Category: International EM
Keywords: Seizure, International, Valproate (PubMed Search)
Posted: 4/30/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Background Information:
ACEP has recently revised its 2004 policy on critical issues in the evaluation and management of adult patients with seizures in the emergency department.
Pertinent Study Design and Conclusions:
Bottom Line:
As an alternative to phenytoin or fosphenytoin, valproate may be considered for refractory convulsive status epilepticus if benzodiazepines fail.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
Category: Critical Care
Posted: 4/29/2014 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Antibiotic Timing in Severe Sepsis/Septic Shock
Ferrer R, Martin-Loeches I, Phillips G, et al. Empiric antibiotic treatment reduces mortality in severe sepsis and septic shock from the first hour: results from a guideline-based performance improvement program. Crit Care Med 2014. [epub ahead of print]
Category: Visual Diagnosis
Posted: 4/28/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
66 year-old female presents with one week of epigastric and right flank pain. Urinalysis was normal. What’s the diagnosis?

Answer: Choledocholithiasis with pancreatitis secondary to 2.2 cm common bile duct stone
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Brain-heart syndrome, Neurogenic Stress Cardiomyopathy (PubMed Search)
Posted: 4/27/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
Category: Pharmacology & Therapeutics
Keywords: Tylenol, liver faliure (PubMed Search)
Posted: 4/6/2014 by Brian Corwell, MD
(Updated: 4/27/2014)
Click here to contact Brian Corwell, MD
Acetaminophen spent much of 2013 being chased by paparazzi and sharing magazine covers with Miley Cyrus. What a fall from stardom after becoming known as the pain reliever “hospitals use most,” and the one, “recommended by pediatricians.” Slogans we know well based on $100 million/year spent on advertising.
Approximately 150 patients a year die from unintentional acetaminophen poisoning averaged over the past 10 years. From 2001 to 2010, annual acetaminophen-related deaths amounted to about twice the number attributed to all other over-the-counter pain relievers combined,
The FDA sets the maximum recommended daily dose of acetaminophen at 4 grams, or eight extra strength acetaminophen tablets.
Ingestion of 150 mg/kg or approximately 10g for a 70 mg individual reaches the toxic threshold for a single ingestion. The toxic threshold decreases in cases of chronic ingestion.
Patients who “unintentionally” overdose have been found to take just over 8g per day (almost double the recommended maximum). This is unlikely due to taking one extra 325mg tablet once or twice.
Before we all go on a mad NSAID prescribing binge, let's all be aware of the dangers, educate our patients and allow Acetaminophen to walk the red carpet again.
http://www.propublica.org/article/tylenol-mcneil-fda-use-only-as-directed
Category: Toxicology
Keywords: Envenomation, Compartment Syndrome, Risk Factors (PubMed Search)
Posted: 4/24/2014 by Kishan Kapadia, DO
Click here to contact Kishan Kapadia, DO
Venomous snakes are believed to be everywhere in the United States except Maine, Hawaii, and Alaska. Most snakebites occur from months of April to October since snakes hibernate in the winter. Most bites occur in the extremities (lower > upper). One of the serious clinical manifestation of snakebite is compartment syndrome.
The following are risk factors for the development of increased intracompartmental pressures:
1) Envenomation of small children
2) Envenomation of digits
3) Application of ice or cold packs
4) Delayed use of antivenin
5) Inadequate dosing of antivenin
Cumpston KL. Is there a role for fasciotomy in Crotalinae envenomations in North America? 2011. Clin Tox 49(5):351-365.
Category: International EM
Keywords: International, virus, middle east, (PubMed Search)
Posted: 4/23/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Area of the world affected:
Relevance to the US physician:
Bottom Line:
Evaluate patients for MERS-CoV infection if they develop fever and pneumonia within 14 days after traveling to countries in or near the Middle East or if they had close contact with someone from this area.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
Category: Critical Care
Keywords: intubation, neurocritical care, mechanical ventilation, direct laryngoscopy, video laryngoscopy (PubMed Search)
Posted: 4/20/2014 by John Greenwood, MD
(Updated: 4/22/2014)
Click here to contact John Greenwood, MD
Direct vs. video laryngoscopy in the patient with an acute TBI
Hypoxia and hypotension are considered the "lethal duo" in patients with traumatic brain injury. In a recent randomized control trial (by our own Dr. Dale Yeatts at the Shock Trauma Center) mortality outcomes were compared between 623 consecutive patients who were intubated with either direct laryngoscopy (DL) or video laryngoscopy (VL). Here is what they found:
1. No significant difference in mortality for all comers (Primary Outcome)
2. In the subset of patients with severe head injuries, there was:
There is a reasonable amount of literature that shows hypoxia and hypotension significantly contribute to morbidity & mortality in the TBI patient, and a growing body of literature that suggests intubation with VL takes longer than DL.
Bottom Line: When choosing a method of intubation for the TBI patient, remember the "Lethal Duo" and consider direct laryngoscopy with manual inline stabilization first.
Reference
Yeatts DJ, Dutton RP, Hu PF, et al. Effect of video laryngoscopy on trauma patient survival: a randomized controlled trial. J Trauma Acute Care Surg. 2013;75(2):212-9.
Follow me on Twitter @JohnGreenwoodMD
Email: johncgreenwood@gmail.com
Category: Cardiology
Posted: 4/21/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Subcutaneous Defibrillator
- The implantable cardioverter-defibrillator (ICD) has evolved from devices through epicardial patch electrodes introduced by thoracotomy to transvenous leads advanced to the right ventricle
- Transvenous ICD (T-ICD) reduced the morbidity associated w/thoracotomy implants, however involves potential complications including: hemopericardium, hemothorax, pneumothorax, lead dislodgement, lead malfunction, device-related infection, and venous occlusion
- Subcutaneous ICD (S-ICD) offers the advantage of eliminating the need for intravenous & intracardiac leads. Clinical trials have proven its effectiveness in detecting and treating ventricular fibrillation/tachycardia; however its major disadvantage is its inability to provide bradycardia rate support and anti-tachycardia pacing to terminate ventricular tachycardia
- No study has directly compared the T-ICD & the S-ICD, however clinical data suggests that its use be considered in relatively younger patients (i.e., age <40 years), those at increased risk for bacteremia, patients with indwelling intravascular hardware at risk for endovascular infection, or in patients with compromised venous access
Aziz S, Leon A, et al. The Subcutaneous Defibrillator. JACC Vol 63, Issue 15, Pages 1473-1479
Category: Pediatrics
Keywords: scabies, pediatrics (PubMed Search)
Posted: 4/18/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Scabies is considered by the WHO to be one of the main neglected diseases with approximately 300 million cases worldwide each year. One third of cases of scabies seen by dermatologists are in kids less than 16 years old. The belief had been that presentation varies by age. One French study reported a first time miss rate of more than 41% and an overall diagnostic delay of 62 days.
A prospective, multi center observational study of patients with confirmed scabies sought to determine common phenotypes in children. All patients were seen by dermatologists in France and administered standard questionnaires. They were divided into 3 age groups, <2 years, 2-15 years and > 15 years. 323 patients were included.
The study found that:
-infants were more likely to have facial involvement and nodules, especially on the back and axilla
-relapse was more common in < 15 year olds - this was hypothesized to be due to poor compliance with treatment to the head
-family members with itch, or planter or scalp involvement were independently associated with diagnosis of scabies in kids < 2 years
-burrows were seen in 78%, nodules in 67% and vesicles of 43% of patients (see photo)
-itching was absent in up to 10% of patients
Bottom line: Have a high suspicion for scabies in any rash.
Category: Toxicology
Keywords: caustic ingestion; esophageal injury (PubMed Search)
Posted: 4/17/2014 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Caustic ingestion can potentially cause significant esophageal and/or gastric injury that can lead to significant morbidity, including death.
Endoscopy is often performed:
· To determine the presence of caustic injury.
· To determine the severity of caustic injury (grade: I to III).
| Grade | Tissue finding | Sequela |
| I | • Erythema or edema of mucosa • No ulceration | No adverse sequela |
| IIa | • Submucosal ulceration and exudates • NOT circumferential | No adverse sequela |
| IIB | • Submucosal ulceration and exudates • Near or circumferential | Stricture > 70% |
| IIII | • Deep ulcers/necrosis • Periesophageal tissue involvement | Acute Perforation and death Chronic Strictures and increased cancer risk |
· Placement of orogastric or nasograstic tube for nutritional support if needed (grade IIb and III)
Evidence for predictor of esophageal injury (frequently cited) comes from mostly studies involving pediatric population and unintentional ingestion:
1. Gaudreault et al. Pediatrics 1983;71:767-770.
o Studied signs/symptoms: nausea, vomiting, dysphagia, refusal to drink, abdominal pain, drooling or oropharyngeal burn
o Presence of symptoms: Grade 0/I lesion: 82%; Grade II: 18%
o Absence of symptoms: Grade 0/I: 88%; Grade II: 12%
2. Crain et al. Am J Dis Child. 1984;138(9):863-865
o Presence of 2 or more (vomiting, drooling and stridor) identified all (n=7) grade II and III lesion.
o Presence of 1 or no symptoms: no grade II/III lesions
o Stridor alone associated with grade II/III lesions (n=2)
o 10% of patients without oropharyngeal burns had grade II/III lesions.
3. Gorman et al. Am J Emerge Med 1990;10(3):189-194.
o Two or more symptoms: vomiting, dysphagia, abdominal pain or oral burns
o Sensitivity: 94%; specificity 49%
o Positive predictive value 43% ; negative predictive value: 96%
o Stridor alone (n=3): grade II or greater lesion
4. Previtera et al. Pediatric Emerg Care 1990;6(3):176-178.
o Esopheal injury in 37.5% of patients without oropharyngeal burn
o Grade II/III injury: 8 patients
Available data suggests that there are no “good” or reliable predictors for esophageal injury.
However, high suspicion for gastrointestinal injury should be considered with GI consultation for endoscopy in the presence of
· Stridor alone
· Two or more sx: vomiting, drooling or stridor (Crain et al)
· Intentional suicide attempt
Category: International EM
Keywords: International, Mental Health, burden of disease (PubMed Search)
Posted: 4/15/2014 by Andrea Tenner, MD
(Updated: 4/16/2014)
Click here to contact Andrea Tenner, MD
General Information:
Relevance to the US physician:
Bottom Line:
Mental illness is an often-forgotten cause of significant morbidity worldwide. Front-line care delivered by appropriately trained and supervised community-based health workers operating in partnership with emergency physicians, primary care physicians, and mental health specialists is key to address this health crisis.
University of Maryland Section of Global Emergency Health
Author: Terrence Mulligan DO, MPH
Transforming Lives, Enhancing Communities — Innovations in Global Mental Health. February 6, 2014 Patel V. and Saxena S. N Engl J Med 2014; 370:498-501
Category: Critical Care
Posted: 4/15/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Only 50% of hemodynamically unstable patients will improve their hemodynamics in response to a fluid bolus. However, because excessive fluid administration can lead to organ edema and dysfunction, it is important to give hemodynamically unstable patients only the necessary amount of fluids to improve their hemodynamics.
There are two general categories of assessing a patient's response to volume administration; static and dynamic assessments (see referenced article below):
Static assessment (generally unreliable, but traditionally used):
Physical exam (dry mucus membranes, cool extremities, etc.)
Urine output
Blood pressure
Central venous pressure via central-line
Dynamic assessment (more reliable but more labor intensive)
Pulse Pressure Variation
IVC Distensibility Index
End-expiratory occlusion test
Passive Leg-Raise
There is no simple way to accurately determine the need for a fluid bolus however the integration of the techniques above can help the clinician make better decisions.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 4/14/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
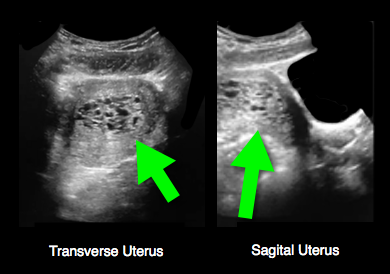
25 year-old female (G1P1) presents with 3 weeks of vaginal bleeding. Her serum beta-HCG is 65,000. Her bedside ultrasound is below; what's the diagnosis?
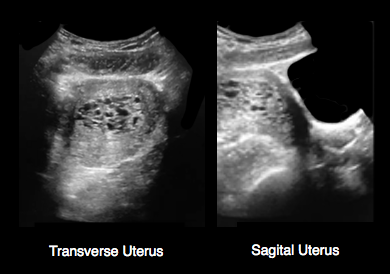
Answer: Hydatidiform mole (molar pregnancy)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Out of hospital cardiac arrest, OHCA, Prehospital airway management (PubMed Search)
Posted: 4/13/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
Optimal out of hospital cardiac arrest (OHCA) airway management strategies remain unclear. In the US, 80% of OHCA patients receive prehospital airway management, most commonly endotracheal intubation (ETI). There is growing enthusiasm for use of supra-glottic airways (SGA) by EMS because of ease of insertion, and the thought that use of SGA reduces interruptions in chest compressions. More recently, studies have suggested improved survival without the insertion of any advanced airway device at all.
A recent secondary analysis of OHCA outcomes in the Cardiac Arrest Registry to Enhance Survival (CARES) compared patients receiving endotracheal intubation (ETI) versus supra-glottic airway (SGA), and also patients receiving [ETI or SGA] with those receiving no advanced airway.
Of 10,691 OHCA, 5591 received ETI, 3110 SGA, and 1929 had no advanced airway. Unadjusted neurologically-intact survival was: ETI 5.4%, SGA 5.2%, no advanced airway 18.6%. Compared with SGA, ETI achieved higher sustained ROSC, survival to hospital admission, hospital survival, and hospital discharge with good neurologic outcome. Moreover, compared with [ETI or SGA], patients who received no advanced airway attained higher survival to hospital admission, hospital survival, and hospital discharge with good neurologic outcome.
Conclusion: In CARES, patients receiving no advanced airway exhibited superior outcomes than those receiving ETI or SGA. When an advanced airway was used, ETI was associated with improved outcomes compared to SGA.
McMullan J, Gerecht R, Bonomo J, et al. Airway management and out-of-hospital cardiac arrest outcome in the CARES registry. Resuscitation. 2014;85(5):617–622. doi:10.1016/j.resuscitation.2014.02.007.
Category: Pediatrics
Posted: 4/11/2014 by Rose Chasm, MD
(Updated: 2/7/2026)
Click here to contact Rose Chasm, MD
Category: Toxicology
Keywords: alcohol, gabapentin, dependence (PubMed Search)
Posted: 4/7/2014 by Bryan Hayes, PharmD
(Updated: 4/10/2014)
Click here to contact Bryan Hayes, PharmD
In a 12-week treatment course,150 alcohol-dependent patients were randomized to receive placebo, gabapentin 900 mg/day, or gabapentin 1,800 mg/day.
Mason BJ, et al. Gabapentin treatment for alcohol dependence: a randomized clinical trial. JAMA Intern Med 2014;174(1):70-7. [PMID 24190578]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: International, Fever, Hemorrhagic (PubMed Search)
Posted: 4/9/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Clinical Presentation:
Diagnosis:
Treatment:
Bottom Line:
University of Maryland Section of Global Emergency Health
Author: Veronica Pei
The CDC Yellow Book 2014 available at: http://wwwnc.cdc.gov/travel/yellowbook/2014/chapter-3-infectious-diseases-related-to-travel/viral-hemorrhagic-fevers
Category: Critical Care
Keywords: map, sepsis, septic shock, hypertension (PubMed Search)
Posted: 4/7/2014 by Feras Khan, MD
(Updated: 4/8/2014)
Click here to contact Feras Khan, MD
How low should you go? MAP Goals in Septic Shock
Background:
The Trial:
Outcome:
Bottom Line:
Pierre Asfar, M.D., Ph.D. et al. for the SEPSISPAM Investigators
March 18, 2014DOI: 10.1056/NEJMoa1312173
Category: Visual Diagnosis
Posted: 4/7/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
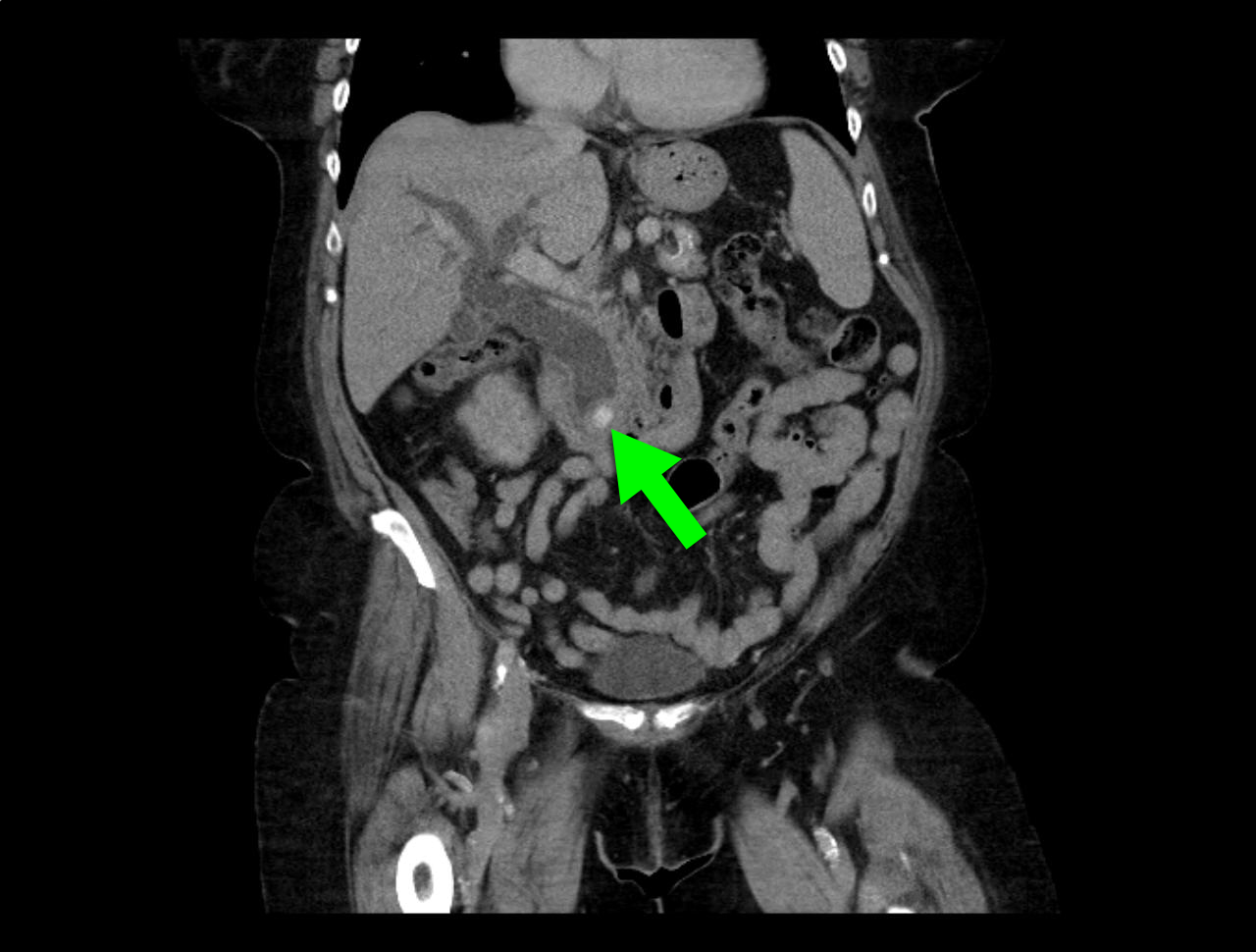
23 year-old female presents complaining of progressive right lower quadrant pain after doing "vigorous" pushups. CT abdomen/pelvis below. What’s the diagnosis? (Hint: it’s not appendicitis)

Answer: Rectus sheath hematoma
Rectus Sheath Hematoma (RSH)
Rectus muscle tear causing damage to the superior or inferior epigastric arteries with subsequent bleeding into the rectus sheath; uncommon cause of abdominal pain but mimics almost any abdominal condition.
May occur spontaneously, but suspect with the following risk factors:
Typically a self-limiting condition, but hypovolemic shock may result from significant hematoma expansion.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
