Category: Critical Care
Posted: 12/29/2015 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Acute Chest Syndrome
Cecchini J, Fartoukh M. Sickle cell disease in the ICU. Curr Opin Crit Care 2015; 21:569-75.
Category: Visual Diagnosis
Posted: 12/28/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
79 year-old male with headaches, ataxia, falls, and difficulty urinating. What's the diagnosis?
Diagnosis: Ventriculomegaly secondary to Normal Pressure Hydrocephalus
An approach to ventriculomegaly
Ventriculomegaly is due to cerebral atrophy (e.g., Parkinson disease) or increased cerebrospinal fluid (CSF) within the ventricles. Increased CSF is due to:
Congenital causes of ventriculomegaly:
Acquired causes of ventriculomegaly:
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Adolescent, head injury (PubMed Search)
Posted: 12/26/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Protracted Recovery from Concussion
Age and sex may influence concussion recovery time frame
Methods: 266 adolescent athletes presenting to a sports medicine concussion clinic
Female athletes had a longer recovery course (P=0.002) and required more treatment interventions (p<0.001).
Female athletes were more likely to require academic accommodations (p<0.001), vestibular therapy (P<0.001) and medications (P<0.001).
Be aware that not all concussion patient subgroups with concussions recover in the same manner. Further study is needed to support whether female adolescent athletes require unique management and treatment guidelines.
Category: Neurology
Keywords: CSF, LP, HSV, infection (PubMed Search)
Posted: 12/22/2015 by Danya Khoujah, MBBS
(Updated: 1/16/2016)
Click here to contact Danya Khoujah, MBBS
HSV infection of the CNS is one of few treatable viral diseases. HSV encephalitis of older children and adults is almost always caused by herpes simplex virus type 1 (HSV-1), and in individuals older than 20, is due to HSV reactivation.
Temporal lobe localization is characteristic for HSV encephalitis in individuals older than 3 months, and is responsible for its characteristic presentation, namely bizarre behavior and expressive aphasia.
CSF analysis will usually reveal an elevated protein level, and a lymphocytic cellular predominance.
CSF protein concentration is a function of disease duration, and will continue to rise even with administration of treatment (acyclovir) and may remain elevated after the completion of therapy.
5% of CSF samples will be totally normal, and the diagnosis will only be revealed with positive PCR detection of viral DNA in the CSF, which is the gold standard for diagnosis.
The sensitivity of MRI is similar to CSF analysis, with 5% of patients with HSV encephalitis having a normal MRI on presentation, and subsequently developing abnormalities.
Of note, HSV-2 tends to cause aseptic meningitis rather than encephalitis in adults, and has a benign course.
Bottom Line? Keep a high index of suspicion for HSV encephalitis, and treat the patient empirically despite a normal CSF/MRI pending PCR results.
Whitley RJ. Herpes Simplex Virus Infections of the Central Nervous System. Continuum 2015;21(6):1704 13
Category: Critical Care
Keywords: Critical care, Trauma, TBI, ICP, hypothermia (PubMed Search)
Posted: 12/22/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
The EuroTherm3235 Trial was a randomized, multi-center trial to study hypothermia (32-35oC) in severe, traumatic brain injury1:
1. Andrews PJ, Sinclair HL, et al; Eurotherm3235 Trial Collaborators. Hypothermia for Intracranial Hypertension after Traumatic Brain Injury. N Engl J Med. 2015 Dec 17;373(25):2403-12. doi: 10.1056/NEJMoa1507581. Epub 2015 Oct 7. PubMed PMID: 26444221.
2. Brain Trauma Foundation; American Association of Neurological Surgeons; Congress of Neurological Surgeons. Guidelines for the management of severe traumatic brain injury. J Neurotrauma. 2007;24 Suppl 1:S1-106. PubMed PMID: 17511534.
Category: Orthopedics
Posted: 12/19/2015 by Michael Bond, MD
Click here to contact Michael Bond, MD
Quick pearl for those that are trying to complete their holiday shopping.
Mulder's sign is not a sign that there is an extra-terrestial in your ED, But rather a sign that your patient is suffering from a Morton's Neuroma (see pearl from 2012)
Patients will often complain of pain in 3rd and 4th intermetatarsal space and if you can reproduce the pain by compressing the metatarsal heads together then you have a Positive Mulder's sign. Check out the original pearl at https://umem.org/educational_pearls/1684/
Category: Pediatrics
Keywords: inflatable, trauma, bounce house (PubMed Search)
Posted: 12/17/2015 by Jenny Guyther, MD
(Updated: 12/18/2015)
Click here to contact Jenny Guyther, MD
Ferro V, D'Alfanso Y, Vanacore N et al. Inflatable bouncer-related injuries to children: increasing phenomenon in pediatric emergency department, 2002-2013. Eur J Pediatr. October 2015 (epub ahead of print).
Category: International EM
Keywords: Horn of Africa, Arabian Pennusla, khat, bath salts, altered mental status (PubMed Search)
Posted: 12/16/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Synthetic cathinones, known as bath salts, are a frequently used street drug in the United States. They have been discussed in a number of previous pearls. But from where did cathinone originate?
Khat (Catha edulis) is flowing plant native to the Arabian Peninsula and the Horn of Africa. It contains the monoamine alkaloid cathinone, which is an amphetamine-like stimulant that also causes euphoria. Historically, khat has been chewed for thousands of years and predates the use of coffee. Khat chewing is particularly popular in Yemen.
Khat contains many different compounds, which cause a number of different effects. Many of these effects are considered harmful to health. Khat chewing primarily impacts the central nervous system and the gastrointestinal system. However, it also has effects on cardiovascular, respiratory, endocrine, and genitourinary systems. In addition to the amphetamine like central nervous effects, other toxic effects include elevated blood pressure, tachycardia, insomnia, anorexia, constipation and general malaise.
Next time you see a patient with confusion and hallucinations from Yemen, Ethiopia, Somalia and other countries around the Horn of Africa, consider Khat in your differential.
Category: Visual Diagnosis
Posted: 12/15/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A patient arrives in acute respiratory distress with left sided chest pain. Ultrasound of the left anterior chest is shown; what's the diagnosis and name one false positive?
Lung point indicating pneumothorax (PTX)....see below for the false positives
What's the (Lung) Point
Follow me on Twitter (@criticalcarenow)
Category: Visual Diagnosis
Posted: 12/14/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
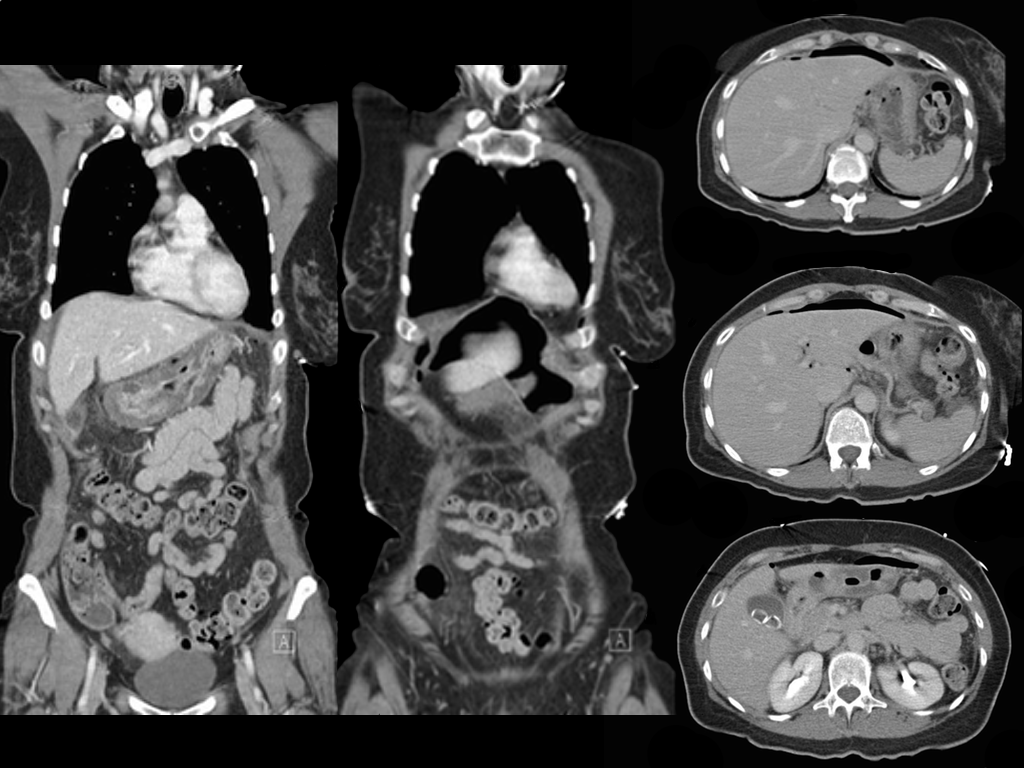
Ruptured gastric ulcer with pneumoperitoneum (CT scan below)
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Concussion, knowledge, education (PubMed Search)
Posted: 12/12/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Parental Knowledge of pediatric concussion
Sample: Parents of children brought to pediatric hospital or outpatient clinics for evaluation of orthopedic injuries.
Participants scored an average of 18.4 (0-25) on knowledge and 63.1 (15-75) on Attitudes toward concussions.
Safest attitudes were seen in white females. Knowledge increased with income and education levels.
Parents from low income or education levels may benefit from additional education in the ED prior to discharge in addition to providing paper information which may not be read or understood.
Assessment of Parental Knowledge and Attitudes toward Pediatric Sports Related Concussions.
Lin, Salzman et al., 2015. Sports Health Journal
Category: Toxicology
Keywords: laboratory, lipid, toxicology (PubMed Search)
Posted: 12/10/2015 by Bryan Hayes, PharmD
Click here to contact Bryan Hayes, PharmD
The American Academy of Clinical Toxicology's Lipid Emulsion workgroup has published its first of 4 systematic reviews on the use of lipid emulsion in toxicology, this one on lipid's effect on laboratory analyses. [1] As expected, administering a fat bolus can significantly alter labs drawn subsequently.
The key point: If you are considering lipid for overdose, draw labs prior to giving it.
Which labs are affected? Most. Here's a helpful mnemonic courtesy of Dr. Kyle DeWitt.
Also remember to give lipid in its own line. It isn't compatable with most resuscitation drugs. [2]
Follow me on Twitter (@PharmERToxGuy)
Category: Neurology
Keywords: Stroke, NIH stroke scale, NIHSS (PubMed Search)
Posted: 12/9/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
A recent study compared the original NIHSS with the shortened 11, 8, and 5 item versions.4
Bottom Line: The original 15-item NIHSS should still be used to evaluate patients’ stroke severity.
The reliability of the NIHSS has been found to improve with personal and videotaped training.
Follow me on Twitter @ EM_NCC
Category: Critical Care
Keywords: plasmalyte, normal saline, fluid, critical care, fluid resuscitation (PubMed Search)
Posted: 12/8/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
The Bottom Line: This was a nicely designed study to evaluate the safety of both fluids. It does suggest that either fluid type is for the most part OK. But in patients requiring hefty fluid boluses, we should be cautious in what type of fluid we choose.
Category: Visual Diagnosis
Posted: 12/7/2015 by Haney Mallemat, MD
(Updated: 12/8/2015)
Click here to contact Haney Mallemat, MD

Lens disclocation
Follow me on Twitter (@criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: tramadol, seizure (PubMed Search)
Posted: 12/3/2015 by Bryan Hayes, PharmD
(Updated: 7/6/2016)
Click here to contact Bryan Hayes, PharmD
Tramadol has a reputation for being a safe, non-opioid alternative to opioids. Nothing could be further from the truth. Several blogs have published about the dangers of tramadol:
But what about seizure risk? Previous studies have been unable to confirm an increased seizure risk with therapeutic doses of tramadol (Seizure Risk Associated with Tramadol Use from EM PharmD blog). However, a new study refutes that premise.
22% of first-seizure patients had recent tramadol use!
This was a retrospecitve study without laboratory confirmation of tramadol intake. Nevertheless, it behooves us not to think of tramadol as a safer alternative to opioids. It is an opioid after all, and it comes with significant adverse effects.
Asadi P, et al. Prevalence of Tramadol Consumption in First Seizure patients; a One-Year Cross-sectional Study. Emerg (Tehran) 2015;3(4):159-61. [PMID 26495407]
Follow me on Twitter (@PharmERToxGuy)
Category: Toxicology
Keywords: CO, Carbon Monoxide Detector (PubMed Search)
Posted: 12/3/2015 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Carbon monoxide (CO) is a colorless, odorless, tasteless toxic gas produced by incomplete combustion in fuel-burning devices and is a leading cause of poisoning morbidity and mortality.
Symptoms can be easily misinterpreted (e.g., headache, nausea, dizziness, or confusion) thus victims may not realize they are being poisoned.
CO detectors use an audible alarm and are effective in alerting potential victims of presence of CO. Some versions offer a digital readout of the CO concentration. Detectors are not a simple alarm level (as in smoke detectors) but are a concentration-time function.
In the UL 2034 Standard, Underwriters Laboratories specifies response times for CO alarms:
Current Occupational Safety and Health Administration permissible exposure limit for CO is 50 parts per million as an 8-hour time-weighted average concentration.
CO detectors have a limited lifespan of up to 7 years.
Forty percent of residential detectors studied failed to alarm in hazardous concentrations, despite outward indications that they were operating as intended.
CO detectors 10 years and older had the highest failure rates.
Night of sirens: analysis of carbon monoxide-detector experience in suburban Chicago. Bizovi KE, Leikin JB, Hryhorczuk DO, Frateschi LJ. Ann Emerg Med. 1998;31(6):737 740.
Residential carbon monoxide detector failure rates in the United States. Ryan TJ, Arnold KJ. Am J Public Health. 2011 Oct;101(10):e15-7. doi:10.2105/AJPH.2011.300274. Epub 2011 Aug 18.
Deaths from unintentional carbon monoxide poisoningand potential for prevention with carbon monoxide detectors. Yoon SS, Macdonald SC, Parrish RG. JAMA. 1998 Mar 4;279(9):685-7.
Category: International EM
Keywords: Injury, guns, firearms, high-income countries (PubMed Search)
Posted: 12/2/2015 by Jon Mark Hirshon, MPH, MD, PhD
(Updated: 12/5/2015)
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
On a day when the 355th mass shooting this year in the USA occurred in San Bernardino, California, it seems appropriate to discuss gun violence.
A recently accepted publication in the American Journal of Medicine compared morality data from the USA to other high-income countries, and found the following:
The US homicide rates were 7.0 times higher than the aggregated rates of all other high-income countries.
The overall US suicide rate is average
Unintentional firearm deaths were 6.2 times higher in the US.
The overall firearm death rate in the US from all causes was 10.0 times higher.
Bottom line: As stated in the article: “The US has an enormous firearm problem compared to other high-income countries with much higher rates of homicide and firearm-related suicide.”
Grinshteyn E, Hemenway D. Violent Death Rates: The United States Compared to Other High-Income OECD Countries, 2010. Am J Med. 2015 Nov 6. pii: S0002-9343(15)01030-X. doi: 10.1016/j.amjmed.2015.10.025.
Category: Critical Care
Posted: 12/1/2015 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Mechanical Ventilation for Septic Patients in Resource-Limited Settings
Neto AS, Schultz MJ, Festic E. Ventilatory support of patients with sepsis or septic shock in resource-limited settings. Intensive Care Med 2016:42:100-3.
Category: Visual Diagnosis
Posted: 11/30/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Patient presents with right elbow pain after a fall. What's the diagnosis and what other injury should you look for?

Displaced fracture of the proximal ulna.
Pearls
Follow me on Twitter (@criticalcarenow)
