Category: Critical Care
Posted: 7/28/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
It's July, that means new doctors are learning to do central-lines...here's a quick video with some quick pearls on how to do that. Enjoy!
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: x-ray, fracture, wrist (PubMed Search)
Posted: 7/26/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Triquetral fractures are the 2nd most common carpal fractures (scaphoid).
Dorsal surface most commonly.
Usually occur from impingement from the ulnar styloid, shear injury or from ligamentous avulsion.
XR: best seen on the lateral projection
http://images.radiopaedia.org/images/902179/42b3487baf4fb66183c51cd982477d_big_gallery.jpg
Remember this injury/radiographic appearance the next time you see an avulsion fracture dorsal to the proximal row of carpal bones on the lateral film but are unsure of the donor site.
Category: Pediatrics
Posted: 7/25/2015 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Post- streptococcal glomerulonephritis (PSGN) is an inflammatory reaction of the kidneys following infection with group A strep, and can occur sub clinically or have a severe presentation requiring admission, Nephrology consult, and careful management.
This diagnosis should be considered in any child between ages 2-12, or adults over 60, presenting with sudden unexplained hematuria or brown urine. Patients may also present with generalized edema secondary to urinary protein loss, hypertension, and acute kidney injury. Since kidney involvement usually trails the throat injection by 2-3 weeks or more, the patient and their family may not relate the two symptoms. A previous or current diagnosis of strep throat is not necessary to consider a patient for PSGN, since they may test negative by throat culture at the time of urinary and renal symptoms
When considering this diagnosis, the EM physician should order the following lab tests:
- Urinalysis (for casts and protein)
- Creatinine
- ASO Titer (or full streptozyme assay of 5 tests including ASO)
- Complement C3, C4, C50
Treatment is primarily supportive, and many cases will be mild enough to discharge home with pediatrician or Nephrology follow up. However, some cases may warrant admission for AKI, pulmonary edema, or cerebral edema. Edema can be managed with sodium restriction and loop diuretics. Hypertension can be managed with anti hypertension medications.
Renal biopsy can confirm the diagnosis with the presence of epithelial crescents in the glomeruli, but this is only necessary in severe cases where it is important to determine the etiology of the nephritis.
Eison TM, et al. Post-streptococcal acute glomerulonephritis in children: clinical features and pathogenesis. Pediatr Nephrol 2011; 26:165-180.
Category: Neurology
Keywords: antiplatelet, stroke, MI, Eptifibatide (PubMed Search)
Posted: 7/22/2015 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Given the similarity in pathophysiology, pharmacologic treatments for ischemic stroke have been modeled after those for acute myocardial infarction, such as the use of antiplatelets and thrombolytic agents. Have you ever wondered, why don't we give glycoprotein IIb/IIIa inhibitors (GPIs) as well?
A Cochrane review answers this question; GPIs increase morbidity in acute ischemic stroke (in the form of intracranial hemorrhage), with no evidence of benefit (improvement in Rankin Scale).
The systematic review looked at randomized clinical trials of GPIs in patients with ischemic stroke of 6 hours or less, alone or in combination with thrombolytics.
Ciccone A, Motto C, Abraha I, et al. Glycoprotein IIb/IIIa Inhibitors for Acute Ischaemic Stroke. Cochrane Database Syst Rev. 2014;3
Category: Critical Care
Keywords: drowning, critical care, swimming, swim, water (PubMed Search)
Posted: 7/21/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
Care of Drowning Patients in the ED
Szpillman D et al. Current Concepts: Drowning. NEJM 2012;366:2102-2110.
Category: Visual Diagnosis
Posted: 7/19/2015 by Haney Mallemat, MD
(Updated: 7/20/2015)
Click here to contact Haney Mallemat, MD
81 year-old man was mowing the lawn and then felt a sudden pop, then pain in his left arm. What's the diagnosis and what's this sign called?
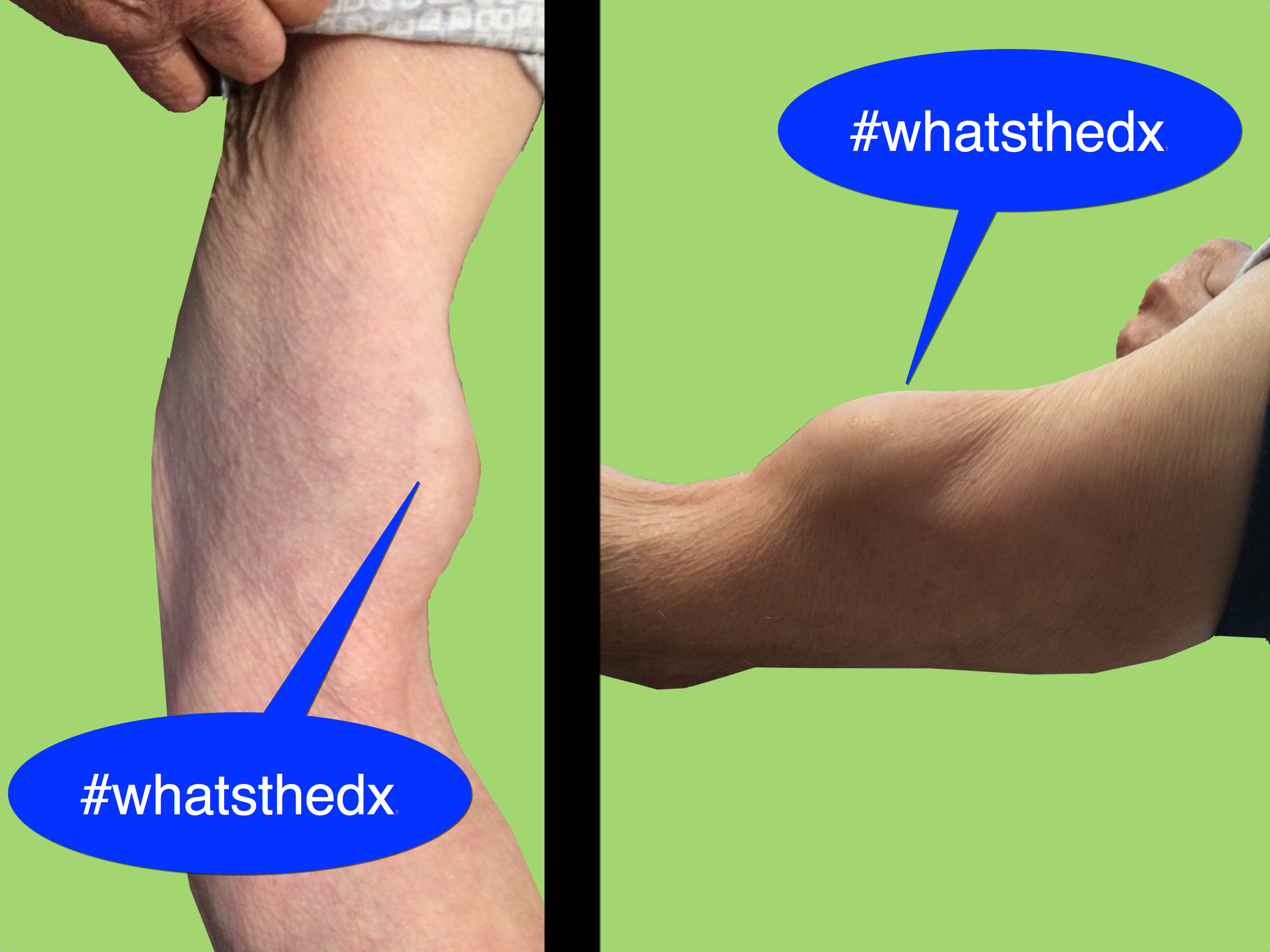
Biceps tendon rupture (BTR) aka Popeye's Sign
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 7/19/2015 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Opiates Causing Cardiac Toxicity
- Opiates are well known in their ability to cause sedation, euphoria, and respiratory depression, however are classically considered devoid of cardiac properties.
- Methadone a synthetic central-acting μ-opioid receptor agonist has been associated with dose-dependent QTc interval prolongation and torsade de pointes (TdP).
- Utilization of other less known drugs of abuse, specifically loperamide (peripherally acting μ-opioid receptor agonist) has been increasing in popularity.
- A surge in recent case reports has shown a potential causal association of loperamide with prolongation of the QTc interval and subsequent TdP.
- Toxic ingestion of loperamide leading to TdP has been successfully managed with standard TdP therapies (magnesium, isoproterenol, and pacing).
Marzec LN, Katz DF, Peterson PN, Thompson LE, Haigney MC, Krantz MJ. Torsade de pointes associated with high dose loperamide ingestion. J Innov Cardiac Rhythm Manage 2015; 6:1897–1899.
Marraffa JM, Holland MG, Sullivan RW, et al. Cardiac conduction disturbance after loperamide abuse. Clin Toxicol (Phila) 2014; 52:952–957.
Category: Orthopedics
Keywords: compartment syndrome, diagnosis (PubMed Search)
Posted: 7/18/2015 by Michael Bond, MD
Click here to contact Michael Bond, MD
Compartment Syndrome
Compartment syndrome is a diagnosis that needs to be made quickly in order to prevent long term muscle, nerve, and vascular compromise.
Two pieces of information are needed to determine if the patient has compartment syndrome.
Diastolic Pressure - Compartment pressure < 30 makes the diagnosis of compartment syndrome
So if a diastolic blood pressure is 80 and the compartment pressure is 40 the difference is 40 mmHg and the patient likely does not need a fasciotomy. The diagnosis can only be 100% onfirmed by a trip to the OR so these values should still be discussed with your local orthopaedist. When calling them just make sure you know both the DBP and the compartment pressure so that it can be interpreted correctly.
Category: Pediatrics
Keywords: Alvarado score, ultrasound (PubMed Search)
Posted: 7/17/2015 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Category: Toxicology
Keywords: physostigmine, anticholinergic toxicity, TCA overdose, asystole (PubMed Search)
Posted: 7/16/2015 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Physostigmine is a cholinergic agent (acetylcholine esterase inhibitor) that can be used to reverse anticholinergic toxicity. Its use has been declining since the publication of several case reports of physostigmine induced cardiac arrest in tricyclic antidepressant (TCA) overdose.
The first case report (and often cited) was by Pental P. et al. (Ann Emerg Med 1980), who presented 2 cases (32 and 25 year old) of asystole after administration of physostigmine (2 mg) in severe TCA overdose. These two cases both had widened QRS interval (120, 240 msec) due to TCA poisoning. Bradycardia preceded the asystole.
The second case report (Shannon M Pediatr Emerg Care 1998) reported a 15 year-old girl with QRS widening (120 msec) received 2 mg of physostigmine and developed severe bradycardia and then asystole.
Another case series (Knudson K et al. BMJ 1984) of 41 patients with overdose of maprotiline showed that physostigmine administration was associated with higher incidence of seizures. No asystole was noted.
Today physostigmine is contraindicated in TCA poisoning. But if we think about it, physostigmine administration probably wasn’t a good idea in the first place. Correcting anticholinergic toxicity of TCA has limited benefit; mortality from TCA overdose is usually associated with cardiac toxicity (Na-channel blockade) and should be treated with NaHCO3 administration
Physostigmine still has a role in treating isolated anticholinergic toxicity (e.g. diphenhydramine, benztropine, dimenhydrinate, scopolamine, jimson weed overdose). Prior to physostigmine administration:
Bottom line: If you suspect isolated anticholinergic toxicity, think about physostigmine. Like any medication, risk and benefit of administration should be considered prior to administration.
Category: International EM
Keywords: Tuberculosis, infectious disease, drug resistance, treatment (PubMed Search)
Posted: 7/15/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
Tuberculosis (TB) remains a deadly scourge killing approximately 1.5 million each year (see Pearl from 7/2/2105). Recognition by astute clinicians in the emergency department is key, as there is no readily available rapid test.
Current testing options:
1) Tuberculin skin test (also known as the Mantoux tuberculin skin test). A small amount of fluid (tuberculin purified protein derivative) is placed intradermally, usually in the left forearm. A positive test means the person was infected with TB. (Alternatively, if they grew up outside the US, they could have been vaccinated with Bacillus Calmette–Guérin or BCG.) A positive test is determined by the size of the reaction, but this can vary depending on the patient’s immune status.
2) Two interferon-gamma release assays or IGRA blood tests are approved for TB. While not readily available in all institutions, this is the preferred method for someone vaccinated with BCG.
Diagnosis of TB disease is based upon:
Treatment:
TB treatment depends on the susceptibility of the organism and the immune status of the patient. For a susceptible organism in a non-HIV patient, the first-line anti-TB agents regimens include
Typical treatment has an initial phase of 2 months, followed by a choice of several options for the continuation phase of either 4 or 7 months. Further information can be found at the CDC website on tuberculosis
Bottom Line
As stated previously, in the emergency department, maintain a strong clinical awareness for tuberculosis for someone with night sweats, cough, chest pain, and intermittent fever lasting for 3 weeks or longer. In particular, consider this diagnosis for someone from a low- or middle-income country or if he or she is HIV positive.
http://www.cdc.gov/tb/topic/testing/default.htm
http://www.cdc.gov/tb/publications/factsheets/testing/diagnosis.htm
http://www.cdc.gov/tb/publications/factsheets/treatment/treatmenthivnegative.htm
Category: Critical Care
Posted: 7/14/2015 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Blood Pressure Management in Severe Preeclampsia
Leone M, Einav S. Severe preeclampsia: what's new in intensive care? Intensive Care Med 2015; 41:1343-6.
Category: Visual Diagnosis
Posted: 7/13/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
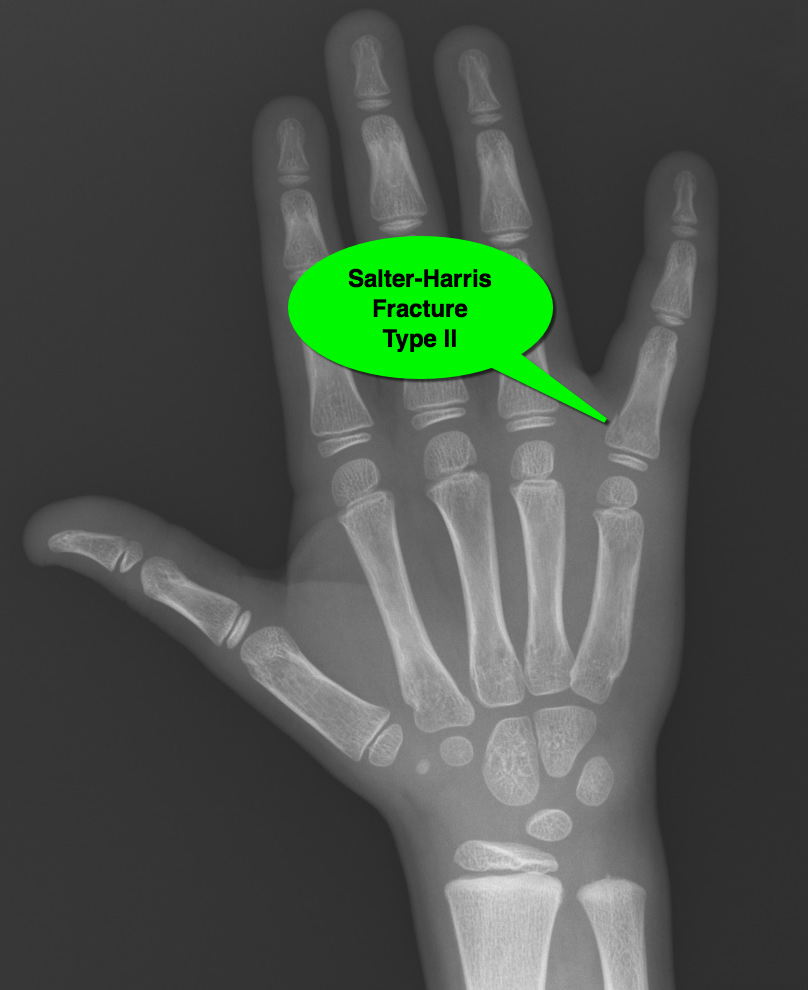
7 year-old male "jammed" 5th finger while playing basketball with pain and swelling over finger. What's the diagnosis?

Salter-Harris fracture (type II):
Salter-Harris Fracture (remember mnemonic SALTR)
For more on Salter-Harris fractures, check out this and that
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: Hernia, abdominal pain (PubMed Search)
Posted: 7/11/2015 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
A sports hernia is a painful musculotendinous injury to the medial inguinal floor.
It is the result of repetitive eccentric overload to the abdominal wall stabilizers of the pelvis.
It is common in sports that require sudden changes of direction or intense twisting movements.
Despite the term "hernia" in the title, it is not a true hernia as there is no "herniation" of abdominal contents
http://www.ssorkc.com/wp-content/uploads/2014/09/publagia.gif
Figure description: The upward and oblique pull of the abdominal muscles on the pubis fights against the downward and lateral pull of the adductors on the inferior pubis. This imbalance of forces can lead to injury.
PE: Evaluation of other GU/GYN/other intra-abdominal pathology comes first.
Clinician may note tenderness of the pubic ramus and medial inguinal floor.
Pain is more severe with resisted hip adduction and with resisted sit-up.
Combining these maneuvers (resisted situp while adducting hips) recreates the pathophysiology described above and is a good exam maneuver.
Sports hernia: the experience of Baylor University Medical Center at Dallas
Proc (Bayl Univ Med Cent). 2011 Apr; 24(2): 89 91
Category: Toxicology
Keywords: dabigatran, bleeding, idarucizumab, reversal (PubMed Search)
Posted: 7/6/2015 by Bryan Hayes, PharmD
(Updated: 7/9/2015)
Click here to contact Bryan Hayes, PharmD
The New England Journal of Medicine and Lancet both published studies evaluating idarucizumab for reversal of dabigatran. It is a monoclonal antibody fragment that binds dabigatran with high affinity. Dr. Ryan Radecki summarizes the two articles on his EM Lit of Note blog.
Here are a few take home points from these early studies:
Pollack CV, et al. Idarucizumab for dabigatran reversal. N Engl J Med. 2015 Jun 22. [Epub ahead of print, PMID 26095746]
Glund S, et al. Safety, tolerability, and efficacy of idarucizumab for the reversal of the anticoagulant effect of dabigatran in health male volunteers: a randomised, placebo-controlled, double-blind phase 1 trial. Lancet. 2015 Jun 15. [Epub ahead of print, PMID 26088268]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Neurology
Keywords: CSF shunts, VP shunt, VA shunt, LP shunt (PubMed Search)
Posted: 7/8/2015 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Cerebrospinal Fluid (CSF) Shunts
Follow me on Twitter @EM_NCC
Category: Visual Diagnosis
Posted: 7/6/2015 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
15 year-old female field hockey player presents with left shoulder pain. Besides fatigue over several weeks, she has no past medical history and there is nothing remarkable on physical exam. What's the diagnosis?
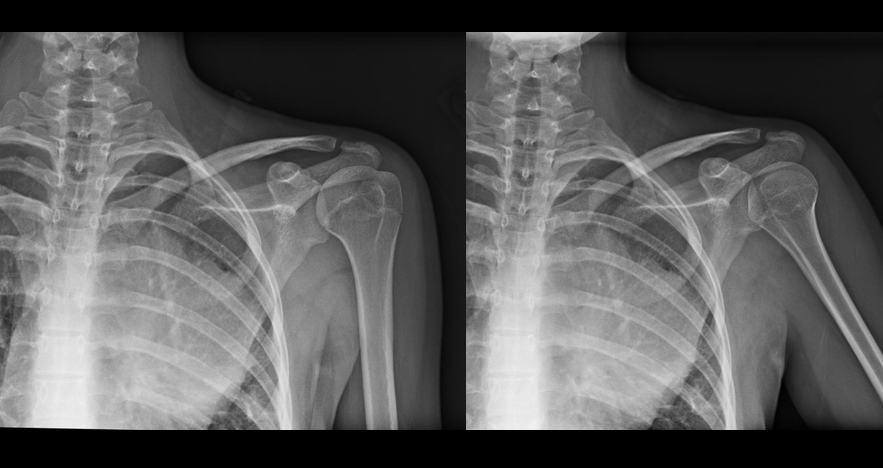
Mediastinal mass (lymphoma confirmed on biopsy)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Pharmacology & Therapeutics
Keywords: diabetic ketoacidosis, insulin, glargine, DKA (PubMed Search)
Posted: 6/29/2015 by Bryan Hayes, PharmD
(Updated: 7/4/2015)
Click here to contact Bryan Hayes, PharmD
Transitioning Diabetic Ketoacidosis (DKA) patients off an insulin infusion can be challenging. If a long-acting insulin, such as glargine or levemir, is not administered at the correct time to provide extended coverage, patients can revert back into DKA.
Pilot Study
A prospective, randomized, controlled pilot study in 40 patients evaluated administration of glargine within 2 hours of insulin infusion initiation compared to waiting until the anion gap (AG) had closed.
What they did
What they found
Mean time to closure of AG, mean hospital LOS, incidents of hypoglycemia, rates of ICU admission, and ICU LOS were all similar between the groups.
Application to Clinical Practice
Although just a pilot study (using a convenience sample), early glargine administration seemed to be absorbed adequately (based on time to AG closure) and was not associated with increased risk of hypoglycemia. If confirmed in a larger study, this technique could help optimize care of DKA patients in the ED by eliminating the often-mismanaged transition step later on.
Doshi P, et al. Prospective randomized trial of insulin glargine in acute management of diabetic ketoacidosis in the emergency department: a pilot study. Acad Emerg Med 2015;22(6):657-62. [PMID 26013711]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: International EM
Keywords: Tuberculosis, infectious diseases (PubMed Search)
Posted: 7/2/2015 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
As noted in a previous pearl (see 1/7/2015), tuberculosis (TB), caused by Mycobacterium tuberculosis, is the second greatest infectious killer after HIV/AIDS globally. While the incidence and death rate from TB is decreasing, it is still a widespread problem.
Mycobacterium tuberculosis primarily attacks the lungs. However, it can attack any part of the body such as the kidney, spine, and brain. TB is primarily spread person to person through the air, for example when a person with TB coughs, sneezes, speaks, or sings.
Once a person is infected with TB, the likelihood of developing disease is greater if the person:
Classic symptoms for pulmonary TB include:
Other TB symptoms can also include:
Bottom line
In the emergency department, maintain a strong clinical awareness for tuberculosis for someone with night sweats, cough, chest pain, and intermittent fever lasting for 3 weeks or longer. In particular, consider this diagnosis for someone from a low- or middle-income country or if he or she is HIV positive.
Next time: Testing and treatment for TB.
Also see prior pearls on TB: Multidrug Resistant Tuberculosis (MDR TB) (1/21/2015), Tuberculosis (1/7/2015); XDR Tuberculosis (8/14/2013); PPD positive? Good news... (2/6/2013)
http://www.cdc.gov/tb/topic/basics/default.htm
http://www.who.int/mediacentre/factsheets/fs104/en/
http://emedicine.medscape.com/article/230802-overview
Category: Critical Care
Keywords: tlc, triple lumen, cordis, catheter, central line, icu, critical care (PubMed Search)
Posted: 6/30/2015 by Feras Khan, MD
Click here to contact Feras Khan, MD
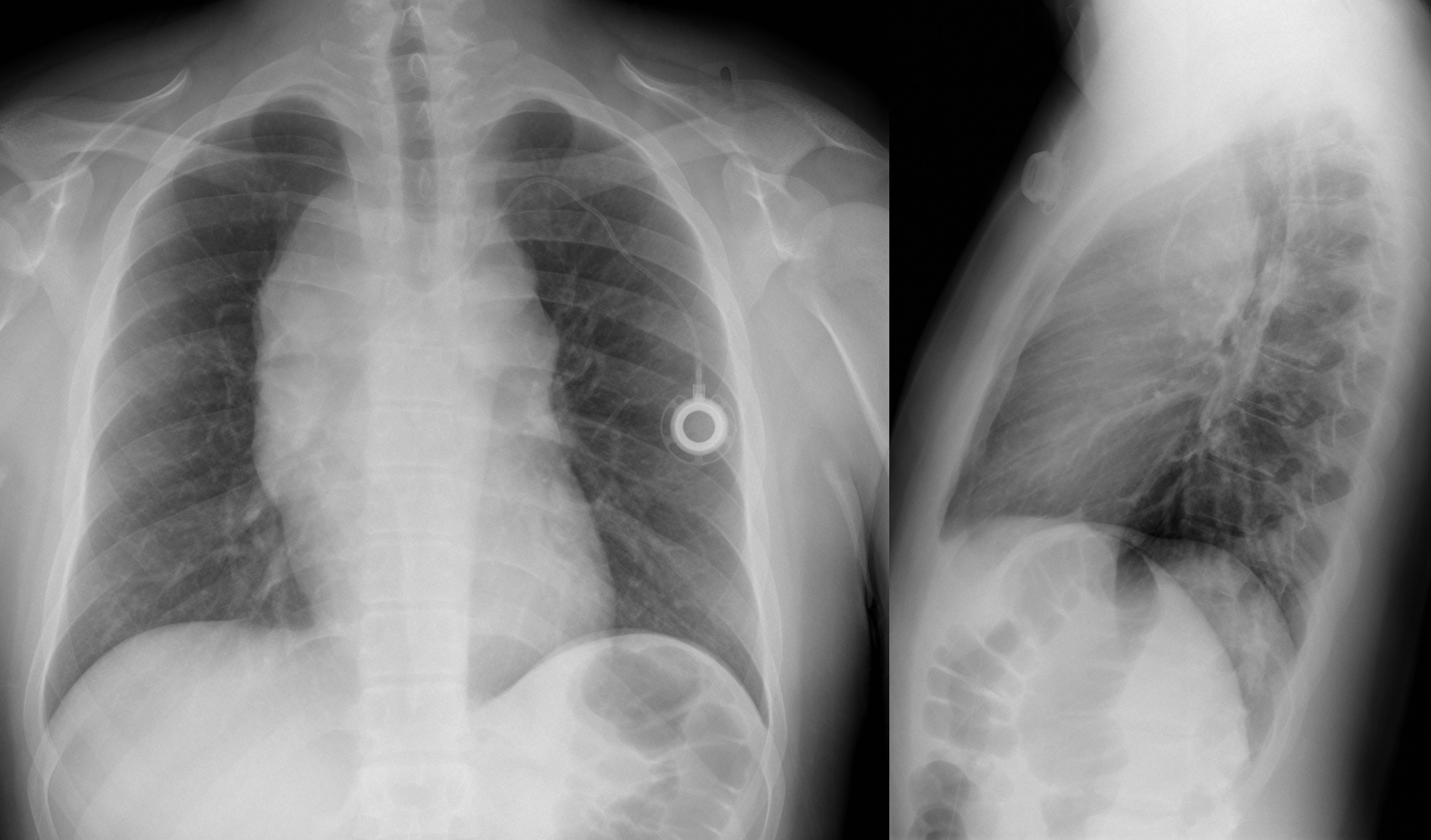
With a new academic year starting, it is important to review some details on central lines
Complications of central lines (TLC-Triple lumen catheter)
Avoiding infections: hand hygiene, chlorhexidine skin antisepsis, maximal barrier precautions, remove unnecessary lines, full gown and glove w/ mask and sterile technique.
Catheter position: 16-18cm for Right sided and 18-20 cm for Left sided. But can vary based on height, neck length, and catheter insertion site. Approximate length based on these factors.
Flow rates: Remember that putting in a central line does not necessarily improve your flow rates in resuscitation
16 G IV: 220 ml/min
Cordis/introducer sheath: 126 ml/min
18 G IV: 105 ml/min
16G distal port TLC: 69 ml/min
Ports (Can vary with type of catheter)
1. Distal exit port (16G)
2. Middle port (18G)
3. Proximal port (18G)
Arterial puncture: hold pressure for 5 mins and evaluate for hematoma formation (harder for subclavian approach)
Arterial cannulation: Has decreased due to ultrasound use but if you do cannulate an arterial site, don’t panic. Don’t remove the line. You can check a blood gas or arterial pulse waveform to confirm placement. Call vascular surgery for open removal and repair or endovascular repair. You could potentially remove a femoral arterial line and hold pressure but seek vascular advice regarding possible closure devices to use after removal.
