Category: Critical Care
Posted: 8/25/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The RV is a low-pressure chamber that doesn’t tolerate acute increases in pulmonary pressures (e.g., ARDS, pulmonary embolism, etc.); acute increases can lead to RV dysfunction / failure
Managing RV dysfunction requires a three-pronged approach:
Follow me on Twitter (@criticalcarenow)
Category: Visual Diagnosis
Posted: 8/24/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
You find this interesting view while scanning a patient. Which view is this and why should you care about it?
This is the right ventricular inflow view
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Sodium Supplementation, Exercise-Associated Hyponatremia, Prolonged Exercise (PubMed Search)
Posted: 8/22/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Sodium Supplementation and Exercise-Associated Hyponatremia (EAH) during Prolonged Exercise (ultramarathon running)
Weight loss of around 4% body weight (relative to pre race weight) can be anticipated to maintain euhydration in such a prolonged event
Those who become symptomatic with EAH have either gained weight or lost less that 3-4% body weight
Overhydration rather than inadequate supplemental sodium intake is a greater contributor to the development of EAH
There is a suggested link between EAH and rhabdomyolysis. The mechanism remains unknown and it is unclear which condition may augment the other. Further research is needed.
Take home: Avoid overhydration during prolonged exercise to prevent EAH.
Sodium Supplementation and Exercise-Associated Hyponatremia (EAH) during Prolonged Exercise (ultramarathon running) Hoffman and Stuempfle 2015.
Category: Pediatrics
Keywords: VBG, DKA, acidosis, hyperglycemia (PubMed Search)
Posted: 8/21/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
The answer may be no, as long as you have a serum HCO3. In this retrospective study, linear regression was used to to assess serum HCO3 as a predictor of venous pH. Logistic regression was also used to evaluate serum HCO3 as a predictor of DKA. Using a HCO3 cutoff of <18 mmol/L had a sensitivity of 91.8% and specificity of 91.7% for detecting a pH <7.3. A HCO3 < 8 had a sensitivity of 95.2 % and specificity of 96.7 % for detecting a pH <7.1.
Von Oettingen J, Wolfsdorf J, Feldman, H and E Rhodes. Use of Serum Bicarbonate to Substitute for Venous pH in New-Onset Diabetes. Pediatrics 2015; 136: e371-e378.
Category: International EM
Keywords: MERS-CoV, respiratory virus, coronavirus, infectious disease (PubMed Search)
Posted: 8/20/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Introduction: As discussed in previous Pearls, Middle East respiratory syndrome coronavirus (MERS-CoV) is a recently emerged respiratory viral infection that is caused by a single stranded, positive-sense RNA novel coronavirus.
Updates:
As of August 12th, 2015, WHO has received reports of:
The current reported case fatality rate is approximately 36%
Recent outbreaks have included
Bottom Line:
MERS-CoV is significantly contagious respiratory virus with high lethality. It is spread primarily as an airborne virus, though the CDC currently recommends both standard contact and airborne precautions. There is currently no vaccine and only supportive treatment is advised.
Don’t be a vector or have your emergency department be a nidus of infection! Take appropriate precautions, including:
http://www.cdc.gov/coronavirus/mers/about/index.html
http://www.cdc.gov/coronavirus/mers/infection-prevention-control.html
http://www.who.int/csr/don/18-august-2015-mers-saudi-arabia/en/
Category: Toxicology
Keywords: body stuffers, observation period (PubMed Search)
Posted: 8/20/2015 by Hong Kim, MD
(Updated: 2/8/2026)
Click here to contact Hong Kim, MD
People who hide illicit drugs can be classified in to three different types.
1. Body stuffers – people who ingest drugs that are poorly wrapped to “eliminate” evidence from police – e.g. street dealers.
2. Body packers – people who ingest large amounts of “well” packed drug packets to transport drugs (usually internationally) – aka “mule.”
3. Body pushers – people hiding drugs in rectum or vagina.
Body stuffers are more frequently encountered in local ED compared to body packers. Stuffers can become symptomatic as the ingested drugs (cocaine, heroin, amphetamines) are often poorly wrapped (e.g. in plastic bag/wrap, cellophane paper, aluminium oil, etc.).
Recent retrospective article looked at the utility of 6-hour observation period in the ED as a management strategy for body stuffers. (n=126)
Characteristics
1. Ingested drugs (self-reported): heroin (48%), cocaine (46%), other drugs [cannabis, MDMA, diazepam, methamphetamine] (16%), unknown (8%)
2. Time of ingestion to ED presentation
Clinical findings
76% of the patients experience clinical signs of toxidrome at time of presentation.
Most common findings:
Patients who ingested heroin were more symptomatic vs. cocaine (87% vs. 70%)
Patients were discharged:
Conclusion
Yamamoto T et al. Management of body stuffers presenting to the emergency department. Europ J Emerg Med. May 8 [Epub ahead of print] PDIM: 25969343
Category: Critical Care
Keywords: ventilation, prvc (PubMed Search)
Posted: 8/18/2015 by Feras Khan, MD
(Updated: 2/8/2026)
Click here to contact Feras Khan, MD
Pressure Regulated Volume Control (PRVC)
Here are some basic pearls about PRVC Ventilation
Benefits: minimum PIP, guaranteed tidal volume, patient can trigger more breaths, improved oxygenation, breath by breath changes
Category: Visual Diagnosis
Posted: 8/17/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
55 year-old male presents with chest pain. Echo is shown below (parasternal long-axis on the left and aortic root / ascending aorta on the right), what's the diagnosis?
Follow me on Twitter (@criticalcarenow)
Category: Toxicology
Keywords: flumazenil, benzodiazepine, overdose (PubMed Search)
Posted: 8/7/2015 by Bryan Hayes, PharmD
(Updated: 8/13/2015)
Click here to contact Bryan Hayes, PharmD
Flumazenil is generally avoided in most adult patients with suspected benzodiazepine overdose due to resedation, seizures/withdrawal, inconsistent reversal of respiratory depression, and the potential for proconvulsant coingestants.
Three relatively recent poison center studies have attempted to demonstrate the safety of flumazenil in this setting. [1-3] In the first study there were 904 adult patients with 13 reported seizures and 1 death. [1] A second study specific to pediatric patients reported 83 patients with no seizures and no deaths. [2] A third study found 80 patients with 1 seizure and 0 deaths. [3]
On the surface, it may appear that flumazenil is safe to give. But, retrospective poison center studies from voluntary reporting cannot be used to prove a drug's safety. The true denominator is unknown. In the pediatric study, we wouldn't expect children to experience withdrawal since they aren't on chronic benzodiazepine therapy. [2] So, it's no surprise there weren't any seizures or deaths.
A recent systematic review and meta-analysis of randomized trials summed it up perfectly: "Flumazenil should not be used routinely, and the harms and benefits should be considered carefully in every patient." [4] Cases in which to consider flumazenil are pediatric patients and reversal of procedural sedation if needed.
Follow me on Twitter (@PharmERToxGuy) and Google Plus (+bryanhayes13)
Category: Neurology
Keywords: insular ribbon sign, MCA stroke, early CT sign of stroke (PubMed Search)
Posted: 8/12/2015 by WanTsu Wendy Chang, MD
(Updated: 10/14/2015)
Click here to contact WanTsu Wendy Chang, MD
Neuroimaging Tip - Loss of the Insular Ribbon Sign
Category: Critical Care
Posted: 8/11/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Is It Really ARDS?
Guerin C, et al. The ten diseases that look like ARDS. Intensive Care Med 2015; 41:1099-1102.
Category: Visual Diagnosis
Posted: 8/10/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
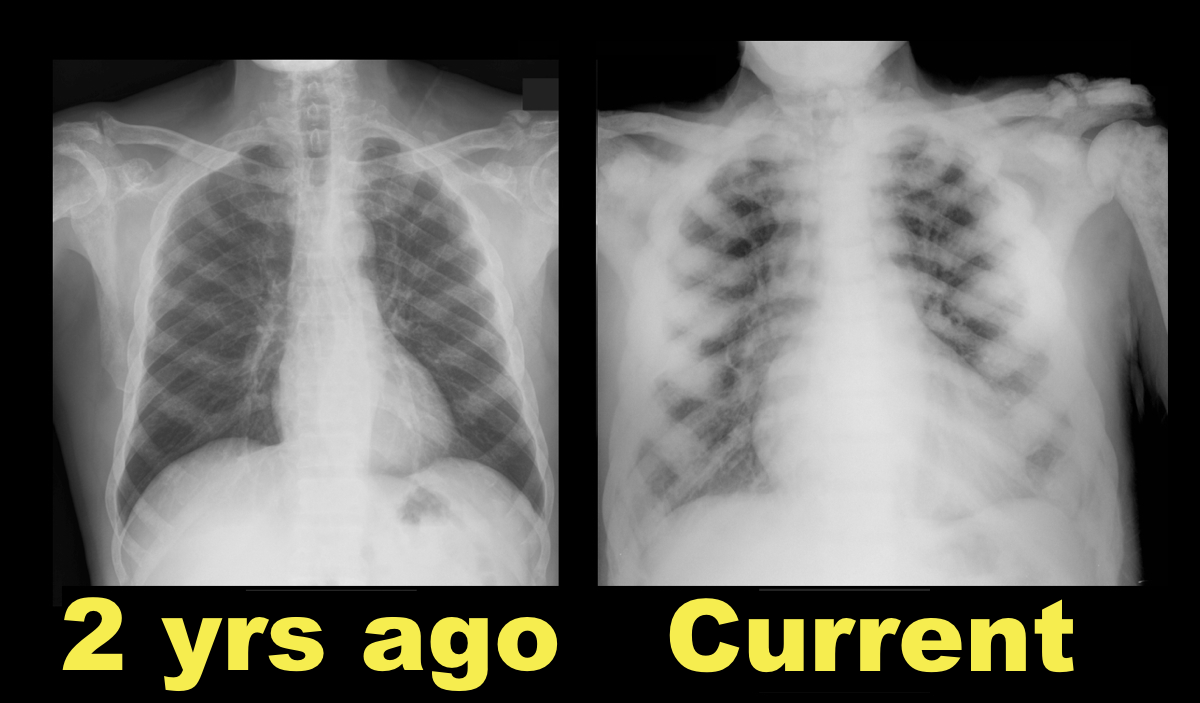
64 year-old male with no past medical history presents complaining of chronic weight-loss and diffuse chest pain; CXR is shown. What's the diagnosis and what other disease(s) may present similarly?

Sclerotic bone (osteoblastic) metastasis secondary to prostate cancer. The patient's CXR from 2 years prior is shown below for comparison.
Other malignancies associated with osteoblastic metastasis:
Follow me on Twitter (@criticalcarenow)
Category: Orthopedics
Keywords: Nerve, wrist (PubMed Search)
Posted: 8/8/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Handcuff Neuropathy
Compression of the superficial radial nerve against the radius.
Tends to occur with prisoners (too tight cuffs or person struggling)
Usually purely sensory lesion
Nerve regeneration can take 8 weeks (about an inch a month)
Document sensory exam to sharps or 2 point sensation.
DDx: De Quervain's, Carpal tunnel, Gamekeeper's thumb,
No need to splint
Category: Pediatrics
Keywords: pediatrics, ultrasound, pneumonia (PubMed Search)
Posted: 8/7/2015 by Jenny Guyther, MD
(Updated: 8/10/2015)
Click here to contact Jenny Guyther, MD
A recent meta-analysis published in Pediatrics reviews the diagnostic accuracy of lung ultrasound for pneumonia. According to the commentary, pneumonia is the leading cause of illness and death in children worldwide; it accounts for 18% of the total number of deaths in children <5 years, more than TB, AIDS, and malaria combined.
They performed a systematic search on several major databases using a combination of controlled keywords for age <18 years, pneumonia, and ultrasound. Of the initially 1475 identified studies, 8 were ultimately chosen for further evaluation.
Characterizing the meta-analysis:
- Three were conducted in the ED, 2 on the wards, 1 in the PICU and 2 in the NICU.
- Of the 765 children encompassed, the mean age was 5 years and they were 52% boys.
- Five of the 8 studies noted using highly skilled sonographers.
- The studies originated from Italy (5), US (1), China (1) and Egypt (1).
- All studies used CXR +/- clinical criteria as the diagnostic standard; LUS assessment was blinded to associated CXR results in 7 of 8 studies.
Results:
- LUS in the diagnosis of pediatric pneumonia had an overall pooled sensitivity of 96% (95% confidence interval [CI]: 94-97%) and specificity of 93% (95% CI: 90-96%).
- Positive and negative likelihood ratios were 15.3 (95% CI: 6.6-35.3) and 0.06 (95% CI: .03-0.11), respectively. For reference, remember that an LR >1 indicates an increased probability that the target disorder is present and >10 is a large or often conclusive increase in the likelihood of disease. Likewise, an LR <1 indicates a decreased probability that the target disorder is present and <0.1 is large or often conclusive decrease in the likelihood of disease.
- The area under the receiver operating characteristic (ROC) curve was 0.98. The ROC curve represents a measure of the accuracy of a test, >0.9 is considered to be excellent.
- In order to determine whether there are genuine differences underlying the results of the studies (heterogeneity) the I-squared statistic was implemented, with values consistent >0.45, demonstrating significant heterogeneity.
Bottom line: LUS appears to be an accurate test for the diagnosis of pneumonia in children. The limitation of this meta-analysis is mainly in the small number of studies and the significant heterogeneity between them, likely due at least in part to the fact that they used CXR +/- clinical data as the diagnostic standard. Nevertheless, the results provide evidence for the use of LUS as a cost-effective tool that potentially eliminates ionizing-radiation from the work-up of pediatric pneumonia and has application potential in resource-limited settings.
Pereda, Maria. "Lung Ultrasound for the Diagnosis of Pneumonia in Children: A Meta-analysis." Pediatrics 135.4 (2015): 714-22. Pediatrics. American Academy of Pediatrics. Web. 7 Aug. 2015.
Category: Toxicology
Posted: 8/6/2015 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Poison ivy, oak, and sumac (Toxicodendron sp) causes a highly puritic, allergic contact dermatitits (ACD) that affects between 10 and 50 million in the US every year. It is a significant occupational hazard as well a scourge for outdoor enthusiasts.
Toxicodendron species contain oleoresins, known as Urushiol compound, secreted by all parts of the plant. Contact with the oil usually occurs by brushing against or direct handling of the plant or contaminated items. This toxin triggers a type IV delayed hypersensitivity reaction in approximately 75% of the population. Within 12-24 hours an erythematous, often linear, vesicular rash develops but new lesions can occur up to 2 weeks later.
There is no ideal treatment for ACD induced by Toxicodendron species. Avoidance and barrier protection are the best strategies. Recommended medications include antihistamines, topical preparations, and systemic steroids. However, steroids require a 2-3 week course to prevent recrudescence of the rash and are not without undesirable side affects.
Zanfel, an OTC granular polyethlene paste, removes urushiol by binding with it to create an aggregate cluster that can be washed away with water. It is highly effective, providing rapid relief even as a sole agent but requires multiple initial applications and is expensive. Mean Green hand scrub has similar ingredients and is claimed to bond urushiol also. Excessive scrathing and abrasive scrubs can cause secondary cellulitis requiring antibiotics.
Category: International EM
Keywords: Low- and Middle-Income Countries, emergency care, burden of disease (PubMed Search)
Posted: 8/6/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Introduction
Obtaining quality information about emergency care in low- and middle-income countries (LMIC) is challenging. Data is sparse and often of low quality and the number of peer reviewed publications is limited.
In order to address this, Obermeyer et. al. just published in the WHO Bulletin a systematic review of emergency care in 59 low- and middle-income countries. In this article, the authors systematically reviewed 195 reports related to 192 facilities. The search included English or French articles from 1990 found within PubMed, CINAHL and World Health Organization (WHO) databases.
Burden of Emergency Care
Most articles were from emeregncy departments (EDs) in academically-affiliated hospitals in urban areas. Median mortality in the EDs was 1.8% (interquartile range, IQR: 0.2–5.1%), though in sub-Saharan Africa it was 3.4% (IQR: 0.5–6.3%). The median number of patients seen per year was 30,000 (IQR: 10 296–60 000). The facilities were staffed primarily by physicians-in-training or by physicians whose level of training was unspecified. There were very few providers specialized in emergency care.
Bottom Line
Based upon available data, there are high patient loads and mortality in LMIC- particularly in sub-Saharan Africa. This report highlights the importance of emergency care and the opportunity for systematic improvement to reduce mortality in these countries.
Reference: http://www.who.int/bulletin/volumes/93/8/en/
Category: Critical Care
Keywords: Anion gap, acidosis, metabolic acidosis, ingestion, critical care (PubMed Search)
Posted: 8/4/2015 by Daniel Haase, MD
Click here to contact Daniel Haase, MD
Ever forget all the things that make up MUDPILES in your AG acidosis differential?
Instead, consider the less-complicated mnemonic "KILR"!
K Ketoacidosis (diabetic, alcoholic, starvation)
I Ingestion (salicylate, acetaminophen, methanol, ethylene glycol, CO, CN, iron, INH)
L Lactic acidosis (infection, hemorrhage, hypoperfusion, alcohol, metformin)
R Renal (uremia)
Once you rule out the KLR causes, begin to consider ingestion or a tox source as your source. Remember that many of the listed ingestions can also cause a lactic acidosis.
For more acid/base pearls in greater detail:
http://lifeinthefastlane.com/ccc/anion-gap/
http://emcrit.org/wp-content/uploads/acid_base_sheet_2-2011.pdf (from emcrit.org)
Category: Pharmacology & Therapeutics
Keywords: blood glucose, dextrose, hypoglycemia (PubMed Search)
Posted: 7/26/2015 by Bryan Hayes, PharmD
(Updated: 8/1/2015)
Click here to contact Bryan Hayes, PharmD
How much does the blood glucose concentration increase when dextrose 50% (D50) is administered?
A new study found a median increase of 4 mg/dL (0.2 mmol/L) per gram of D50 administered.
This retrospective study was conducted in critically ill patients who experienced hypoglycemia while receiving an insulin infusion. While it may not directly apply to all Emergency Department patients, an estimation of the expected blood glucose increase from rescue dextrose is helpful. If the blood glucose doesn't respond as anticipated, it can help us troubleshoot possible issues (eg, line access).
Murthy MS, et al. Blood glucose response to rescue dextrose in hypoglycemic, critically ill patients receiving an insulin infusion. Ann Pharmacother 2015;49(8):892-6. [PMID 25986006]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: sulfonylurea, hypoglycemia, octreotide (PubMed Search)
Posted: 7/28/2015 by Hong Kim, MD
(Updated: 2/8/2026)
Click here to contact Hong Kim, MD
Oral hypoglycemic agents (e.g. sulfonylureas) can cause symptomatic hypoglycemia. Unlike metformin, sulfonylureas stimulate the release of insulin from beta-cells (in pancreas) in response to serum glucose level.
ED management of hypoglycemia involves:
However, for recurrent hypoglycemia (> 3 episodes of hypoglycemia), think about octreotide, rather than starting a dextrose (D5) infusion.
For example, D5 infusion at 150 mL/hour has only 7.5 gm of dextrose (calculation: D5% = 5gm/100 mL). One gram of dextrose contains about 4 calories (equivalent to one piece of Skittles) So, with a D5 infusion at 150 mL/hour, you are giving your patients 8 pieces of Skittles per hour. A bottle of Snapple lemon ice tea (non-diet) has more calories (150 calories in 16 oz. or 473 mL)!
Octreotide 50 mcg SQ (q6 hour) injection will decrease the insulin release from the beta-cell by blocking the voltage-gated Ca channel on the beta-cell.
All patient who received octreotide in the ED requires admission to the hospital for observation. Patients can be safely discharge from the hospital when finger stick glucose level remains normal for 24 hours after the last dose of octreotide.
Bottom line: In sulfonylrea-induced recurrent hypoglycemia, administer octreotide, rather than continuous infusion of dextrose (D5) solution.
Category: International EM
Keywords: Global burden of disease, international, non-communicable diseases, injuries (PubMed Search)
Posted: 7/29/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Every wonder what are the major global killers? Per the World Health Organization, the following were the top 20 causes.
Not unexpected, diseases primarily of the elderly, such ischemic heart disease, stroke and chronic obstructive pulmonary disease are on the top of the list. However, there are others, such as road traffic injuries and HIV/AIDS that could impact anyone.
| Top 20 Causes of Global Mortality, 2012 | ||||
| Rank | Cause | Deaths (000s) | % deaths | Deaths per 100,000 population |
| 0 | All Causes | 55859 | 100.0 | 789.5 |
| 1 | Ischaemic heart disease | 7356 | 13.2 | 104.0 |
| 2 | Stroke | 6671 | 11.9 | 94.3 |
| 3 | Chronic obstructive pulmonary disease | 3104 | 5.6 | 43.9 |
| 4 | Lower respiratory infections | 3052 | 5.5 | 43.1 |
| 5 | Trachea, bronchus, lung cancers | 1600 | 2.9 | 22.6 |
| 6 | HIV/AIDS | 1534 | 2.8 | 21.7 |
| 7 | Diarrhoeal diseases | 1498 | 2.7 | 21.2 |
| 8 | Diabetes mellitus | 1497 | 2.7 | 21.2 |
| 9 | Road injury | 1255 | 2.3 | 17.7 |
| 10 | Hypertensive heart disease | 1141 | 2.0 | 16.1 |
| 11 | Preterm birth complications | 1135 | 2.0 | 16.0 |
| 12 | Cirrhosis of the liver | 1021 | 1.8 | 14.4 |
| 13 | Tuberculosis | 935 | 1.7 | 13.2 |
| 14 | Kidney diseases | 864 | 1.6 | 12.2 |
| 15 | Self-harm | 804 | 1.4 | 11.4 |
| 16 | Birth asphyxia and birth trauma | 744 | 1.3 | 10.5 |
| 17 | Liver cancer | 740 | 1.3 | 10.5 |
| 18 | Stomach cancer | 733 | 1.3 | 10.4 |
| 19 | Colon and rectum cancers | 724 | 1.3 | 10.2 |
| 20 | Alzheimer's disease and other dementias | 701 | 1.3 | 9.9 |
http://www.who.int/healthinfo/global_burden_disease/estimates/en/index1.html
