Category: Orthopedics
Keywords: back pain, analgesia (PubMed Search)
Posted: 10/24/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
A traditional ED practice has been to combine promethazine as an anxiolytic adjunct to morphine for patients with musculoskeletal pain (eg back pain).
However, when compared to morphine alone, this combination does not lead to greater analgesia or decrease anxiety. It does however prolong ED length of stay.
This use of this "pain cocktail" is not recommended
Behrbalk E, Halpern P, Boszczyk BM, et al. Anxiolytic medication as an adjunct to morphine analgesia for acute low back pain management in the emergency department: A prospective randomized trial. Spine (Phila Pa 1976). 2014;39(1):17-22.
Category: Pediatrics
Keywords: UTI, Fever, febrile, AAP, clinical practice guideline (PubMed Search)
Posted: 10/23/2015 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Fever is the most common presenting symptoms to pediatric emergency departments 10-20%
Singh S., Sandelich S., Current Status of the Diagnosis and Treatment of Pediatric Urinary Tract Infections. Pediatric Emergency Medicine Reports 2014;19(2):13-22.
Roberts KB, Subcommittee on Urinary Tract Infection, Steering Committee on Quality Improvement and Management. Urinary tract infection: clinical practice guideline for the diagnosis and management of the initial UTI in febrile infactns and children 2 to 24 months. Pediatrics. 2011 Sept; 128(3):595-610.
Category: Toxicology
Keywords: propranolol, lipid emulsion (PubMed Search)
Posted: 10/22/2015 by Fermin Barrueto
Click here to contact Fermin Barrueto
There have been a variety of case reports that have been describing the effects of lipid emulsion therapy on severe hemodynamic overdoses. As time has gone on, we have realized that this therapy is not for all severe overdoses. The type of medication and its pharmacokinetic properties factor into the decision. There is minimal evidence and no ideal randomized control trials that will tell us what the right answer is but take beta-blockers for instance:
Atenolol - in overdose, consider hemodialysis, very effectively removed by HD [1]
Propranolol - very lipophilic and one of the few beta-blockers that can cause widened QRS, seizures as well as the prototypical hypotension and bradycardia.
Because of its lipophilicity, ability to cross the blood brain barrier and ability to cause lethal dysrrthmias, lipid emulsion therapy has been effective in reversing the clinically severe effects of a propranolol overdose. [2]
1)Case report: atenolol overdose successfully treated with hemodialysis.
Huang SH, Tirona RG, Ross C, Suri RS.
Hemodial Int. 2013 Oct;17(4):652-5. doi: 10.1111/hdi.12020. Epub 2013 Jan 24.
Jovic-Stosic J, Gligic B, Putic V, Brajkovic G, Spasic R.
Clin Toxicol (Phila). 2011 Jun;49(5):426-30. doi: 10.3109/15563650.2011.583251.
Category: International EM
Keywords: Road traffic, injuries, World Health Organization (PubMed Search)
Posted: 10/20/2015 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 11/4/2015)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
The World Health Organization (WHO) has just released a report on the current status of road traffic safety globally.
From a postive perspective, road traffic deaths are stabilzing even though the number of motor vehicles are rapidly increasing.
The bottom line- injuries are preventable. Continued policy efforts, laws with enforncement, can save lives. Specific life saving legislation includes:
http://www.who.int/mediacentre/news/releases/2015/road-safety-report/en/
Category: Critical Care
Posted: 10/20/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
There is more than the standard preparations of plasma, platelets, and PRBCs in the blood bank. Certain patients will require these specialized preparations when a transfusion is required. Here are three to know:
Follow me on Twitter (@criticalcarenow)
Category: Visual Diagnosis
Posted: 10/19/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
8 year-old female presents with nausea, vomiting, double-vision and inability to move her left eye upwards after being kicked in the face at school. What's the diagnosis?
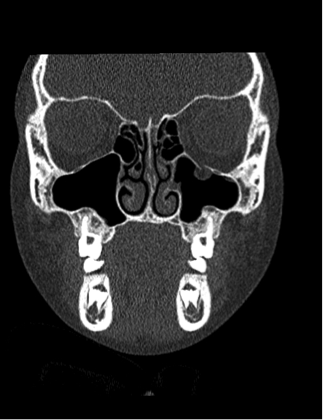
Orbital floor fracture with entrapment of the inferior rectus muscle.
Follow me on Twitter (@criticalcarenow)
Category: Pediatrics
Keywords: Blunt abdominal trauma, seat belt sign, pediatrics (PubMed Search)
Posted: 10/16/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Our suspicion of significant abdominal injury increases when there is bruising across the abdomen in adults after a motor vehicle collision, but what about in children? A PECRAN analysis may have provided us with the answer.
Of 3740 pediatric patients after motor vehicle collision, 16% had a seat belt sign. Seat belt sign was defined as a continuous area of erythema, ecchymosis or abrasion across the abdomen due to the seat belt. 1864 children had CT scans of the abdomen. Intra-abdominal injuries (IAI) were more common in those children with seat belt sign than those without (19% versus 12%). Those with seat belt sign had a greater risk of hallow viscous or mesenteric injuries. There was no increased risk of solid organ injury. 33% of patients with seat belt sign did not have complaints of abdominal pain or tenderness on initial exam (with a GCS of 14 or 15); 2% of these patients underwent operative intervention for their injuries.
Borgialli et al. Association Between the Seat Belt Sign and Intra-abdominal Injuries in Children With Blunt Torso Trauma in Motor Vehicle Collisions. Academic Emergency Medicine, 2014; 21: 1240 1248.
Category: Toxicology
Keywords: body stuffer, body packer, CAT Scan (PubMed Search)
Posted: 10/15/2015 by Hong Kim, MD
Click here to contact Hong Kim, MD
Toxicity due to body packing and body stuffing can be a significant concern due to unknown quantity and/or substance that was ingested.
A recent prospective observational case series compared the utility of CT abdomen/pelvis with and without PO contrast in identifying the ingested packets.
The gold standard comparison: surgical removal or expulsion of packets.
All patients received CT abd/pelvis with and without PO contrast.
A. Body stuffers (n = 24)
CT w/ PO contrast:
Positive: 7 (sensitivity 29.2%)
Negative: 17
CT w/o PO contrast:
Positive: 9 (sensitivity 36.5%)
Negative: 15
All 24 patients passed ingested packets
B. Body packers (n= 11)
CT w/ PO contrast
CT w/p PO contrast
10 patients expulsed packets; one patient did not have any packets.
Conclusion
Bottom line:
Shahnazi M et al. Comparison of abdominal computed tomography with and without oral contrast in diagnosis of body packers and body stuffers. Clin Toxicol 2015;53:596-603.
Category: Neurology
Keywords: serotonin syndrome, SSRI, SNRI, MAOI, TCA (PubMed Search)
Posted: 10/14/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Last month we discussed symptoms of serotonin syndrome and its diagnosis by the Hunter Criteria. Let's move on to what causes serotonin syndrome.
Serotonin Syndrome - What Causes It?

** Stay tuned for the conclusion on management of serotonin syndrome **
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: central line, cvc (PubMed Search)
Posted: 10/13/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Parienti et al. INtravascular complications of central venous catherization by insertion site. N ENGL J MED 373;13. Sept 24, 2015
Category: Visual Diagnosis
Posted: 10/12/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
5 year-old boy who presents with sudden onset hoarse voice, and drooling without a fever.
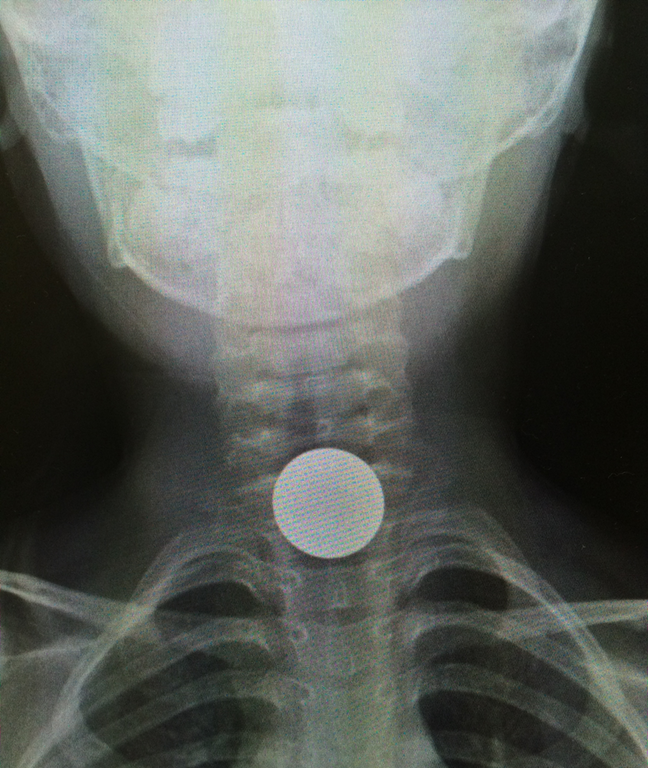
Coin lodged in the esophagus
Coin ingestions
Follow me on Twitter (@criticalcarenow)
Category: Toxicology
Keywords: hemodialysis, dabigatran, rebound (PubMed Search)
Posted: 10/7/2015 by Bryan Hayes, PharmD
(Updated: 10/8/2015)
Click here to contact Bryan Hayes, PharmD
In patients receiving renal replacement therapy as a treatment modality for dabigatran-related bleeding, watch for a rebound concentration increase after hemodialysis is stopped.
More than 50% of patients demonstrate a rebound effect with a median increase in dabigatran concentration of 33%.
It is unclear whether this rebound effect is clinically important, and whether it translates to prolonged clinically relevant bleeding. Extended hemodialysis sessions or consideration of CVVHD should offset this potential problem.
Bonus Pearl:
The North American Congress of Clinical Toxicology starts today and runs through October 12. Look for toxicology pearls and updates on Twitter under the official conference hashtag #NACCT15.
Chai- Adisaksopha C, et al. Hemodialysis for the treatment of dabigatran-associated bleeding: a case report and systematic review. J Thromb Haemost 2015;13(10):1790-8. [PMID 26270886]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Suicide, injury, self harm, youth (PubMed Search)
Posted: 10/7/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Overall, suicide is the 15th leading global cause of death. However, it is the 2nd leading cause among 15-29 year olds
Suicides are preventable. Interventions to decrease suicides include:
http://www.who.int/mediacentre/factsheets/fs398/en/
Category: Visual Diagnosis
Posted: 10/5/2015 by Haney Mallemat, MD
(Updated: 10/7/2015)
Click here to contact Haney Mallemat, MD
Patient presents after being started on an antibiotic for cellutlitis of lower extremity. What's the diagnosis and what are some other etiologic agents (name 3)
Erythema Multiforme (minor)
Follow me on Twitter (@criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: targeted temperature management, drug (PubMed Search)
Posted: 9/27/2015 by Bryan Hayes, PharmD
(Updated: 10/3/2015)
Click here to contact Bryan Hayes, PharmD
An excellent new review article provides a detailed look at how the drugs we give are affected by targeted temperature management. Here is a helpful chart of drug alterations that have data in reduced body temperature states:
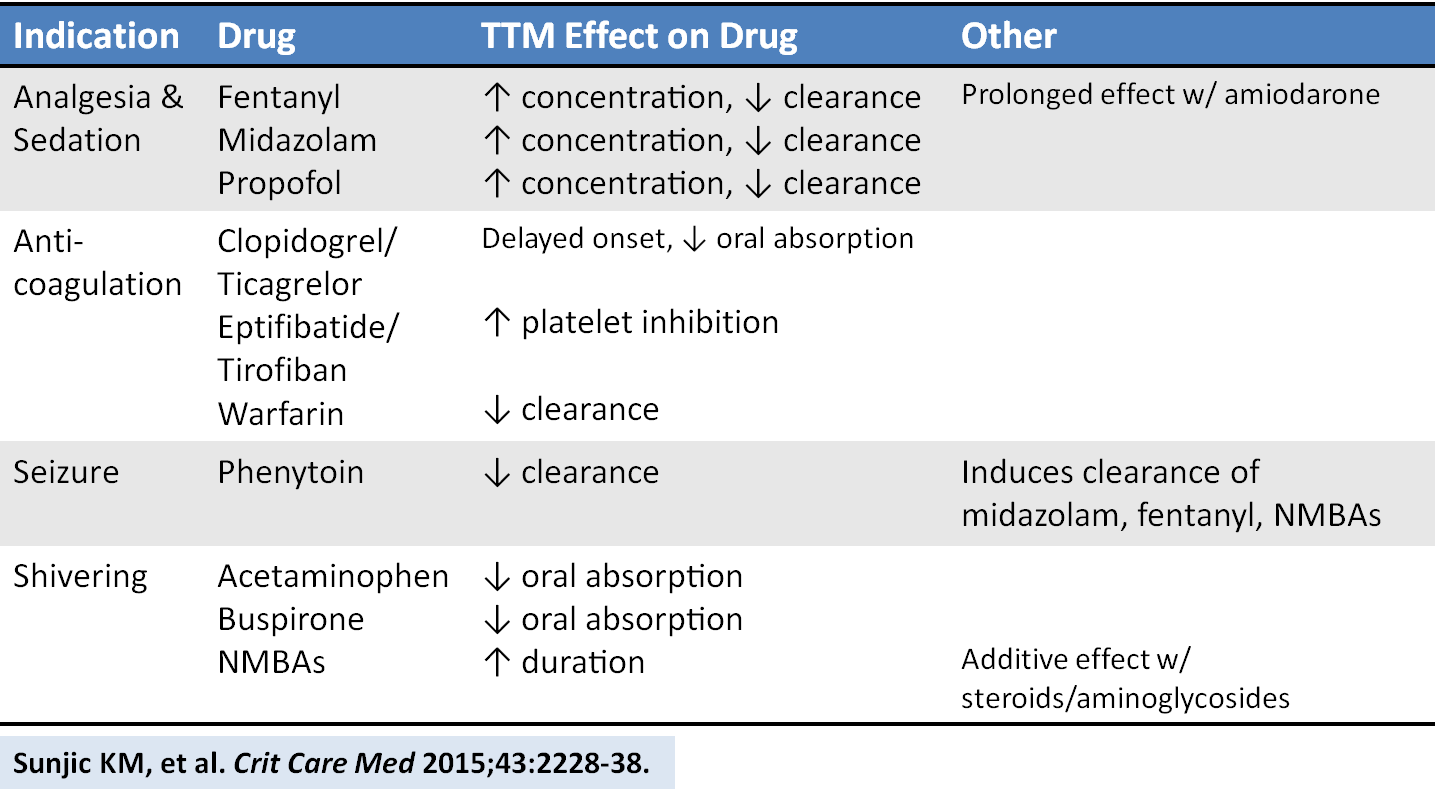
Sunjic KM, et al. Pharmacokinetic and other considerations for drug therapy during targeted temperature management. Crit Care Med 2015;43:2228-38. [PMID 26237312]
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: pediatric, code, resuscitation, medication error (PubMed Search)
Posted: 10/3/2015 by Christopher Lemon, MD
Click here to contact Christopher Lemon, MD
A group from Colorado identified the high-stress of pediatric resuscitation as a high-risk setting for possible medication error. As such, they performed a prospective, block-randomized, crossover study with two mixed teams of docs (ABEM certified) and nurses, managing 2 simulated peds arrest scenarios using either:
1) conventional “draw-up and push” drug administration methods [control] or
2) prefilled medication syringes labeled with color-coded volumes correlating to the weight-based Broselow Tape dosing [intervention].
The objective was to compare the time of preparation and administration of a medication, as well as to assess dosing errors. Participants were blinded to the purpose during recruitment but unblinded just prior to running the scenarios.
The scenarios included advanced airway management and hemodynamic life support efforts to care for an 8-year-old or 8-month-old manikin. The intervention group received a standard 3-minute tutorial on the use of prefilled color-coded syringes just prior to their scenario. After completing the first scenario, the groups switched, utilizing the other sim with the other method of medication administration. After a 4-16 week “wash out” period, the groups reconvened to reverse the medication administration technique across the same 2 scenarios.
Each Broselow tape color zone corresponds to a narrow range of weights. The authors opted to designate medication dosing errors >10% above or below the correct range as critical dosing errors.
The results? Median time to delivery of all conventionally administered medication doses was 47 seconds versus the prefilled color-coded administration system-- 19 seconds. The conventional administration system saw 17% of doses with critical errors versus none for the prefilled color-coded syringe group.
These prefilled color-coded syringes are not currently manufactured. Should they go into commercial production, the hope is that such syringes would be longer and more narrow than conventional syringes to effectively elongate each color-coded section (the delineations for red and purple on a standard syringe differ by as little as 1/8-3/32 of an inch if you want to make your own!-- see picture).
Color-Coded Prefilled Medication Syringes Decrease Time to Delivery and Dosing Error in Simulated Emergency Department Pediatric Resuscitations. Moreira, Maria E. et al. Annals of Emergency Medicine, Volume 66 , Issue 2 , 97 - 106.e3.
Category: Toxicology
Keywords: Odansetron, Zofran (PubMed Search)
Posted: 10/2/2015 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Category: International EM
Keywords: international, American College of Emergency Physicians, emergency medicine (PubMed Search)
Posted: 9/30/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
If you are interested in learning about the current status of emergency medicine in a specific country, it can be difficult to find up-to-date information. One excellent resource for country specific details is the American College of Emergency Physicians’ (ACEP) International Ambassador Program.
This program has Emergency Medicine Ambassadors (U.S. emergency physicians), Liaisons (in-country emergency physicians) and Representatives (U.S. emergency physicians in training) for many countries around the world. Additionally, there are country specific reports that give annually updated information about emergency medicine in each country.
Included on the website are links to send emails to the Ambassadors, Liaisons and Representatives in order to request more detailed information.
To learn more, see: http://www.acep.org/IntlAmbassador/
Category: Critical Care
Keywords: Aortic dissection, STEMI, cardiac tamponade, aortic insufficiency, echocardiography (PubMed Search)
Posted: 9/30/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
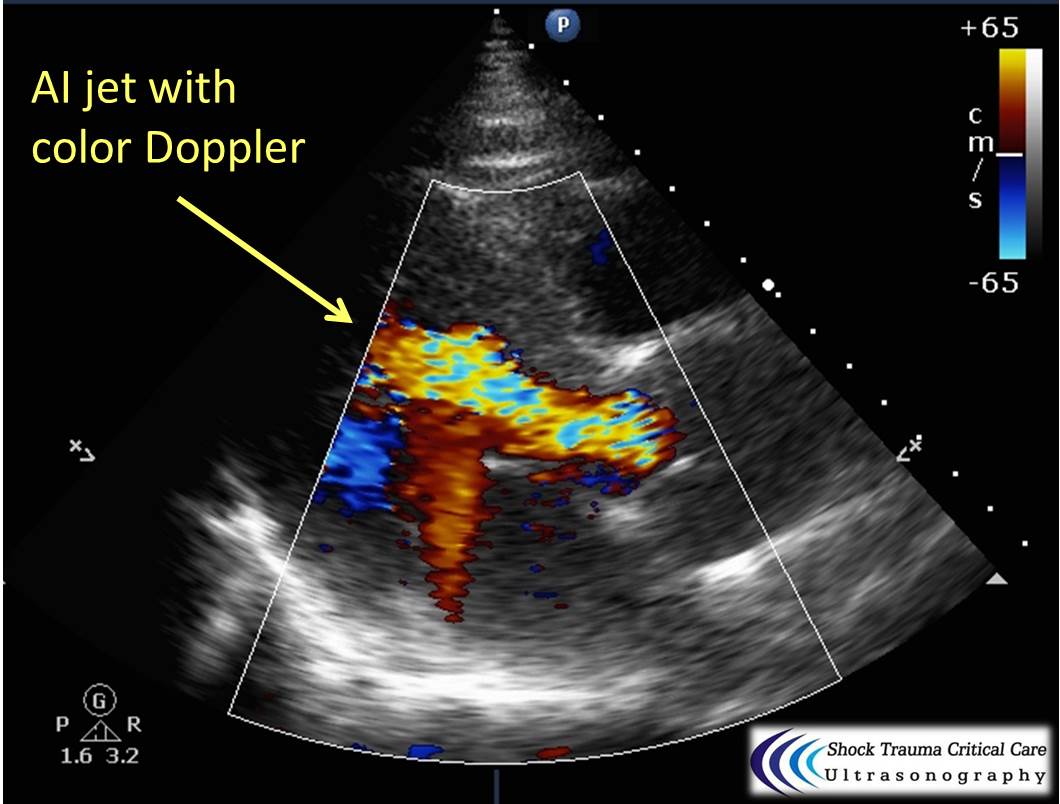
Classically, aortic dissection presents as tearing or ripping chest pain that radiates to the back in a HYPERtensive patient.
However, type A aortic dissections can quickly become HYPOtensive due to any the primary cardiac complications from retrograde dissection into:
Bedside echo can't rule out aortic dissection, but it can help rule in the diagnosis (figure 1) or complications (figure 2) at times.
Category: Visual Diagnosis
Posted: 9/28/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
26 year-old male presents with a swollen 4th digit and pain during extension, what’s the diagnosis?

Answer: Infectious Flexor Tenosynovitis
Infectious Flexor Tenosynovitis
Follow me on Twitter (@criticalcarenow)
