests a simpler, more stream-lined dosing scheme as follows:
In imminent cardiac arrest, it may be justified to give a full neutralizing dose of digoxin-Fab.
In acute poisoning, a bolus of 80 mg (2 vials), repeat if necessary, titrated against clinical effect, is likely to achieve equivalent benefits with much lower total doses.
With chronic poisoning, it may be simplest to give 40 mg (1 vial) at a time and repeat after 60 min if there is no response.
Chan BS, et al. Digoxin-specific antibody fragments in the treatment of digoxin toxicity. Clin Toxicol 2014;52:824-36. [PMID 25089630]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: blood pressure, stroke (PubMed Search)
Posted: 9/11/2014 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Why is everyone obsessed about blood pressure management in stroke?
Greater than 60% of patients with stroke have elevated blood pressure, and 15% have a systolic blood pressure (SBP) greater than184 mmHg. That is more common in hemorrhagic stroke than ischemic stroke.
Whether it's an acute hypertensive response or a premorbid uncontrolled hypertension, it is likely to negatively affect the clinical course and neurological outcome.
Below is a suumary of the current guidelines for blood pressure management of stroke subtypes; for a more detailed summary of the guidelines, refer to the original article (below)
Ischemic stroke:
Lytic patients have a target SBP of <185mmHg, whereas nonlytic patients have a higher SBP target of <220mmHg
Hemorrhagic Stroke:
Non-aneurysmal hemorrhage patients with a SBP >180mmHg have a target SBP of <160 mmHg, whereas if their SBP was 150-220 mmHg then lowering it to 140 mmHg is safe. Patients with aneurysmal hemorrhage have a target SBP of <160mmHg
Miller J et al. Management of Hypertension in Stroke. Ann Emerg Med 2014;64:248-255
Category: Critical Care
Posted: 9/8/2014 by John Greenwood, MD
(Updated: 9/9/2014)
Click here to contact John Greenwood, MD
Goal-Directed Resuscitation During Cardiac Arrest
Focusing on high-quality CPR is by far one of the most effective methods to ensure your arrested patient has the best chance to survive. However, emerging evidence suggests that there are additional goals that we should try and accomplish during our resuscitation.
As we continue to move toward goal-directed resuscitation strategies, optimizing coronary perfusion pressure (CPP) may be our next target in “personalizing” the care we provide to those in cardiac arrest.
A recent AHA consensus statement recommended the following physiologic goals during cardiac arrest care:
Each of these variables can give the provider valuable feedback about how their patient is responding to their resuscitation. Some argue that the DBP target should be much higher (>35 mmHg), with the caveat that pharmacologic optimization can only occur once high quality CPR is confirmed. The goal should always be to minimize the use of epinephrine whenever possible!
Bottom Line: During your next cardiac arrest resus, consider using a goal-directed strategy by monitoring the patient’s CPP, DBP, & EtCO2 to determine the effectiveness of your resuscitation.
Suggested Reading
Follow me on Twitter @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 9/8/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
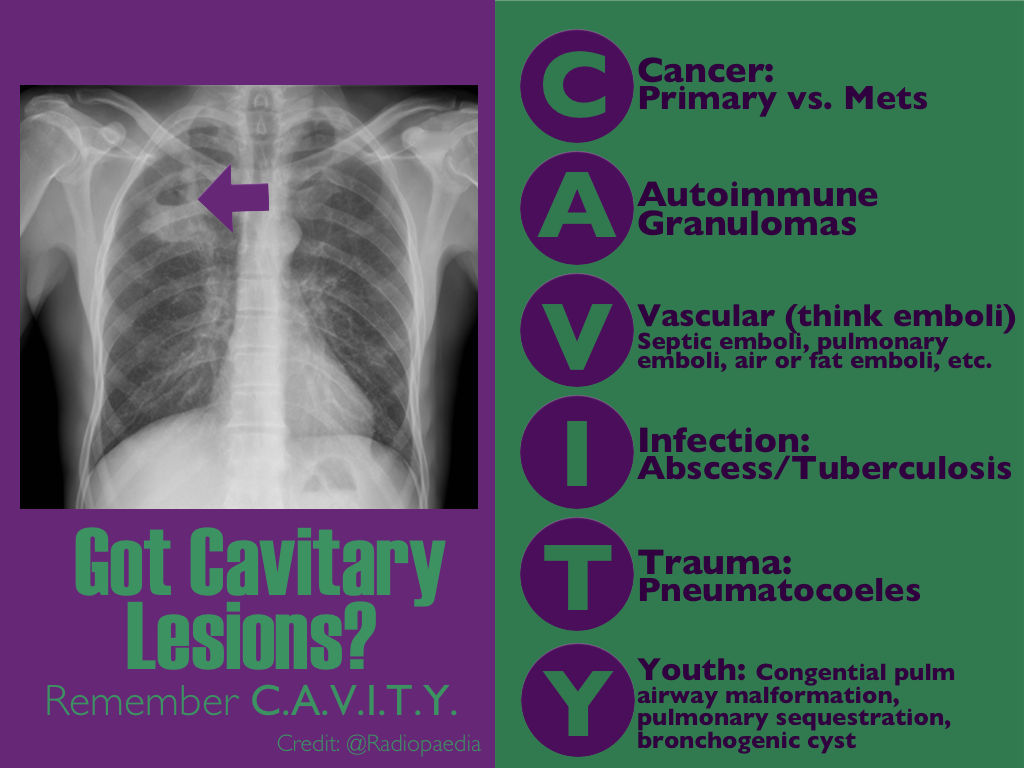
CXR shown below, what's the diagnosis? ...and name 3 differential diagnoses.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 9/7/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
PARADIGM Shift in Heart Failure
- Angiotensin-converting enzymes inhibitors (ACE-I) are cornerstone for treatment of heart failure (HF) given the multiple trials which have shown their positive risk reduction in cardiovascular death.
- Studies looking at the effect of angiotensin-receptor blockers (ARBs) on mortality have been inconsistent; thus ARB's have been recommended as 2nd-line for those who have unacceptable side effects to ACE-I.
- A recent double-blinded RCT (PARADIGM-HF) ~8400 patients with class II-IV HF w/ ejection fraction <40% were treated with enalapril (standard therapy) versus novel therapy with neprilysin (neutral endopeptidase) inhibitor combined with an ARB.
- Primary outcomes were death from cardiovascular causes and hospitalization for HF; The RCT was ceased early (~27 months) because of an overwhelming benefit with the new agent.
- At study closure death occurred 26.5% in the standard group versus 21.8% in the novel group. The risk of HF hospitalization was decreased 21% with novel therapy.
- In early studies the use of a neprilysin inhibitor combined with an ARB has shown superior effects to current standard therapy (ACE-I), however long-term effects of this novel therapy are yet to be determined.
McMurray J, Packer M, Desai A, et al. Angiotension-Neprilysin Inhibition versus Enalapril in Heart Failure. NEJM August 30, 2014.
