Category: Geriatrics
Keywords: guidelines, protocols, safety, delirium (PubMed Search)
Posted: 7/1/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Based in part upon Geriatric Emergency Department Guidelines, the American College of Emergency Physicians has initiated a Geriatric Emergency Department Accreditation Program. Emergency departments (EDs) can be accredited at one of three levels- Gold (Level 1), Silver (Level 2) and Bronze (Level 3). There are various aspects upon which and EDs’ level is determined, including nurse and physician staffing and education, appropriate policies and protocols, quality improvement activities, outcome measures, equipment and the physical environment.
Category: Pediatrics
Posted: 6/29/2018 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
Category: Neurology
Keywords: capacity, dementia, altered mental status, medicolegal, ethics (PubMed Search)
Posted: 6/27/2018 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Medical decision-making capacity refers to the patient’s ability to make informed decisions regarding their care, and emergency physicians are frequently required to assess whether a patient possess this capacity. Patients with acute or chronic neurological diseases (such as dementia) may lack this capacity, and this should be identified, especially in life-threatening situations. The patient must have the ability to:
communicate a consistent choice
understand (and express) the risks, benefits, alternatives and consequences
appreciate how the information applies to the particular situation
reason through the choices to make a decision
There are numerous tools that may help with this assessment, but none has been validated in the ED. Be careful of determining that the patient lacks capacity just because of the diagnosis they carry.
BONUS PEARLS:
Capacity is a fluid concept; a patient may have the capacity to make simple decisions but not more complex ones. Capacity may also change over time
Psychiatry consultation to determine capacity is not obligatory but may be utilized for a second opinion.
Rodgers JJ, Kass JS. Assessment of Medical Decision-making Capacity in Patients With Dementia. Continuum 2018;24(3):920–925.
Category: Critical Care
Posted: 6/26/2018 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Volume Responsiveness, Carotid Ultrasound, and the PLR
Gassner M, Killu K, Bauman Z, Coba V, Rosso K, Blyden D. Feasibility of common carotid artery point of care ultrasound in cardiac output measurements compared to invasive methods. Journal of Ultrasound. 2015;18(2):127-133.
Category: Orthopedics
Posted: 6/23/2018 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
ED visits for acute gout increased almost 27% between 2006 & 2014, a 26.8% increase
Presentation: Acute severe pain, swelling, redness, warmth.
Pain peaks between 12 to 24 hours and onset more likely at night
Quiet, calm period between flares vs other arthritic disorders
Signs of inflammation can extend beyond the joint
Normal to low serum urate values have been noted in 12 to 43% of patients with gout flares
Accurate time for assessment of serum urate is greater than 2 weeks after flare subsides
Most hyperuricemic individuals never experience a clinical event resulting from urate crystal deposition.
Gout flares may occasionally coexist with another type of joint disease (septic joint, psedugout),
A clinical decision rule has shown to be more accurate than clinical diagnosis (17 versus 36%)
*Male sex (2 points)
*Previous patient-reported arthritis flare (2 points)
*Onset within one day (0.5 points)
*Joint redness (1 point)
*First metatarsal phalangeal joint involvement (2.5 points)
*Hypertension or at least one cardiovascular disease (1.5 points)
*Serum urate level greater than 5.88 mg/dL (3.5 points)
Scoring for low (≤4 points), intermediate (>4 to <8 points), and high (≥8 points) probability of gout identified groups with a prevalence of gout of 2.2, 31.2, and 82.5 percent, respectively.
Consider supplementing your clinical decision with this in the future
Miathal A, Singh G. Emergency department visits for gout: a dramatic increase in the past decade. Oral presentation at the EULAR 2018 European Congress of Rheumatology in The Netherlands, June 13–16.
Kienhorst LB, et al. The validation of a diagnostic rule for gout without joint fluid analysis: a prospective study.Rheumatology (Oxford). 2015;54(4):609.
Becker, MA. Clinical manifestations and diagnosis of gout. Up to date. 2018
Category: Pediatrics
Keywords: DKA, cerebral edema, PECARN (PubMed Search)
Posted: 6/22/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Children with diabetic ketoacidosis (DKA) may have brain injuries ranging from mild to severe. The debate over the contribution from intravenous fluids towards poor neurologic outcomes has been ongoing for decades.
PECARN's large multicenter randomized, controlled trial examined the effects of the rate of administration and the sodium chloride content of intravenous fluids on neurologic outcomes in children with diabetic ketoacidosis may finally put the controversy to rest. There was no difference on significant neurologic outcomes based on the rate (fast vs slow) or concentration (0.9% vs 0.45%) of IV fluid administration.
Clinically apparent brain injury occurred in 12 of 1389 episodes (0.9%) of children in DKA.
Any change in the mental or neurological status of the patient should be concerning for life threatening edema and should be treated with mannitol 1g/kg IV bolus or hypertonic saline (3%) 5-10 mL/kg IV over 30 minutes.
Long, B; Koyfman, A. Emergency medicine myths: cerebral edema in pediatric diabetic ketoacidosis and intravenous fluids. J. Emerg. Med; 2017:53(2),212-221.
Category: Critical Care
Keywords: cardiac arrest, CPR, obesity (PubMed Search)
Posted: 6/19/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Although not specifically a part of current recommendations due to lack of data, the AHA has previously recommended shifting upward on the sternum during CPR in the pulseless pregnant patient in order to account for upward displacement of the heart by a gravid uterus. Should the same be done for our obese patients?
Lee et al. performed a retrospective study that reviewed chest CTs to determine the location on the sternum that corresponded to the optimal point of maximal left ventricular diameter (OPLV), in both obese and non-obese patients.
They found that the OPLV was higher (more cranial) on the sternum for obese patients than for patients with normal weight, although 96% of obese patients' OPLV fell within 2cm of where the guidelines recommend standard hand placement should be, compared to a notable 52% in non-obese patients.
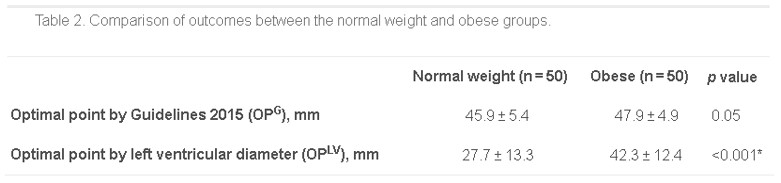
*as measured from the distal end of the sternum
Bottom Line: Radiographically, the location on the sternum that corresponds to optimal compression of the LV is more cranial in obese patients than in non-obese patients. It remains to be seen whether the recommendations for hand placement in CPR should be adjusted, but we may want to consider staying within 4cm of the bottom of the sternum in patients of normal weight.
Lee J, Oh J, Lim TH, et al. Comparison of optimal point on the sternum for chest compression between obese and normal weight individuals with respect to body mass index, using computer tomography: A retrospective study. Resuscitation. 2018; 128:1-5.
Category: Orthopedics
Posted: 6/2/2018 by Michael Bond, MD
(Updated: 6/17/2018)
Click here to contact Michael Bond, MD
Bottom Line:
Less than 1/2 of patients presenting to EDs and being diagnosed with concussion receive mild traumatic brain injury educational materials, and less than 1/2 of patients have seen a clinician for follow up by 3 months after injury.
In order to improve long term outcomes in patients with concusions please remember to provide the patient with approriate discharge instrucitons and strict instructions to follow up on their injury.
Full details of the article in JAMA can be found at https://jamanetwork.com/journals/jamanetworkopen/fullarticle/2681571
Category: Pediatrics
Keywords: Fever, infants, blood culture (PubMed Search)
Posted: 6/15/2018 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
The rate of occult bacteremia in infants 3 months to 24 months with a temperature higher than 40.5C was slightly higher when compared to those with a temperature higher than 39C.
363 infants (3 months to 24 months) with a fever > 40.5C who were well appearing were evaluated in this study. 4 were diagnosed with occult bacteremia (1.1%). 3 of these were caused by S. pneumoniae and 2 were fully immunized.
A larger sample size is needed to see if reconditions to include empiric blood cultures on this subgroup of patients is warrented.
After introduction of the pneumococcal conjugate vaccine, occult bacteremia dramatically decreased. Previous cost effective analysis showed that if the rate of occult bacteremia was less than 0.5%, then empiric testing should be eliminated, but if it is over 1.5%, then obtaining blood work is cost effective. In vaccinated patients, the occult bacteremia rates is less than 0.5%. These studies that showed this included patients with temperatures > 39C. This study looked at higher temperatures to see if there was a higher rate of occult bacteremia in this subgroup. In this ED, in all children with a temperature > 40.5C it was recommended that patients get a blood culture, WBC, ANC, CRP, UA, procalcitonin and PCR for pneumococcus and meningococcus regardless of immunization status. Further testing was at the discretion of the physician.
Gangoiti et al. Prevalence of Occult Bacteremia in Infants with Very High Fever without a source. Pediatr Infect Dis J. 2018 Feb. epub ahead of print.
Category: Toxicology
Keywords: acute agitation, midazolam, antipsychotics, (PubMed Search)
Posted: 6/14/2018 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Acutely agitated patients in the emegency room receive single or combination of benzodiazepine (lorazepam vs. midazolam) and antipsychotic (e.g. haloperidol) agents. Recently, use of ketamine has also been advocated to sedate agitated patients.
A recently published article compared IM administration several medications to treat acutely agitated patients in the ED. According to established protocol, each medication was administered in predetermined 3 week blocks:
Results
N=737 with median age of 40 years, 72% men.
Midazolam resulted in greater proportion of patients with "adequate" sedation (altered mentatl status scale <1) compared to antipsychotics at 15 min post administration. Among antipsychotics, olanzapine resulted in greater proportion of patient with sedation.
Adverse effect were limited
Conclusion:
Midazolam 5 mg IM achieve more effective sedation at 15 min in agitated ED patients than antipsychotics.
Klein LR et al. Intramuscular midazolam, olanzapine, ziprasidone or haloperidol for treating acute agitaion in the emergency department. Ann of Emerg Med 2018 June 6. pii: S0196-0644(18)30373-1. doi: 10.1016/j.annemergmed.2018.04.027. [Epub ahead of print]
Category: Neurology
Keywords: Syncope, neurological, neuroimaging, CT, MRI (PubMed Search)
Posted: 6/13/2018 by WanTsu Wendy Chang, MD
(Updated: 2/7/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider obtaining neuroimaging in patients presenting with syncope only if clinical features suggest probable neurological syncope.
Follow me on Twitter @EM_NCC
Category: Orthopedics
Posted: 6/9/2018 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Syndesmotic sprain aka a “high ankle sprain”
Ankle injuries make up almost 30% of the injuries in professional football
High ankle injuries make up between 16 and 25% of these injuries in the NFL (lateral most common)
10% in general population
In comparison to lateral ankle sprains, high ankle sprains result in significantly more missed games, missed practices and required a longer duration of treatment
Anatomy: The syndesmosis comprises several ligaments and the interosseous membrane
Mechanism: External foot rotation with simultaneous rotation of the tibia and fibula.
Can lead to a Maisonneuve fracture
Injuries 4x more likely in game setting than practice
A positive proximal squeeze test significantly predicts missed games and practices compared to those without.
https://www.youtube.com/watch?v=ThiW_9m7cFM
Conservative management for the stable high ankle injuries in professional football players. Knapik et al. Sports Health 2018
Category: Pediatrics
Keywords: augmentin, conjunctivitis, AOM, otitis media (PubMed Search)
Posted: 6/8/2018 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Although conjuncitivitis outside of the neonatal period is commonly caused by viruses, there are times when antibiotics are warranted due to bacterial infections, such as conjuncitivits-otitis syndrome.
Bottom line: Every patient with conjunctivitis should have an examination of his/her TMs, as your management may change.
Teoh DL, Reynolds S. Diagnosis and management of pediatric conjunctivitis. Pediatric Emergency Care: 2003; 19(1), pp. 48-55.
Bodor FF, Marchant CD, Shurin PA, Barenkamp SJ. Bacterial etiology of conjunctivitis-otitis media syndrome. Pediatrics: 1985; 76(1), pp.26-28.
Bodor FF. Conjunctivitis-Otitis Syndrome. Pediatrics: 1982; 69(6), 695-698.
Category: Geriatrics
Keywords: fever, infection, physiology (PubMed Search)
Posted: 6/3/2018 by Danya Khoujah, MBBS
(Updated: 2/7/2026)
Click here to contact Danya Khoujah, MBBS
Older patients are less likely than their younger counterparts to mount a fever in response to an infection. One explanation is that their basal temperature is lower. Some experts suggest redefining fever in older patients to match this decrease of 0.15C per decade. Therefore, your 80 year old patient would be considered “febrile” if their temperature is above 37.3C, rather than the traditional 38C.
Roghmann MC, Warner J, Mackowiak PA. The relationship between age and fever magnitude. Am J Med Sci. 2001;322(2):68-70
Category: Pharmacology & Therapeutics
Keywords: steroids, infection, leukocytosis (PubMed Search)
Posted: 6/2/2018 by Ashley Martinelli
(Updated: 2/7/2026)
Click here to contact Ashley Martinelli
Steroids induce leukocytosis through the release of cells from bone marrow and the inhibition of neutrophil apoptosis. This effect typically occurs within the first two weeks of steroid treatment.
Leukocyte elevation is commonly used in the diagnosis of septic patients; however, this can be hard to discern in patients on concomitant steroid therapy.
A retrospective cohort study of adult patients presenting with fevers and a diagnosis of pneumonia, urinary tract infection, bacteremia, cellulitis, or COPD exacerbation was conducted to determine the maximal level of WBC within the first 24h of admission between patients on acute, chronic, or no steroid treatment.
Results: maximal WBC levels (p< 0.001)
· Acute steroid therapy: 15.4 ± 8.3 x 10 9/L
· Chronic steroid therapy: 14.9 ± 7.4 x 10 9/L
· No steroid therapy: 12.9 ± 6.4 x 10 9/L
An increase in WBC of 5 x 10 9/L can be found in acute and chronic steroid use when presenting with an acute infection and fever.
Frenkel A, Kachko E, Cohen K, Novak V, Maimon N. Estimations of a degree of steroid inducted leukocytosis in patients with acute infections. Am J Emerg Med. 2018;36(5):749-753.
Category: Orthopedics
Keywords: Heat, exertion, muscle (PubMed Search)
Posted: 5/26/2018 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Exertional rhabdomyolysis (ER)
The warm weather is here and with it comes an increased risk of ER
Risks include the intensity, duration and types of exercises performed
One of the biggest risks is the exercise experience of the participants, both in those with little to no experience and in those experienced athletes less trained than their counterparts.
Multiple case reports find that intense novel exercises early in the preseason before getting acclimatized and “in shape” carry great risk to the participant. These can be summarized as “too much, too soon, too fast.”
Coaches need to be educated about this and be prepared to detect and effectively handle ER through an emergency action plan.
-Conditioning workouts need to be phased in rather than start at maximum intensity on day one.
Eccentric exercises appear worse than concentric exercises.
Has been seen in almost all sports, ranging from swimming to golf.
It’s not just preseason football!
High humidity and high temperature environments increase the likelihood of ER
Males are more vulnerable to ER than females
Increased risk with sickle cell trait and glycogen storage diseases
Multiple drugs may increase individual risk including alcohol, cocaine, amphetamines, MDMA and caffeine.
Implicated medicines include, salicylates, neuroleptics, quinine, corticosteroids, statins, theophylline, cyclic antidepressants and SSRIs
Football Team Rhabdomyolysis: The Pain Beats the Gain and the Coach Is to Blame Eichner, E., Randy, Current Sports Medicine Reports: May 2018
Category: Neurology
Keywords: myelopathy, myelitis, physical exam (PubMed Search)
Posted: 5/23/2018 by Danya Khoujah, MBBS
(Updated: 2/7/2026)
Click here to contact Danya Khoujah, MBBS
Lhermitte’s phenomenon is as a sign of cervical spinal cord demyelination. It is considered positive if flexion of the neck causes a tingling sensation moving down the limbs or trunk, and may be reported as a symptom or elicited as a sign. This is due to stretching of the dorsal column sensory fibers, the commonest cause of which is multiple sclerosis. Other causes include other myelopathies, such as B12 deficiency, radiation and toxic (due to chemotherapy) or idiopathic myelitis. Its sensitivity is low at 16%, but its specificity for myelopathy is high at 97%.
Kempster PA, Rollinson RD. The Lhermitte phenomenon: variant forms and their significance. J Clin Neurosci 2008;15(4):379–81.
Khare S, Seth D. Lhermitte's Sign: The current status. Ann Indian Acad Neurol. 2015 Apr-Jun; 18(2): 154-156.
Category: Critical Care
Keywords: sepsis, septic shock, guidelines (PubMed Search)
Posted: 5/22/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD


Take Home Points:
For additional reading:
EMNerd, Dr. Rory Spiegel https://emcrit.org/emnerd/em-nerd-case-temporal-fallacy/
Surviving Sepsis Campaign http://www.survivingsepsis.org/Guidelines/Pages/default.aspx
Category: Pediatrics
Keywords: Button batteries, removal (PubMed Search)
Posted: 5/18/2018 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
There were 180 battery ingestions over a 5 year period at two tertiary care children’s hospital. The median age was 3.8 years (0.7 to 18 years). The most common symptoms were abdominal pain (17%), and nausea and vomiting (14%). X-rays detected the location in 94% of patients.
Based on these patients, a treatment algorithm was developed (See attached). Prospective validation is needed.
All patients with esophageal batteries had an intervention (foley catheter removal with post procedure esophagram, ridged esophagram or EGD).
The majority of patients with a gastric battery or small bowel battery were managed non operatively.
20 patients had a colonic battery and 7 had symptoms of abdominal pain or nausea or vomiting.
For batteries distal to the gastroesophageal junction, 16 patients had an intervention. 13 had an EGD with a 69% retrieval rate. 1 patient had a colonoscopy with successful retrieval. 2 patients had abdominal surgery with retrieval.
Rosenfled et al. Battery ingestions in children: Variations in care and development of a clinical algorithm. Journal of Pediatric Surgery. 2018. Epub ahead of print.
Category: Toxicology
Keywords: Methylene Blue (PubMed Search)
Posted: 5/17/2018 by Kathy Prybys, MD
(Updated: 5/18/2018)
Click here to contact Kathy Prybys, MD
Methylene Blue is a dye that was synthesized in the late 1800s as an antimalarial drug. After the emergence of chloroquine its use loss favor partly due to unpopular side effects of temporarily turning the urine, other body fluids, and the sclera blue. Methylene blue is primarily known as a highly effective fast acting antidote for methemboglobinemia. Over the past few years, it has become an important therapeutic modality with expanding uses in cardiac surgery and critical care. As a potent inhibitor of nitric oxide mediated guanylate cyclase induced endothelium vascular smooth muscle relaxation, it has been shown to be effective in increasing arterial blood pressure and cardiac function in several clinical states, such as septic shock and calcium channel blocker poisoning.
BOTTOM LINE:
Methylene blue should be considered for treatment of refractory shock from calcium channel and beta blocker poisoning.
Clinical improvement in refractory hypotension and reduction of vasopressor dose has been described in several poisoning cases.
Recommended dose is 1–2 mg/kg injection with effects seen within 1 hour.
Methylene Blue Used in the Treatment of Refractory Shock Resulting From Drug Poisoning. Fisher J, et al. Clin Toxicol 2914 Jan;52:63-65.
Calicum channel antagonist and beta blocker overdose: antidotes and adjunct therapies. Graudins A, et al. British Journal of Clin Pharm. 2016;81(3):453-461.
