Category: Critical Care
Posted: 1/22/2019 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Respiratory Complications of ICIs
Ferreyro BL, Munshi L. Causes of acure respiratory failure in the immunocompromised host. Curr Opin Crit Care. 2019;25:21-8.
Category: Orthopedics
Keywords: anesthetic, orthopedics, wound (PubMed Search)
Posted: 1/19/2019 by Michael Bond, MD
Click here to contact Michael Bond, MD
When caring for a patient with a laceration we often do lcoal infiltration prior to suturing but remember the benefits of regional nerve blocks
Benefits of Regional Nerve Blocks
Quick reminder of properities of common anesthetic
| Anesthetic | Onset of Action | Duration of Action | Max Dose No Epi | Max Dose With Epi |
|---|---|---|---|---|
| Lidocaine | Seconds | 1 hr | 4mg/kg | 7mg/kg |
| Bupivicaine | Seconds + | > 6 hrs | 2mg/kg | 3mg/kg |
Final reminder: There is no evidence that epinephrine causes necrosis and it can be used safely in digital blocks. Duration of action is max 90 minutes. Even individuals that have injected themselves with EpiPens into their hands have not had any long term sequelue or necrosis seen. Vast majority required no treatment at all.
Category: Pediatrics
Keywords: Post-tonsillectomy, bleeding, airway (PubMed Search)
Posted: 1/18/2019 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Post tonsillectomy hemorrhage occurs and 0.1-3% of post tonsillectomy patient's. It occurs typically greater than 24 hours after surgery and up to 4-10 days postoperatively. A survey of otolaryngologists showed that ED management strategies for active bleeding have included direct pressure, clot suction, silver nitrate, topical epinephrine, and thrombin powder.
This article was a case study demonstrating the use of nebulized tranexamic acid (TXA) for post tonsillectomy hemorrhage in a 3-year-old patient. The patient had a copious amount of oral bleeding and had failed treatment with nebulized racemic epinephrine and direct pressure was not an option due to the patient's cooperation and small mouth. 250 mg of IV TXA was given via nebulizer with a flow rate of 8 L. Bleeding stopped 5-7 minutes after completion of the nebulizer. The patient was then taken to the OR for definitive management. No adverse effects were noticed.
TXA in the pediatric population has been shown to decrease surgical blood loss and transfusions in cardiac, spine and craniofacial surgeries. Studies have also been done in pediatric patients with diffuse alveolar hemorrhage using doses of 250 mg for children less than 25 kg and 500 mg for those who are greater than 25 kg.
Bottom line: There are case reports of nebulized TXA use in the pediatric population with no adverse outcomes noted. More research is needed.
Schwarz W, Ruttan T, Bundick K. Nebulized Tranexamic Acid Use for Pediatric Secondary Post-Tonsillectomy Hemorrhage. Annals of Emergency Medicine 2018. Epub ahead of print.
Category: Critical Care
Keywords: Cardiac arrest, neruo (PubMed Search)
Posted: 1/15/2019 by Daniel Haase, MD
(Updated: 1/19/2019)
Click here to contact Daniel Haase, MD
--Late awakening (>48h after sedation held) was common (78/402) in patients with cardiac arrest in prospective cohort study
--Poor prognostic signs of discontinuous (10-49% suppression) EEG and absent brain stem reflexes were independently associated with late awakening. Use of midazolam also associated with late awakening
--Late awakeners had good functional outcome when compared to early awakeners
DON'T NEUROPROGNOSTIC EARLY (OR IN ED)!
And traditional poor prognostic signs may not be as poor as previously thought!
------------------
Rey A, Rossetti AO, Miroz JP, et al. Late Awakening in Survivors of Postanoxic Coma: Early Neurophysiologic Predictors and Association With ICU and Long-Term Neurologic Recovery. Critical Care Medicine: January 2019 - Volume 47 - Issue 1 - p 85–92
Category: Orthopedics
Keywords: Skiing, gamekeeper (PubMed Search)
Posted: 1/12/2019 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Epidemiology of Alpine Skiing Injuries
Mean age of injury 30.3 (range 24 to 35.4 years)
Populations at greatest risk are children and adolescents and possibly adults over 50 (increased risk of tibial plateau fractures)
Sex: Males> females
Knee injuries, esp to ACL, are higher among females
Fractures greater in males
Injury location greatest at lower extremity (primarily to knee)
Primarily sprains to MCL and ACL (increasing incidence)
14% occur to upper extremity and primarily involve the thumb and shoulder
Skiers thumb – FOOSH with thumb Abducted gripping pole
Pole is implicated as this injury is rare among snowboarders
The pole acts as a lever to amplify the forced Abduction of the thumb as the outstretched hand hits the ground.
Let go before you hit the ground!!
13% occur to head and neck
The number of all type injuries has decreased over time with advances in equipment and helmet use
Proportion of skiers wearing a helmet exceeds 80%
However, the number of traumatic fatalities has remained constant
Accidents involving fatalities exceed the protective capacity of helmets
Helmets likely decrease risk of mild and moderate head injury
Ekeland et al., 2018. Epidemiology of Alpine Skiing Injuries. J Sci Med Sport
Davey et al., 2018. Alpine Skiing Injuries. Sports Health
Category: Pediatrics
Keywords: ADEM (PubMed Search)
Posted: 1/11/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Acute Disseminated Encephalomyelitis (ADEM) is primarily a pediatric disease and can cause a wide variety of neurologic symptoms. As such, should always be in the differential for pediatric patient presenting with vague neurologic symptoms including altered mental status. It is an immune-mediated, demyelinating disease that can affect any part of the CNS; usually preceding a viral illness or rarely, immunizations.
The average age of onset is 5-8 years of age with no gender predilection. It usually has a prodromal. That includes headache, fever, malaise, back pain etc. Neurological symptoms can vary and may present with ataxia, altered mental status, seizures, focal symptoms, behavioral changes or coma.
MRI is the primary modality to diagnose this condition. Other possible indicators may be mild pleocytosis with lymphocyte predominance, and elevated inflammatory markers such as ESR, CRP. These findings, however, are neither sensitive nor specific.
First-line treatment for ADEM is systemic corticosteroids, typically 20-30 mg/kg of methylprednisolone for 2-5 days, followed by oral prednisone 1-2 mg/kg for 1-2 weeks then 3-6-week taper. For steroid refractory cases, IVIG and plasmapheresis may be considered.
ADEM usually has a favorable long-term prognosis in the majority of patients. However, some may experience residual neurological deficits including ataxia, blindness, clumsiness, etc.
Take home points:
Gray, M.P. & Goralick, M.H. (2016). Acute disseminated encephalomyelitis (6th ed, volume 32). Milkwaukee, WI
Category: Toxicology
Keywords: take home naloxone, opioid overdose (PubMed Search)
Posted: 1/10/2019 by Hong Kim, MD
Click here to contact Hong Kim, MD
Take home naloxone (THN) programs have been expanded to help reduce the opioid overdose-related deaths. A study was done in Australia to characterize a cohort of heroin overdose deaths to examine if there was an opportunity for a bystander to intervene at the time of fatal overdose.
235 heroin-overdose deaths were investigated during a 2 year study period in Victoria, Australia.
Conclusion
Stam NC et al. Challenges with take-home naloxone in reducing heroin mortality: a review of fatal heroin overdose cases in Victoria, Australia. Clin Toxicol 2018 Nov 17:1-6. doi: 10.1080/15563650.2018.1529319. [Epub ahead of print]
Category: Neurology
Keywords: Intracerebral hemorrhage, ICH, volume, ABC/2 (PubMed Search)
Posted: 1/9/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
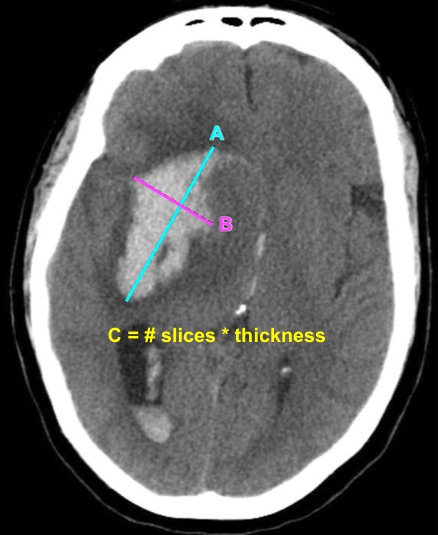
Bottom Line: EPs can reliably estimate ICH volume using the ABC/2 formula. Communicating ICH volume to neurosurgical and neurocritical care consultants can help direct treatment decisions.
Dsouza LB, Pathan SA, Bhutta ZA, et al. ABC/2 estimation in intracerebral hemorrhage: A comparison study between emergency radiologists and emergency physicians. Am J Emerg Med. 2018 Dec 19. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 1/8/2019 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Critically Ill Renal Transplant Patients
Darmon M, et al. Ten tips to manage renal transplant recipients. Intensive Care Med. 2019. epub ahead of print.
Category: Pharmacology & Therapeutics
Keywords: Flu, Treatment, Oseltamivir (PubMed Search)
Posted: 1/8/2019 by Wesley Oliver
(Updated: 2/8/2026)
Click here to contact Wesley Oliver
---Early antiviral treatment can shorten the duration of fever and illness symptoms, and may reduce the risk of some complications from influenza.
---Early treatment of hospitalized adult influenza patients with oseltamivir has been reported to reduce death in some observational studies.
---Clinical benefit is greatest when antiviral treatment is administered within 48 hours of influenza illness onset.
Antiviral treatment is recommended for patients with confirmed or suspected influenza who:
---are hospitalized;
---have severe, complicated, or progressive illness; or
---are at higher risk for influenza complications. (See below for in-depth information)
Oral oseltamivir is the recommended antiviral for patients with severe, complicated, or progressive illness who are not hospitalized, and for hospitalized influenza patients.
Treatment:
Doses: Oseltamivir 75 mg twice daily
Renal Impairment Dosing
CrCl >60 mL/minute: No dosage adjustment necessary
CrCl >30 to 60 mL/minute: 30 mg twice daily
CrCl >10 to 30 mL/minute: 30 mg once daily
ESRD undergoing dialysis: 30 mg immediately and then 30 mg after every hemodialysis session
Duration of Treatment:
Recommended duration for antiviral treatment is 5 days for oral oseltamivir. Longer daily dosing can be considered for patients who remain severely ill after 5 days of treatment.
People at higher risk for influenza complications recommended for antiviral treatment include:
---children younger than 2 years;
---adults 65 years and older;
---people with chronic pulmonary (including asthma), cardiovascular (except hypertension alone), renal, hepatic, hematological (including sickle cell disease), and metabolic disorders (including diabetes mellitus), or neurologic and neurodevelopment conditions (including disorders of the brain, spinal cord, peripheral nerve, and muscle, such as cerebral palsy, epilepsy [seizure disorders], stroke, intellectual disability, moderate to severe developmental delay, muscular dystrophy, or spinal cord injury);
---people with immunosuppression, including that caused by medications or by HIV infection;
---women who are pregnant or postpartum (within 2 weeks after delivery);
---people younger than 19 years old who are receiving long-term aspirin- or salicylate-containing medications
---American Indians/Alaska Natives;
---people who are extremely obese (i.e., body mass index is equal to or greater than 40); and
---residents of nursing homes and other chronic care facilities.
Centers for Disease Control and Prevention. Influenza antiviral medications: summary for clinicians. https://www.cdc.gov/flu/professionals/antivirals/summary-clinicians.htm (Accessed on January 8, 2019).
Category: Critical Care
Posted: 1/1/2019 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Dyspnea in the Intubated Patient
Decavele M, et al. Detection and management of dyspnea in mechanically ventilated patients. Curr Opin Crit Care. 2019; 25:86-94.
Category: Critical Care
Keywords: circulatory dysfunction, hypotension, shock, fluid resuscitation, IV fluids (PubMed Search)
Posted: 1/1/2019 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
The European Society of Intensive Care Medicine (ESICM) recently released a review with recommendations from an expert panel for the use of IV fluids in the resuscitation of patients with acute circulatory dysfunction, especially in settings where invasive monitoring methods and ultrasound may not be available.
Points made by the panel include:
Recommendations from the panel include:
Bottom Line: Utilize all the information you have about your patient to determine whether or not they require IVF, and reevaluate their physical and biochemical (lactate) response to fluids to ensure appropriate IVF administration and avoid volume overload.
Cecconi M, Hernandez G, Dunser M, et al. Intensive Care Med. 2018. https://doi-org.proxy-hs.researchport.umd.edu/10.1007/s00134-018-5415-2
Category: Toxicology
Keywords: double-dose of single medication (PubMed Search)
Posted: 12/27/2018 by Hong Kim, MD
(Updated: 2/8/2026)
Click here to contact Hong Kim, MD
Taking a double-dose of a single medication is presumed to be safe in most cases. However, there is limited data to support this assumption.
A retrospective study of the California Poison Control System was performed to assess adverse effects of taking double dose of a single medication. During a 10-year period, 876 cases of double-dose ingestion of single medication were identified.
Adverse effects were rare (12 cases). However, medication classes that were involved in severe adverse effects included:
Conclusion:
Correia MS et al. A 10-year review of single medication double-dose ingestions in the nation's largest poison control system. Clin Toxicol 2018 Nov 28:1-5. doi: 10.1080/15563650.2018.1493205. [Epub ahead of print]
Category: Neurology
Keywords: headache, post concussion syndrome (PubMed Search)
Posted: 12/16/2018 by Brian Corwell, MD
(Updated: 12/23/2018)
Click here to contact Brian Corwell, MD
A previous pearl discussed medication-overuse headache (MOH).
MOH is also known as analgesic rebound headache, drug-induced headache or medication-misuse headache.
It is defined as headache… occurring on 15** or more days per month in a patient with a preexisting headache disorder who has been overusing one or more acute treatment drugs for headache with symptoms for three or more months.
The diagnosis is clinical, and requires a hx of chronic daily headache with analgesic use more than 2-3d per week.
The diagnosis of MOH is supported if headache frequency increases in response to increasing medication use, and/or improves when the overused medication is withdrawn.
The headache may improve transiently with analgesics and returns as the medication wears off. The clinical improvement after wash out is not rapid however, patients may undergo a period where their headaches will get worse. This period could last in the order of a few months in some cases.
The meds can be dc’d cold turkey or tapered depending on clinical scenario.
Greatest in middle aged persons. The prevalence rages from 1% to 2% with a 3:1 female to male ratio.
Migraine is the most common associated primary headache disorder.
** Each medication class has a specific threshold.
Triptans, ergot alkaloids, combination analgesics, or opioids on ten or more days per month constitute medication overuse.
Use of simple analgesics, including aspirin, acetaminophen and NSAIDS on 15 or more days per month constitutes medication overuse.
Caffeine intake of more than 200mg per day increases the risk of MOH.
Consider MOH in patients in the appropriate clinical scenario as sometimes doing less is more!
Category: Pediatrics
Keywords: Intubation, ETT, cuffed, airway management (PubMed Search)
Posted: 12/21/2018 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Historically uncuffed endotracheal tubes were used in children under the age of 8 years due to concerns for tracheal stenosis. Advances in medicine and monitoring capabilities have resulted in this thinking becoming obsolete. Research is being conducted that is showing the noninferiority of cuffed tubes compared to uncuffed tubes. Multiple other studies are looking into the advantages of cuffed tubes compared to uncuffed tubes.
The referenced study is a meta-analysis of 6 studies which compared cuffed to uncuffed endotracheal tubes in pediatrics. The pooled analysis showed that more patients needed tube changes when they initially had uncuffed tubes placed. There was no difference in intubation duration, reintubation occurrence, post extubation stridor, or racemic epinephrine use between cuffed and uncuffed tubes.
Bottom line: There is no difference in the complication rate between cuffed and uncuffed endotracheal tubes, but uncuffed endotracheal tubes did need to be changed more frequently.
Liang C, Zhang J, Pan G, Li X, Shi T, He W. Cuffed versus uncuffed endotracheal tubes in pediatrics: a meta-analysis. Open Med. 2018; 13:366-373.
Category: Toxicology
Keywords: Bupropion, TCAs, adolescents (PubMed Search)
Posted: 12/20/2018 by Hong Kim, MD
Click here to contact Hong Kim, MD
Selective serotonin reuptake inhibitors are the most common anti-depressant used today. However, the use bupropion in adolescents is increasing due the belief that it has fewer side effects than TCAs.
Using the National Poison Data System (2013 – 2016), the adverse effects of bupropion were compared to TCA in adolescents (13 – 19 years old) with a history of overdose (self harm).
Common clinical effects were:
TCA: n=1496; Bupropion: n=2257
| Clinical effects | TCAs | Bupropion |
| Tachycardia | 59.9% | 70.7% |
| Drowsiness/lethargy | 51.5% | 18.1% |
| Conduction disturbance | 22.2% | 15.6% |
| Agitation | 19.1% | 16.4% |
| Hallucination/delusions | 4.2% | 23.9% |
| Seizure | 3.9% | 30.7% |
| Vomiting | 2.7% | 20.0% |
| Tremor | 3.7% | 18.1% |
| Hypotension | 2.7% | 8.0% |
| Death | 0.3% | 0.3% |
Conclusion:
Bupropion overdose results in significant adverse effects in overdose; however, death is relatively rare.
Sheridan DC et al. Suicidal bupropion ingestions in adolescents: increased morbidity compared to other antidepressants. Clin Toxicol. 2018;56:360-364.
Category: Neurology
Keywords: ultrasound, lumbar puncture, LP, landmark (PubMed Search)
Posted: 12/12/2018 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider using pre-procedural ultrasound-assistance for all lumbar punctures.
Gottlieb M, Holladay D, Peksa GD. Ultrasound-assisted lumbar punctures: a systematic review and meta-analysis. Acad Emerg Med. 2018 Aug 21. [Epub ahead of print]
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 12/11/2018 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Noninvasive Ventilation in De-Novo Respiratory Failure
Thille AW, Frat JP. Noninvasive ventilation as acute therapy. Curr Opin Crit Care. 2018; 24:519-24.
Category: Orthopedics
Keywords: head injury, medication (PubMed Search)
Posted: 12/8/2018 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Retrospective chart review at a headache clinic seeing adolescent concussion patients
70.1% met criteria for probable medication-overuse headache
Once culprit over the counter medications (NSAIDs, acetaminophen) were discontinued,
68.5% of patients reported return to their preinjury headache status
Take home: Excessive use of OTC analgesics post concussion may contribute to chronic post-traumatic headaches
If you suspect medication overuse, consider analgesic detoxification
Heyer and Idris., 2014. Pediatr Neurol. Does analgesic overuse contribute to chronic post-traumatic headaches in adolescent concussion patients?
Category: Critical Care
Keywords: hyperoxia, oxygen therapy, saturation, SpO2, critical care, mechanical ventilation (PubMed Search)
Posted: 12/4/2018 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Hyperoxia has been repeatedly demonstrated to be detrimental in a variety of patients, including those with myocardial infarction, cardiac arrest, stroke, traumatic brain injury, and requiring mechanical ventilation,1-4 and the data that hyperoxia is harmful continues to mount:
Bottom Line: Avoid hyperoxia in your ED patients, both relatively stable and critically ill. Remove or turn down supplemental O2 added by well-meaning pre-hospital providers and nurses, and wean down ventilator settings (often FiO2). A target SpO2 of >92% (>88% in COPD patients) or PaO2 >55-60 is reasonable in the majority of patients.8
