Category: Visual Diagnosis
Keywords: Green urine, diuretic (PubMed Search)
Posted: 2/17/2018 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
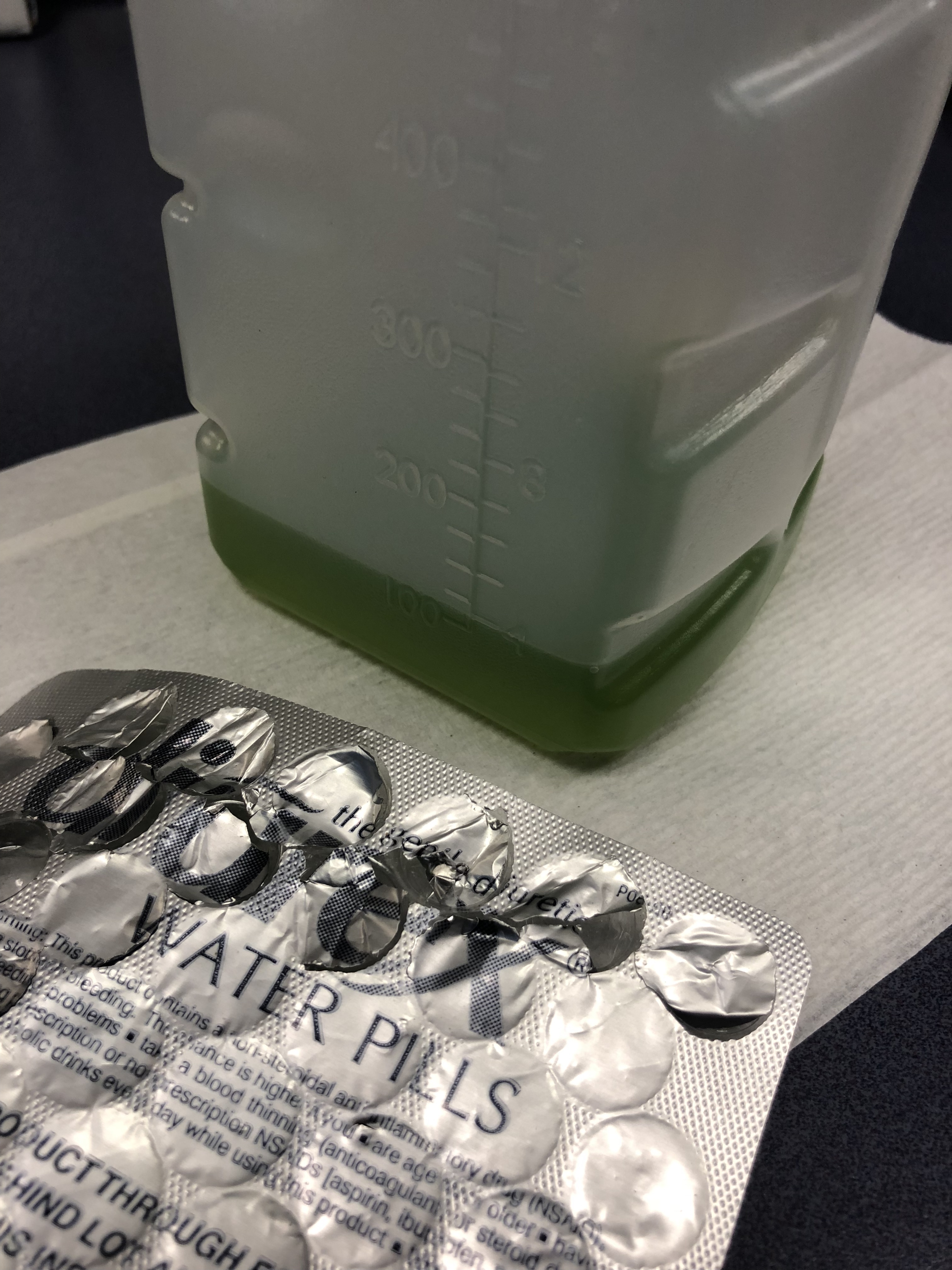
75 y/o M is brought in by EMS after he fell off the light rail and hit his head. In the ED he is A&Ox3, and is asking for a urinal. Two minutes later the tech comes running to show you the following:
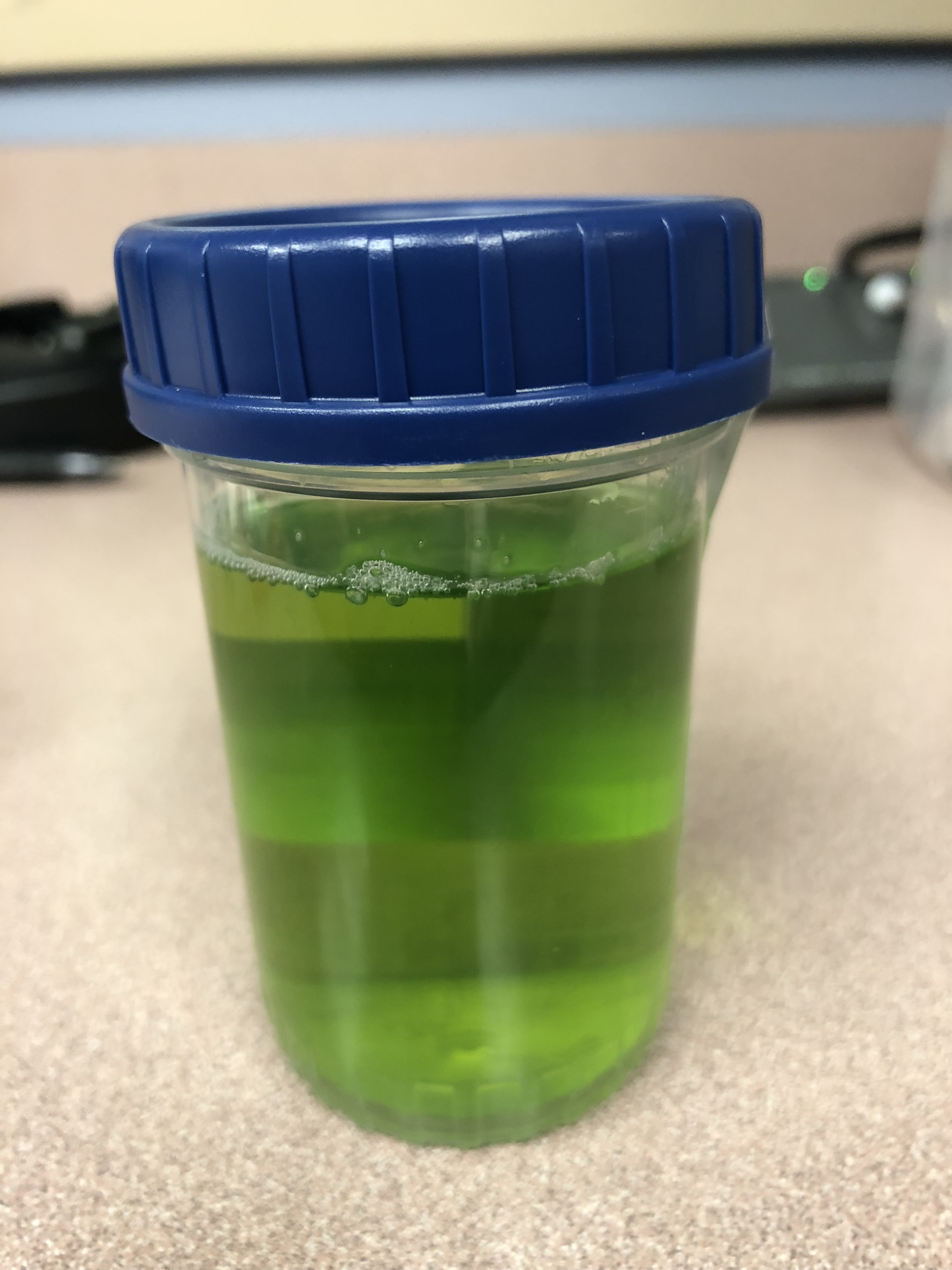
What is the cause of this patients Jolly Rancher Green Apple looking urine sample?
Answer:
Pamabrom side effect. Patient admitted to taking an “over the counter diuretic” called Diurex. The generic name is pamabrom. Pamabrom is a xanthine diuretic with only modest diuretic effect. It is marked mostly for weight loss to lose “water weight” and for relief of bloating during menstruation. A common side effect of the pills is a blue, green or golden discoloration of the urine. The capsules do not have the same side effect. The side effect is otherwise harmless and will disappear after stopping the diurex.
Category: Pediatrics
Keywords: foreign body, choking (PubMed Search)
Posted: 2/16/2018 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Patient: 11 month old with trouble breathing and color change after a family member sprayed air freshener. Symptoms have since resolved.
What are you concerned about in the attached xrays?
Answer: Radiolucent foreign body
Bilateral decubitus lateral films allow assessment of air trapping. The expectation is that the dependent lung will collapse partially in the normal patient. When a foreign body is present, there will be air trapping and hyperlucency in the dependent lung. In older patients, you can also obtain expiratory films to look for air trapping.
The patient had a food/mucus plug that was taken out of the right mainstem on bronchoscopy.
Foreign body aspiration is the 4th most common cause of accidental death in children younger than 3 years. Coughing and choking are the most common presenting symptoms.
CXRs are negative in > 50% of tracheal foreign bodies and 25% of bronchial foreign bodies.
More than 75% of foreign bodies in children less than 3 years are radiolucent.
Indirect signs of radiolucent foreign bodies include unilateral hyperinflation, atelectasis, consolidation and bronchiectasis (if presentation is delayed).
Bottom line: Consider bilateral lateral decubitus xrays in patients with a history concerning for foreign body.
Baram et al. Trachoebronchial Foreign Bodies in Children: The Role of Emergency Rigid Bronchoscopy. Global Pediatric Health. 2017: 1-5.
Category: Toxicology
Keywords: Cardiotoxicity, Bupropion, Ventricular dysrhythmia (PubMed Search)
Posted: 2/15/2018 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Bupropion (Wellbutrin, Zyban) is unique monocyclic antidepressant and smoking cessation agent that is structurally similar to amphetamines. Bupropion blocks dopamine and norepinephrine reuptake and antagonizes acetylcholine at nicotinic receptors.
Bottom line:
Bupropion is a common cause of drug induced seizures but in severe overdose can also cause prolonged QTc and wide complex ventricular dysrhythmia that may be responsive to sodium bicarbonate. All patients with an overdose of bupropion should have an ECG performed and cardiac monitoring to watch for conduction delays and life-threatening arrhythmias.
Wide complex tachycardia after bupropion overdose. Franco V. Am J Emerg Med. 2015 Oct;33 (10):1540.
Delayed bupropion cardiotoxicity associated with elevated serum concentrations of bupropion but not hydroxybupropion. Al-Abri SA, Orengo JP, et al. Clin Tox. 2013 Dec ;51(10):1230-4.
QRS widening and QT prolongation under bupropion: a unique cardiac electrophysiological profile. Caillier B. Pilote S. et al. Fundam Clin Pharmacol. 2012 Oct;26(5): 599-608.
Comparison of Resuscitative Protocols for Bupropion Overdose Using Lipid Emulsion in a Swine Model. Fulton LV, Fabrich RA, et al, Military Medicine 181, 5:482, 2016.
Category: Neurology
Keywords: occipital nerve block, migraine, headache (PubMed Search)
Posted: 2/14/2018 by WanTsu Wendy Chang, MD
(Updated: 2/15/2018)
Click here to contact WanTsu Wendy Chang, MD
Zhang H, Yang X, Lin Y, Chen L, Ye H. The efficacy of greater occipital nerve block for the treatment of migraine: a systematic review and meta-analysis. Clin Neurol Neurosurg. 2018;165:129-133.
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: Hip pain, athletes (PubMed Search)
Posted: 2/10/2018 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Femoral neck stress fractures
Adults>kids
Represents 5% of all stress fractures
Usually due to repetitive abductor muscle contraction
As with all stress fractures can occur in 2 types
1) Insufficiency type (normal physiologic stress on abnormal bone)
2) Fatigue type (abnormal/excessive physiologic stress on normal bone)
2 locations on interest:
1) Compression side (inferior femoral neck)
2) Tension side (superior femoral neck)
History: Insidious onset of groin or lateral hip pain associated with weight bearing
Exam: Antalgic gait, pain with hip log roll and with FABER (hip flexion, Abduction and external rotation test)
Treatment:
Compression side: reduced weight bearing and activity modification
Tension side: Non weight bearing (due to high risk of progression to displacement with limited weight bearing) AND surgical consultation for elective pinning to prevent displacement. If displaced, will require ORIF
Pevlis, hip and thigh injuries and conditions. Heidi Prather and Devyani Hunt. In Sports Medicine Study Guide and Review for Booards 2nd Edition. 2017
Category: Pediatrics
Keywords: Kawasaki's disease, SJS, TEN, dermatitis (PubMed Search)
Posted: 2/9/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Case: 5 year old presents to the ED with 2 weeks of fever. She has extensive cracked, bleeding lips and a rash on her hands and feet. She was recently diagnosed with “walking pneumonia” and hand, foot and mouth disease this week. Her pediatrician sent her in for further workup after she was found to have an elevated CRP on outpatient labs. A similar picture appears in the link below:
What's the diagnosis?
The diagnosis of Mycoplasma pneumonia-induced rash and mucositis (MIRM) was recently termed in the 2015 Journal of American Academy of Dermatology. It is characterized by mucocutaneous eruptions with prominent mucosal involvement. 94% of patients in the reviewed cases had extensive oral lesions that can range from erosions, ulcers or vesiculobullous lesions. 82% of patients had ocular involvement characterized by purulent bilateral conjunctivitis. In 63% of cases, patients were found to have urogenital lesions. Almost all of these patients had prodromal symptoms of cough and fever preceding the eruption by 1 week. The disease was found to be most prominent with young (11.9 ± 8.8 years) and with a 66% male predominance. The treatment is antibiotics such as azithromycin and oral corticosteroids with a minority of patients requiring IVIG. These patients have a good prognosis.
Bottom Line: Consider MIRM in patients with extensive mucosal disease that do not completely fit the criteria of Kawasaki’s or Stevens-Johnson Syndrome/ Toxic Epidermal Necrolysis.
Reference:
Canavan TN, Mathes EF, Frieden I, Shinkai K. Mycoplasma pneumoniae-induced rash and mucositis as a syndrome distinct from Stevens-Johnson syndrome and erythema multiforme: a systematic review. J Am Acad Dermatol. 2015
Feb;72(2):239-45.
Category: Critical Care
Posted: 2/6/2018 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Hyperoxia and the Post-Arrest Patient
Roberts BW, et al. Association between early hyperoxia exposure after resuscitation from cardiac arrest and neurological disability: a prospective multi-center protocol-directed cohort study. Circulation 2018; epub ahead of print.
Category: Geriatrics
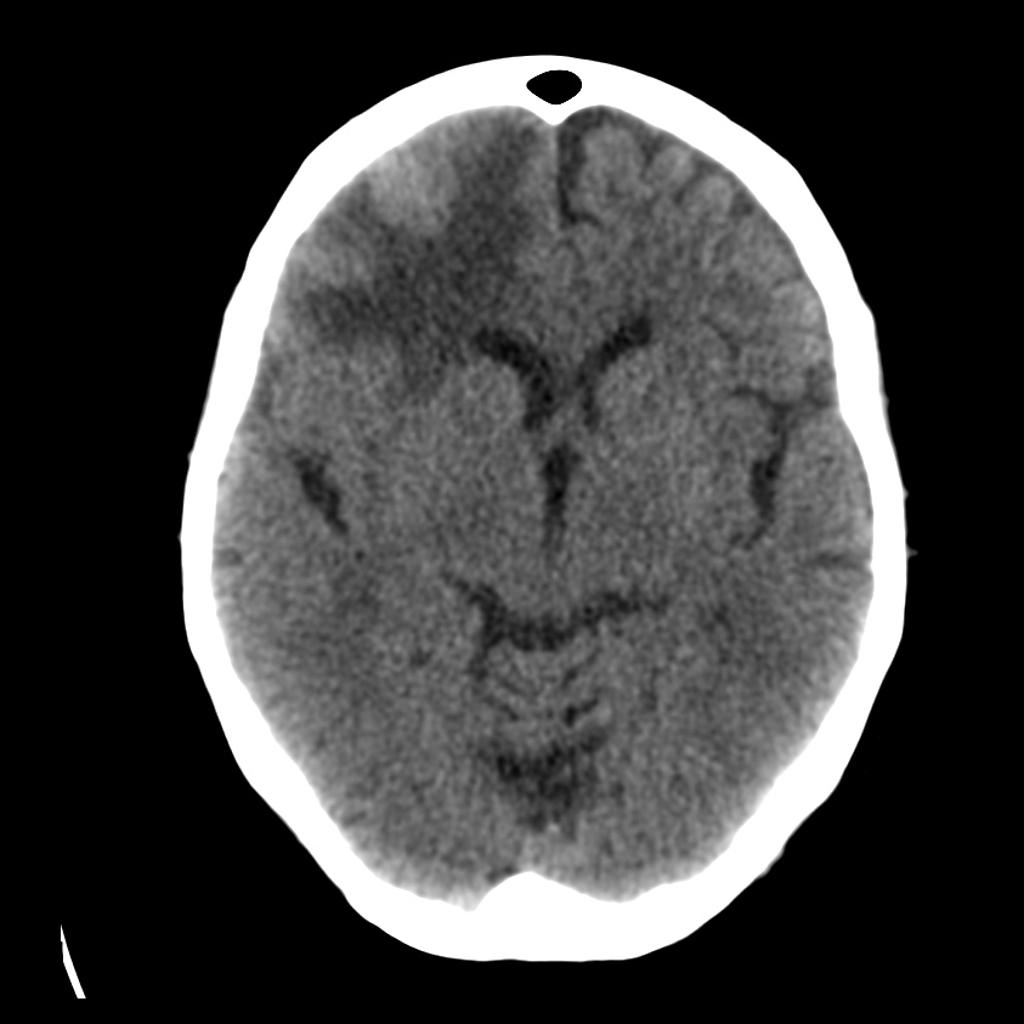
Keywords: dizziness, CT, MRI, Cerebellar (PubMed Search)
Posted: 2/5/2018 by Danya Khoujah, MBBS
(Updated: 2/7/2026)
Click here to contact Danya Khoujah, MBBS
15% of older adults presenting to ED for dizziness have serious etiologies; 4-6% are stroke-related and sensitivity of CT for identifying stroke or intracranial lesion in dizziness is poor (16%), so if CNS etiology suspected, seek neuro consult or MRI (83% sensitivity)
Lo AX, Harada CN. Geriatric dizziness: evolving diagnostic and therapeutic approaches for the emergency department. Clin Geriatr Med. 2013;29(1):181-204.
Category: Infectious Disease
Keywords: sepsis, pseudomonas (PubMed Search)
Posted: 2/3/2018 by Ashley Martinelli
(Updated: 2/7/2026)
Click here to contact Ashley Martinelli
Debating between cefepime or piperacillin/tazobactam for your septic patient? Use this table to help you decide.
|
|
| Cefepime | Piperacillin/Tazobactam |
| Gram Negative Spectrum | Pseudomonas aeruginosa | Yes | Yes |
| Aerobic gram negative organisms | E. coli Klebsiella sp. Proteus mirabilis M catarrhalis H. influenza | E. coli Klebsiella sp. Proteus mirabilis M. catarrhalis H. influenza | |
| Anerobic gram negative organisms | No | B. fragilis
| |
| Gram Positive Spectrum | MRSA | No | No |
| Aerobic gram positive organisms | MSSA CoNS Group A Strep S. pneumoniae
| MSSA CoNS Group A Strep S. pneumoniae E. faecalis | |
| Anaerobic gram positive organisms | P. acnes Peptostreptococci | P. acnes Peptostreptococci Clostridium sp. | |
| Infection Site Concerns | CNS Penetration | Yes | No1 |
| Urine Penetration | Yes | Yes | |
| Lung Penetration | Yes | Low2 | |
| Dosing Frequency (Normal Renal Function) | Q8h | Q6h | |
1. Tazobactam CNS penetration is limited, thus limiting antipseudomonal activity in the CNS
2. Low pulmonary penetration, may not achieve therapeutic levels in patients with critical illness
Take home points:
-Piperacillin/tazobactam differs in spectrum with its ability to cover enterococcus and anaerobes. Consider for sepsis with gastrointestinal source
-Cefepime can be used for CNS infections and readily achieves therapeutic concentrations in the lungs. Metronidazole can be added to ensure anaerobic organism coverage.
-Piperacillin/tazobactam should be dosed every 6 hours in patients with normal renal function to achieve therapeutic concentration.
1. Gilbert, D. N., Chambers, H. F., Eliopoulos, G. M., Saag, M. S., & Pavia, A. T. (2016). Sanford guide to antimicrobial therapy 2016. 46th edition. Sperryville, VA, USA: Antimicrobial Therapy, Inc.
2. Nau R, Kinzig-Schippers M, Sörgel F, et al. Kinetics of piperacillin and tazobactam in ventricular cerebrospinal fluid of hydrocephalic patients.?Antimicrobial Agents and Chemotherapy. 1997;41(5):987-991.
3. Felton T, McCalman K, Malagon I, et al. Pulmonary penetration of piperacillin and tazobactam in critically ill patients. Clinical pharmacology and therapeutics. 2014;96(4):438-448. doi:10.1038/clpt.2014.131.
4. Boselli E, Breilh D, Duflo F, et al. Steady-state plasma and intrapulmonary concentrations of cefepime administered in continuous infusion critically ill patients with severe nosocomial pneumonia. Critical Care Medicine.2003;31:2102-2106.
Category: Pediatrics
Keywords: Pediatrics, Abdominal Pain (PubMed Search)
Posted: 2/2/2018 by Megan Cobb, MD
Click here to contact Megan Cobb, MD
 Your patient is an18 months old female with intermittent abdominal pain for the last 4-5 days. She has history of constipation and soy allergy, seen at an outside hospital three days ago for the same. She had an xray and was discharged home with instructions for at home clean out with diagnosis of constipation.
Your patient is an18 months old female with intermittent abdominal pain for the last 4-5 days. She has history of constipation and soy allergy, seen at an outside hospital three days ago for the same. She had an xray and was discharged home with instructions for at home clean out with diagnosis of constipation.
Mother is bringing her to your ED because the pain is back. The laxatives helped somewhat, but her symptoms have returned. She reports that the patient cries spontaneously, lasting 1-2 minutes, then completely resolves. These episodes happen at multiple times during the day.
ROS: Decreased appetite and energy, but NO fevers, vomiting, diarrhea, bloody stool, abdominal distension, hematuria, or lethargy.
Intussusception classically presents with colicky abdominal pain, palpable mass, and currant jelly stools, but in less than 50% of patients. The clinical presentation of intussusception actually occurs on a spectrum. Children who present early in their course may look well with intermittent, unexplained crying episodes, while others may be febrile, dehydrated, with bloody stools, and be septic. The diagnosis can be missed in up to 60% of children presenting for initial evaluation. Identified risk factors include any syndrome or abnormality causing a lead point, ie Meckel's Diverticulum, Familial Polyposis, lymphoma and Henoch-Scholein Purpura, as well as GI infections, bacterial and viral, (Adenovirus, Rotavirus, and HHV6, etc.)
On exam, our patient's abdomen was soft but hard to evaluate due to behavior. Flat plate AXR demonstrated a circular hyperdensity in the RUQ, which on ultrasound, corresponded to a large ileocolic intussusception. She was successfully treated with air enema reduction, which in recent review has the lowest recurrence rate of intussusception.
Bottom Line -
In children with intermittent abdominal pain or unexplained crying episodes, consider intussusception on your differential, as more than half are missed on initial presentation, which can be subtle. Late presentations can include bowel perforation, peritonitis, sepsis, and shock. If diagnosed, arrange for enema reduction or transfer to a facility with this capability.
References:
Waseem M, Rosenberg HK. Intussusception. Pedi Emer Care. Nov 2008, 24(11): 793-800.
Gluckman S, Karpelowsky J, Webster AC, McGee RG. Management for intussusception in children. Cochrane Review of Systematic Databases. 2017; Issue 6.
Category: Toxicology
Posted: 2/1/2018 by Kathy Prybys, MD
(Updated: 2/2/2018)
Click here to contact Kathy Prybys, MD
47 year old woman presents with cough, headache, weakness, and low grade fever. Her symptoms have been present for several days. Vital signs are temperature 99.9 F, HR 96, RR 16, BP 140/88, Pulse Ox 98%. Physical exam is nonfocal. She is Influenza negative. She is treated with Ibuprofen and oral fluids. Upon discharge she mentions she is having difficulty hearing and feels dizzy. Upon further questioning she admits to ringing in her ears. What tests should you order?
ANSWER: Salicylate and Acetaminophen levels.
Patient admits to taking BC Powder, an over the counter medication to self treat over the past few days. The active ingredients of BC powder are 845 mg of aspirin and 65 mg of caffeine. Her salicylate level is 45 mg/dL. Her other labs are unremarkable. Serial salicylate levels should be obtained every 2-4 hours and correlated with blood pH and clinical findings.
Salicylates commonly cause of ototoxicity. Tinnitus and hearing loss are early signs of salicylate toxicity and occur between 20-45 mg/dL. Other CNS effects are vertigo, hyperventilation, delirium, seizure, lethargy, and coma. Salicylate and acetaminophen are contained in numerous over the counter medications and are often mistakenly considered safe by the public resulting in accidental overdose. Early signs of toxicity can be missed or confused with other illness with serious consequences.
American College of Medical Toxicology. Guidance Document: Management Priorities in Salicylate Toxicity. J Med Tox. 2015;11(1):149-152.
Emergency department management of the salicylate-poisoned patient. O'Malley GF. Emerg Med Clin North Am. 2007 May ;25(2):333-46.
Category: Critical Care
Keywords: sepsis, septic shock, glucocorticoids, steroids, hydrocortisone (PubMed Search)
Posted: 1/29/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
As hospital volumes increase and ED patient boarding becomes more commonplace, emergency physicians may find themselves managing critically ill patients beyond the initial resuscitation.
The benefit of glucocorticoids in critically ill patients with septic shock has remained a topic of controversy for decades due to conflicting studies, including the 2002 Annane trial and the 2008 CORTICUS trial, which had opposing results when it came to the mortality benefit of steroids.
The results of the eagerly-awaited ADRENAL trial, a multicenter randomized controlled trial investigating the benefit of steroids in septic shock, were released earlier this month:
Take Home Points:
1. Administration of standard daily dose hydrocortisone by infusion does not seem to affect mortality in septic shock.
2. Emergency providers should continue to consider stress-dose steroids in patients with shock and a high risk of adrenal insufficiency (e.g., chronic steroid therapy, genetic disorders, infectious adrenalitis, etc).
Category: Orthopedics
Keywords: Dental avulsion, tooth, trauma (PubMed Search)
Posted: 1/27/2018 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Dental Avulsion in the field/sporting event
- Only replace avulsed secondary teeth
- Handle the tooth by the crown only
- Rinse tooth with cold running water gently (the root should not be wiped)
- Immediate attempt to reimplant permanent tooth into socket by 1st capable person:
* Time is tooth: Each minute tooth is out of socket reduces tooth viability by 1%
* Best chance of success if reimplant done within 5–15 min*? Poor tooth viability if avulsed for >1 hr
- If unsuccessful, place tooth in a transport solution (from most to least desirable):
- Hanks balanced salt solution (HBSS)
* Balanced pH culture media available commercially in the Save-A-Tooth kit
* Effective hours after avulsion
- Cold milk:
* Best alternative storage medium
* Place tooth in a container of milk that is then packed in ice (prevents dilution)
- Saliva:
* Store in a container of parent or child's saliva
- Never use tap water or dry transport
Category: Neurology
Keywords: edema, hemorrhage, tumor, CT, MRI, contrast (PubMed Search)
Posted: 1/24/2018 by Danya Khoujah, MBBS
(Updated: 2/7/2026)
Click here to contact Danya Khoujah, MBBS
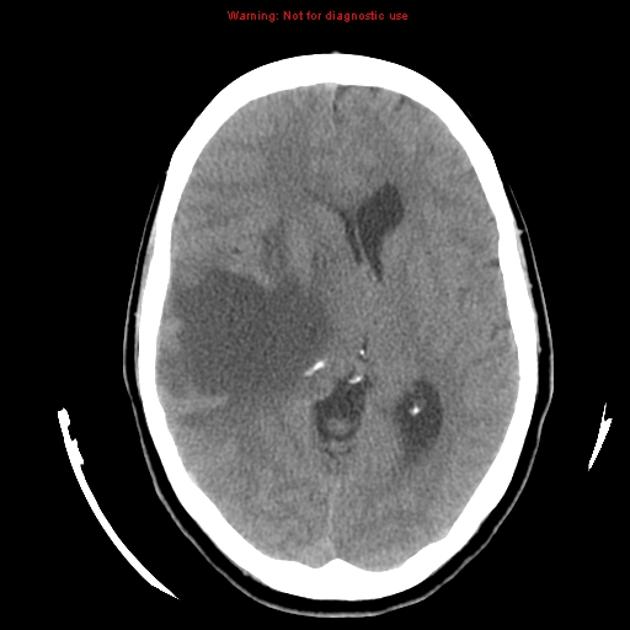

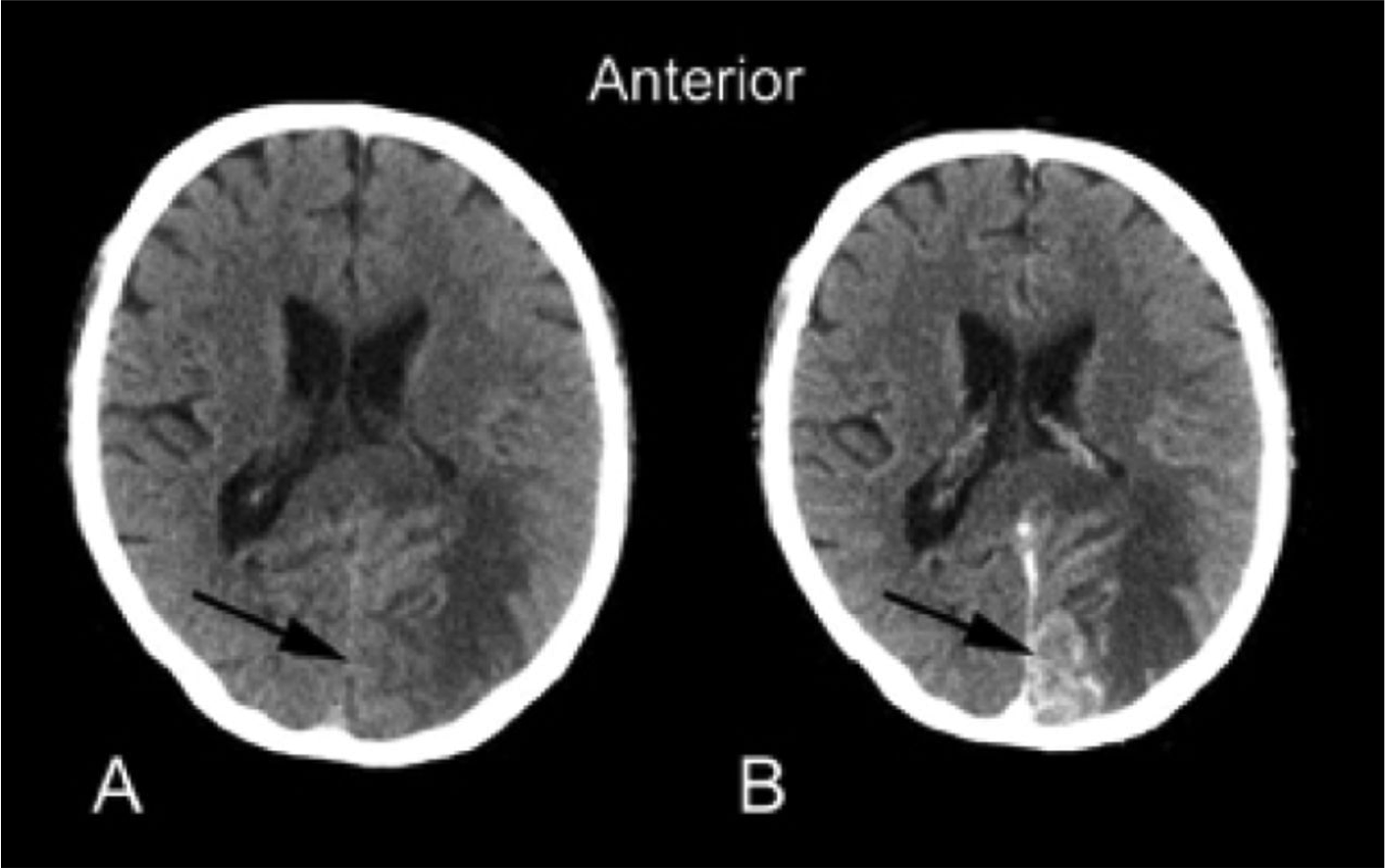
Klein JP, Dietrich J. Neuroradiologic Pearls for Neuro-oncology. Continuum 2017;23(6):1619-1634.
Category: Pediatrics
Keywords: Pain control in children, opiates, NSAIDS, motrin, orthopedic (PubMed Search)
Posted: 1/19/2018 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Bottom line: Oral morphine was not superior to ibuprofen and both drugs decreased pain with no difference in efficacy. Morphine was associated with more adverse events.
Poonai et al. Oral Morphine versus ibuprofen administered at home for postoperative orthopedic pain in children: a randomized controlled trial. CMAJ 2017. 189: E1252-E1258.
Category: Toxicology
Keywords: Liver dialysis, MARS (PubMed Search)
Posted: 1/18/2018 by Kathy Prybys, MD
(Updated: 1/19/2018)
Click here to contact Kathy Prybys, MD
Acute liver failure carries a high morbidity without liver transplantation. Liver support systems can act as “bridge” until an organ becomes available for the transplant procedure or until the liver recovers from injury. Artificial liver support systems temporally provide liver detoxification utilizing albumin as scavenger molecule to clear the toxins without providing synthetic functions of the liver (coagulation factors). One of the most widely used devices is the Molecular Adsorbent Recirculating System (MARS).This system has 3 different fluid compartments: blood circuit, albumin with charcoal and anion exchange column, and a dialysate circuit that removes protein bound and water soluble toxins with albumin.
Bottom Line
MARS therapy could be a potentially promising life saving treatment for patients with acute poisoning from drugs that have high protein-binding capacity and are metabolized by the liver, especially when concomitment liver failure. Consider consultation and transfer of patients to liver center.
The Molecular Adsorbent Recirculating System (MARS®) in the Intensive Care Unit: A Rescue Therapy for Patients with Hepatic Failure. F Saliba, Critical Care 10.1 (2006): 118.
Category: Orthopedics
Keywords: Head injury, concussion, sideline (PubMed Search)
Posted: 1/13/2018 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Concussion – Where are we now?
The Sport Concussion Assessment Tool 5th edition (SCAT 5) was released in 2017
It is a standardized tool to assist health care professionals in the evaluation of sport associated concussions
It should be used for those 13 years and older (there is a child version for younger athletes)
Print and bring to the sideline for your next coverage event!
http://bjsm.bmj.com/content/bjsports/early/2017/04/26/bjsports-2017-097506SCAT5.full.pdf
Some points to consider:
It should take at least 10 minutes to complete. Any less and you may not be performing the test correctly
The SCAT5 is the standard tool used in concussion assessment in the NCAA and NFL and other professional sports
Some symptoms of concussion appear over time. For example, an athlete may have zero or minimal symptoms immediately after yet be considerably symptomatic in 10 to 15 minutes.
-Follow up screening evaluations are essential even in those with a negative initial sideline screening test
The SCAT5 should be used immediately after injury
-Utility decreases post injury after days 3-5
-The included symptom checklist has utility in tracking recovery
-Attempt to perform in an environment free of distractions (crowd noise, bad weather)
The clinical utility of the SCAT5 can be enhanced by adding assessment of other factors such as reaction time, balance assessment, video-observable signs (if available) and oculomotor screening.
Category: Pediatrics
Posted: 1/12/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: activated charcoal, large acetaminophen overdose, NAC dose (PubMed Search)
Posted: 1/11/2018 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Acetaminophen (APAP) overdose is the leading cause of liver failure in the U.S. and Europe. Large APAP ingestion can result in hepatotoxicity despite the early initiation of n-acetylcysteine (NAC).
A recently published study from Austrialia investigated the effect of activate charcoal and increasing the NAC dose for large APAP overdose patients (3rd bag: 100 to 200 mg/kg over 16 hours) during first 21 hours of NAC therapy
acetaminophen ratio (first APAP level taken between 4 to 16 hour post ingestion / APAP level on the Rumack nomogram line at that time point) was determined to compare APAP levels at different time points among study sample
e.g.
first APAP level at 4 hour post ingestion = 400
APAP level on the Rumack APAP nomogram at 4 hour post ingestion = 150
APAP ratio = 400/150 = 2.67
Findings:
Conclusion:
Note: Any increase in NAC dosing from the standard 21 hour therapy should be performed after consulting your regional poison center.
Chiew AL et al. Massive paracetamol overdose: an obsevational study of the effect of activated charcoal and increased acetylcysteine dose (ATOM-2). Clin Toxicol 2017;55:1055-1065. PMID: 28644687.
Category: Neurology
Keywords: RCVS, thunderclap headache, migraine, SAH (PubMed Search)
Posted: 1/10/2018 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider RCVS in the differential of thunderclap headache and in patients who present with worse than usual migraine headache.
Arrigan MT, Heran MKS, Shewchuk JR. Reversible cerebral vasoconstriction syndrome: an important and common cause of thunderclap and recurrent headaches. Clin Radiol. 2017 Dec 21 [Epub ahead of print]
Follow me on Twitter @EM_NCC
