Category: Critical Care
Posted: 10/17/2017 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Improving CPR Performance
Nassar BS, et al. Improving CPR performance. Chest. 2017. {epub ahead of print]
Jentzer JC, et al. Improving survival from cardiac arrest: A review of contemporary practice and challenges. Ann Emerg Med. 2016; 68:678-89.
Category: Orthopedics
Keywords: Knee pain (PubMed Search)
Posted: 10/14/2017 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Complete or incomplete separation of the articular cartilage and subchondral bone
-70% occur at the lateral aspect of the medial femoral condyle
-Also seen in the talar dome and capitellum
Repetitive overloading leads to fragmentation and separation from surrounding bone
Prognosis better in kids than in adults
http://www.eorif.com/KneeLeg/Images/OCD4w.jpg
CC: Vague difficult to localize activity related pain and swelling. Mechanical symptoms only if loose body is present
PE: Wilson’s test
Internal tibial rotation and knee extension impinges the tibia on the OCD lesion causing pain. Pain abates with external rotation and flexion.
https://www.youtube.com/watch?v=e7zrKo41Pos
Plan of care: Limit activity and trial period of non-weight bearing for 6 weeks.
50% resolve in 10 to 18 months with conservative care.
Detached, loose or unstable fragments or failure of non-operative care will need surgery
Category: Pediatrics
Keywords: Trauma, hematuria, kidney injury (PubMed Search)
Posted: 10/13/2017 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: Cannabinoid, cyclic vomiting, Capsaicin (PubMed Search)
Posted: 10/12/2017 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Cannabinoid hyperemesis is a syndrome (CHS) characterized by severe intractable nausea, cyclical vomiting, and abdominal pain associated with chronic marijuana abuse. It is often a underrecognized cause of cyclic vomiting syndrome. Despite well established anti-emetic properties of marijuana, paradoxical effects on the GI tract exist through cannabinoid receptors which exert their neuromodulatory properties in the central nervous system and the enteric plexus. Multiple theories of mechanism of CHS are in the literature. Diagnosis is based on the following clinical criteria:
Acute care goals are to treat dehydration and terminate nausea and vomiting. Administration of intravenous fluids, dopamine antagonists, topical capsaicin cream, and avoidance of narcotic medications are recommened treatment measures. Benzodiazepines followed by haloperidol and topical capsaicin are reported to be most effective. Capsaicin activates the transient receptor potential vanilloid 1 receptors (TRPV1) which impairs substance P signalling in the area postrema and nucleus tract solitarius similar to noxious stimuli, such as heat.
Cannabinoid Hyperemesis Syndrome: Diagnosis, Pathophysiology, and Treatment-a Systematic Review. Sorensen CJ, DeSanto K, et al. J Med Toxicol. 2017 Mar;13(1):71-87.
Cannabinoid Hyperemesis and Compulsive Bathing: A Case Series and Paradoxical Pathophysiological Explanation. Patterson D, Smith E, et al. Am Board Fam Med. 2010 Nov-Dec; 23(6): 790-793.
Pharmacologic treatment of cannabinoid hyperemesis Syndrome: A systematic review. Pharmacotherapy. Dezieck L, Hafez Z. 2017 Jun:37(6):725-734.
Resolution of cannabis hyperemesis syndrome with topical capsaicin in the emergency department: a case series. Dezieck L, Hafez Z, et al. Clin Toxicol (Phila). 2017 Sep;55(8):908-913.
Category: Neurology
Keywords: traumatic brain injury, TBI, fall, subdural hematoma, SDH, elderly (PubMed Search)
Posted: 10/11/2017 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Traumatic brain injury (TBI) is associated with close to half of major trauma admissions in adults over age 65 in the U.K.
Falls accounted for 85% of all TBIs, while 45% of patients had subdural hematomas (SDH).
More than 3/4 of patients were treated conservatively, though outcomes were not significantly better than those who underwent neurosurgical intervention.
Higher age is associated with higher mortality and greater disability.
Bottom Line: Trauma in older adults is increasing and fall prevention is important in reducing significant injuries.
Hawley C, Sakr M, Scapinello S, et al. Traumatic brain injuries in older adults - 6 years of data for one UK trauma centre: retrospective analysis of prospectively collected data. Emerg Med J 2017;0:1-8.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: liver failure, dialysis, MARS, Molecular Adsorbent Recirculating System (PubMed Search)
Posted: 10/10/2017 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Molecular Adsorbent Recirculating System (MARS) is an artificial liver support system colloquially known in the medical field as "dialysis for the liver."
Take-Home:
1. Consider MARS in your patient with severe acute liver failure due to potentially reversible/recoverable etiology
2. Know if and where MARS is offered near you

(http://findbesttreatment.com/images/healthnet_dialyse_schema.gif)
Molecular Adsorbent Recirculating System (MARS) is an artificial liver support system colloquially known in the medical field as "dialysis for the liver."
Its use demonstrates apparent effective replacement of liver function, with consistently-proven improvements in hemodynamics, hepatic encephalopathy, hepatorenal syndrome, drug clearance, hyperbilirubinemia, and other markers of hepatic homeostasis.
It has been repeatedly demonstrated to work well as a short-term bridge to liver recovery or liver transplant in severe ALF of various causes, especially those that are generally reversible with support and time severe trauma, toxic ingestions, and acute alcoholic hepatitis.
Mortality benefit remains unclear and may be dependent on the subtype of acute liver failure. Most of the current literature is made up of case reports, or case studies with small study populations. In acute on chronic liver failure, the 23-patient randomized, controlled RELIEF trial failed to show survival advantage at 28 days. Gerth et al, however, found a 14-day mortality benefit in ACF patients by retrospective analysis, which may indicate that MARS use as a bridge to transplant is the most appropriate utilization in this patient population.
Category: Pharmacology & Therapeutics
Keywords: antipyretic, sepsis, fever (PubMed Search)
Posted: 10/7/2017 by Ashley Martinelli
(Updated: 2/8/2026)
Click here to contact Ashley Martinelli
Fever occurs in 40% of patients with sepsis. Historically, there has been conflicting evidence of whether patient outcomes improve with antipyretic therapy.
A recent large meta-analysis assessed the effect of antipyretic therapy on mortality of critically ill septic patients. The analysis included 8 randomized studies (1,531 patients) and 8 observational studies (17,432 patients) that assessed mortality of septic patients with and without antipyretic therapy.
The authors found no difference in mortality at 28 days or during hospital admission. There was also no difference in shock reversal, heart rate, or minute ventilation.
As expected, they found a statistically significant reduction in posttreatment body temperature (-0.38°C, 95% IC -0.63 to -0.13) in patients who received antipyretic therapy. NSAIDs and cooling therapies were more effective than acetaminophen, however no agent or dosing information was provided and only one study included physical cooling therapies.
Bottom Line: Antipyretic therapies do not reduce mortality in patients with sepsis, but they may improve patient comfort by reducing body temperature.
Drewry AM, et al. Antipyretic therapy in critically ill septic patients: a systematic review and meta-analysis. Crit Care Med 2017;45:806-813.
Category: Pediatrics
Keywords: Pediatrics, Bronchiolitis, Respiratory Decompensation, Risk factors (PubMed Search)
Posted: 10/6/2017 by Megan Cobb, MD
Click here to contact Megan Cobb, MD
Bronchiolitis season will soon be upon us. Here are some risk factors for children under 2 y/o with bronchiolitis, who may be more likely to suffer respiratory decompensation:
1. Age under 9 months
2. Black race
3. Hypoxia documented in the ED
4. Persisent accessory muscle use.
Bottom Line: Consider providing respiratory support sooner than later in bronchiolitic infants with risk factors for decompensation. For HFNC, start at 1.5 - 2.0 L/kg/min, and titrate to work of breathing and 02 saturations.
_______________________________________________________________________________
Pathophysiology: Bronchiolitis is a disease process that leads to inflammation of lower airways, causing bronchiolar edema, epithelial hyperplasia, mucus plugging, and air trapping or atelectasis. Common viral causes include RSV, Human Metapneumovirus, Rhinovirus, Influenza, and Parainfluenza.
Clinical Course: For most strains, the disease course is often 5-7 days with the worst days being 3-5. The disease process can last longer, especially in neonates. The predominant presenting symptoms are often rhinorrhea, low grade fevers, and cough, but apnea can be the primary symptom in younger infants. As a result of increased work of breathing, PO feeding tolerance decreases and leads to dehydration.
Treatment: Primarily supportive care with suctioning, hydration, supplemental oxygen via standard NC, HFNC, and in severe cases BiPAP, CPAP or intubation. Trial of bronchodilator is often used, but there is no role for repeated bronchodilator use if no benefit is seen in pre and posttreatment respiratory effort. Hypertonic saline is not recommended for routine use in the ED. Corticosteroids have no role for routine use in viral bronchiolitis, either.
Category: Toxicology
Keywords: Capsaicin, hunan hand, chili peppers (PubMed Search)
Posted: 10/6/2017 by Kathy Prybys, MD
Click here to contact Kathy Prybys, MD
Hunan hand syndrome is a painful contact dermatitis that frequently presents in cooks and chili pepper workers after preparing or handling chili peppers. Contact with other body parts gives rise to the terms: "Hunan nose" ''Hunan eye",and "Chili Willie". Capsaicin, found in the fruit of plants from the genus Capsicum such as red chili peppers, jalapeños, and habaneros, is a hydrophobic, colorless, odorless compound that binds with pain receptors causing the sensation of intense heat or burning. The "heat" or pungency of a peppers is measured in Scoville heat units (SHU), the number of times a chili extract must be diluted with water to lose heat. Habanero peppers generate 30,000 SHU. Even at low concentrations capsaicin is a skin irritant. It is the primary ingredient in pepper spray used in law enforcement and in personal defense sprays.
Treatment consists of decontamination with water irrigation for opthalmic exposure and milk or antacids for dermal or gastrointestinal exposure. Burning can be recurrent and of of long duration depending on tissue penetration. Topical anesthetic especially for the eye and cool compresses for the skin can relieve pain. Parodoxically capsaicin is used as a topical analgesic medication for local pain relief from muscle pain, itching, and painful neuropathies (diabetic, postherpetic). Capsaicin initially causes neuronal excitation followed by a long-lasting refractory period due to depletion of substance P, during which neurons are no longer responsive to a large range of stimuli and thus are desensitized.
Category: Critical Care
Posted: 10/4/2017 by Ashley Menne, MD
(Updated: 2/8/2026)
Click here to contact Ashley Menne, MD
Risk of Pneumocystis pneumonia (PCP) increases with degree of immunosuppression. If clinical suspicion exists (CD4 <200 with cough, pulmonary infiltrates, hypoxic respiratory failure), it is reasonable to initiate empiric therapy.
First line treatment is trimethoprim-sulfamethoxazole (TMP-SMX) orally or IV for 21 days. IV pentamidine has equivalent efficacy to IV TMP-SMX but greater toxicity and is generally reserved for patients with severe PCP who cannot tolerate or are unresponsive to TMP-SMX.
Importantly, adjunctive corticosteroids have been shown to significantly improve outcomes (mortality, need for ICU admission, need for mechanical ventilation) in HIV-infected patients with moderate to severe PCP (defined by pO2 <70 mmHg on Room Air).
· Ideally steroids should be started BEFORE (or at the same time as) Pneumocystis-specific treatment to prevent/mitigate the sharp deterioration in lung function that occurs in most patients after initiation of PCP treatment. This is thought to be secondary to the intense inflammatory response to lysis of Pneumocystis organisms, which can cause an ARDS-like picture.
· Recommended dosing schedule: 40mg prednisone twice daily for 5 days, then 40mg once daily for 5 days, followed by 20mg once daily for the remaining 11 days of treatment.
Bottom Line: In patients with moderate to severe PCP (pO2 <70 mmHg on RA), don’t forget to initiate adjunctive corticosteroids early (at the same time you initiate empiric therapy for PCP).
Wang RJ, Miller RF, Huang L. Approach to Fungal Infections in Human Immunodeficiency Virus–Infected Individuals. Clin Chest Med. 2017;38(3):465-477. doi:10.1016/j.ccm.2017.04.008.
Bozzette SA, Sattler FR, Chiu J, et al. A Controlled Trial of Early Adjunctive Treatment with Corticosteroids for Pneumocystis carinii Pneumonia in the Acquired Immunodeficiency Syndrome. N Engl J Med. 1990;323(21):1451-1457. doi:10.1056/NEJM199011223232104.
Montaner JS, Lawson LM, Levitt N, Belzberg A, Schechter MT, Ruedy J. Corticosteroids prevent early deterioration in patients with moderately severe Pneumocystis carinii pneumonia and the acquired immunodeficiency syndrome (AIDS). Ann Intern Med. 1990;113(1):14-20. http://www.ncbi.nlm.nih.gov/pubmed/2190515.
Category: International EM
Keywords: Influenza, southern hemisphere (PubMed Search)
Posted: 10/4/2017 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
The current number of influenza cases in the Southern Hemisphere is substantially higher than normal. For example, in Australia the number of influenza cases this year are twice the next highest year. 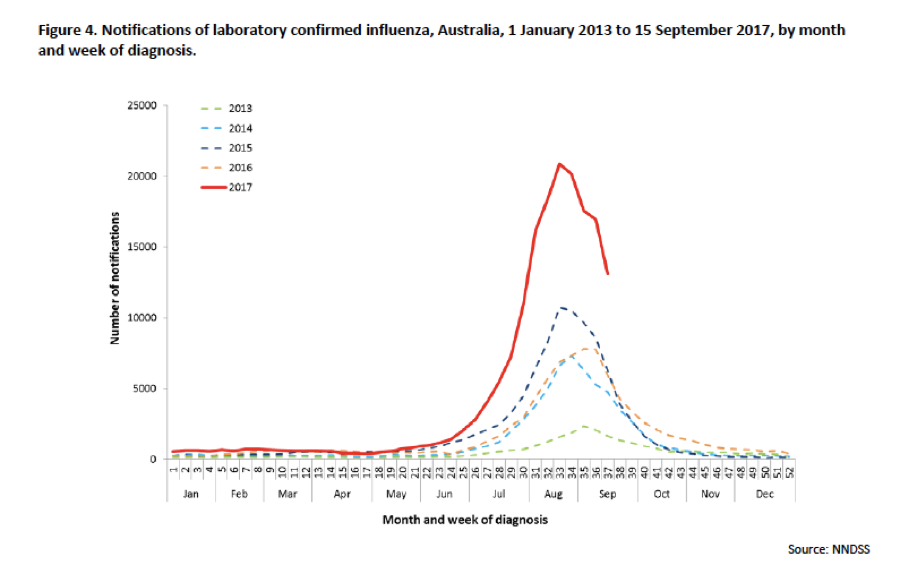
Have you gotten your flu shot yet?
http://www.health.gov.au/internet/main/publishing.nsf/Content/cda-surveil-ozflu-flucurr.htm/$File/ozflu-surveil-no09-2017.pdf
Category: Geriatrics
Posted: 10/1/2017 by Danya Khoujah, MBBS
(Updated: 2/8/2026)
Click here to contact Danya Khoujah, MBBS
Providing consistent, quality emergency care to the elderly is critically important. The Geriatric Emergency Department (GED) guidelines, developed collaboratively, provide a standardized set of guidelines to help improve care of the geriatric population in the emergency department.
In order to improve the standards for geriatric emergency care, representatives from the American College of Emergency Physicians, the American Geriatrics Society, Emergency Nurses Association, and the Society for Academic Emergency Medicine worked together to create the GED Guidelines. These guidelines create a template related to developing a geriatric focused emergency department, including specific recommendations related to staffing and administration, follow up and transition of care, education, quality improvement, equipment and supplies, as well as policies and procedures.
https://www.acep.org/
https://www.acep.org/WorkArea/
Category: Neurology
Keywords: stroke, tPA, thrombolytics, ICH, hemorrhage, adverse events (PubMed Search)
Posted: 9/28/2017 by Danya Khoujah, MBBS
Click here to contact Danya Khoujah, MBBS
Category: Orthopedics
Keywords: ACL tear (PubMed Search)
Posted: 9/23/2017 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Lever Sign/Lelli’s test
A new test for diagnosing ACL tears
Higher sensitivity (94 - 100%) than the Lachman test (highest sensitivity test to date)
With time and more study, this may become our new gold standard physical examination test
Very easy to learn and apply to bedside care
Can help with diagnosing partial tears
Area of manipulation is the femur and not the tibia (as in other tests)
Consider incorporating into your standard knee examination
https://www.youtube.com/watch?v=T9ujIYIctdw
Original study
https://www.ncbi.nlm.nih.gov/m/pubmed/25536951/
Validation
https://www.ncbi.nlm.nih.gov/pubmed/26753117
Thank you to Ari Kestler for sending
https://www.ncbi.nlm.nih.gov/m/pubmed/25536951/
Category: Pediatrics
Keywords: ARDS, oxygenation index, OI, PALICC, acute lung injury (PubMed Search)
Posted: 9/22/2017 by Mimi Lu, MD
(Updated: 10/27/2017)
Click here to contact Mimi Lu, MD
Since the first description of acute respiratory distress syndrome (ARDS), various consensus conferences (including American-European Consensus Conference (AECC) and the Berlin Conference) have produced definitions focused on adult lung injury but have limitations when applied to children.
This prompted the organization of the Pediatric Acute Lung Injury Consensus Conference (PALICC), comprised of 27 experts, representing 21 academic institutions and eight countries. The goals of the conference were 1) to define pediatric ARDS (PARDS); 2) to offer recommendations regarding therapeutic support; and 3) to identify priorities for future research in PARDS.
Although there were several recommendations from the group, some notable ones, in contrast to the Berlin definition focused on adults, include: 1) use the Oxygenation Index (or, if an arterial blood gas is not available, the Oxygenation Severity Index) rather than the P/F ratio; 2) elimination of the requirement for “bilateral” pulmonary infiltrates (may be unilateral or bilateral) 3) elimination of specific age criteria for PARDS.
Tune in next month for pearls on management for children with PARDS...
Pediatric Acute Respiratory Distress Syndrome: Consensus Recommendations from the Pediatric Acute Lung Injury Consensus Conference. Pediatric Acute Lung Injury Consensus Conference Group. Pediatr Crit Care Med. 2015 Jun;16(5):428-39
Collaborators: Jouvet P, Thomas NJ, Wilson DF, Erickson S, Khemani R, Zimmerman J, Dahmer M, Flori H, Quasney M, Sapru A, Cheifetz IM, Rimensberger PC, Kneyber M, Tamburro RF, Curley MA, Nadkarni V, Valentine S, Emeriaud G, Newth C, Carroll CL, Essouri S, Dalton H, Macrae D, Lopez-Cruces Y, Quasney M, Santschi M, Watson RS, Bembea M.
Category: Toxicology
Keywords: Hyperkalemia (PubMed Search)
Posted: 9/22/2017 by Kathy Prybys, MD
(Updated: 10/5/2017)
Click here to contact Kathy Prybys, MD
Hyperkalemia is a potentially life threatening problem which can lead to cardiac dysrhythmias and death. Drug interactions inducing hyperkalemia are extremely common such as the combination of ACE inhibitors and spironolactone or ACE inhibitors and trimehoprim sulfamethoxazole. Hyperkalemia can also occur with a single agent and is a relatively common complication of therapy with trimethoprim sulfamethoxazole. The following drugs can cause hyperkalemia:
Drug induced hyperkalemia. Salem B. Badreddine A, et al. Drug Safety 2014 Sept;37(9) 677-92.
Beta-blockers, trimethoprim-sulfamethoxazole, and the risk of hyperkalemia requiring hospitalization in the elderly: a nested case-control study. Weir MA, Juurlink DN, et al. Clin J Am Soc Nephrol. 2010;5:1544-1551.
Category: International EM
Keywords: Octopus, tetrodotoxin (PubMed Search)
Posted: 9/20/2017 by Jon Mark Hirshon, MPH, MD, PhD
Click here to contact Jon Mark Hirshon, MPH, MD, PhD
The blue-ringed octopus (genus Hapalochlaena) is normally found in the Great Barrier Reef and other coastal waters and tide pools around Australia and other Western Pacific islands. Though not an aggressive animal, when it does bite, such as stepped upon, it can inject tetrodotoxin along with a number of other toxic compounds.
Tetrodotoxin can cause paralysis, leading to respiratory failure and death, though the blockage of voltage-gated fast sodium channel conduction, blocking peripheral nerve conduction. Treatment is supportive, as the venom usually wears off within 4 to 10 hours.
http://emedicine.medscape.com/article/771002-treatment#d10
Category: Critical Care
Posted: 9/19/2017 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Post-Arrest Tidal Volume Setting
Beitler JR, et al. Favorable neurocognitive outcome with low tidal volume ventilation after cardiac arrest. Am J Respir Crit Care Med. 2017; 195:1196-1206.
Category: Pediatrics
Keywords: Sedation, URI, adverse events (PubMed Search)
Posted: 9/15/2017 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Elective surgeries with general anesthesia are often cancelled when the child has an upper respiratory tract infection. What are the adverse events when procedural sedation is used when the child has an upper respiratory tract infection?
Recent and current URIs were associated with an increased frequency of airway adverse events (AAE). The frequency of AAEs increased from recent URIs, to current URIs with thin secretions to current URIs with thick secretions. Adverse events not related to the airway were less likely to have a statistically significant difference between the URI and non-URI groups
AAEs for children with no URI was 6.3%. Children with URI with thick/green secretions had AAEs in 22.2% of cases. Children with URIs did NOT have a significant increase in the risk of apnea or need for emergent airway intervention. The rates of AAEs, however, still remains low regardless of URI status.
Data was collected on over 83,000 patients retrospectively from a voluntary database, The Pediatric Sedation Research Consortium. Children with URIs (no fever) who underwent procedural sedation for things such as imaging or hematology/oncology procedures were included. Propofol, dexmedetomidine, ketamine and opiates were the most commonly used agents.
AAEs included wheezing, secretions requiring treatment, cough, stridor, desaturations, obstruction, snoring, laryngospasm, and apnea.
Mallory et al. Upper Respiratory Infections and Airway Adverse Events in Pediatric Procedural Sedation. Pediatrics. 2017; 140 (1): 1-10.
Category: Toxicology
Keywords: SGLT2 inhibitors, diabetes (PubMed Search)
Posted: 9/14/2017 by Hong Kim, MD
Click here to contact Hong Kim, MD
During the past several years, several new classes of diabetic medications were introduced for clinical use, including SGLT2 inhibitors (canagliflozin, dapagliflozin and empagliflozin).
SGLT2 inhibitors prevent reabsorption of glucose in the proximal convoluted tubules in the kidney and does not alter insulin release.
A recent retrospective study (n=88) of 13 poison center data from January 2013 to December 2016 showed
49 patients were evaluated in a health care facility (HCF) with 18 admissions. Referral to HCF was more common in pediatric patients. This was likely due to unfamiliarity with a new mediation and lack of toxicity data.
Other case reports have shown higher incidence of DKA with the therapeutic use of SGLT2 vs. other classes of DM medications.
Bottom line:
Limit data is available regarding the toxicologic profile of SGLT2 inhibitors.
Based upon this small retrospective study, hypoglycemia may not occur and majority of the patient experience minimal symptoms.
Schaeffer SE et al. Retrospective review of SGLT2 inhibitor exposures reported to 13 poison center. Clin Toxicol (Phila).2017 Aug 16:1-5 PMID: 28812381
Burke KR et al. SGLT2 inhibitors: a systematic review of diabetic ketoacidosis and related risk factors in the primary literature. Pharmacothearpy. 2017;37:187-194
