Category: Toxicology
Keywords: pradaxa, myocardial infarction (PubMed Search)
Posted: 1/19/2012 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Never be the first or last person to use a drug
Vioxx was once touted to be the drug that would be the new standard for anti-inflammatories until it was found to increase your chance of MI by 33% and cause hypertension.
Dabigatran was recently pulled from Japan markets and now is dealing with an impressive meta-analysis by Uchino et al. It showed that dabigatran was significantly associated with higher risk of MI or ACS than other agents.
Control arms (included warfarin, enoxaparin or placebo): MI rate 83 per 10,514
Dabigatran arms: MI rate 237 per 20,000
OR 1.33; 95% CI, 1.03-1.71; p=0.03
The rush for what is perceived as a panaceae for all that is wrong with coumadin could actually cause an MI while it tries to prevent a stroke in nonvalvular a-fib.
Look at the study and decide for yourself and remember Vioxx:
http://archinte.ama-assn.org/cgi/content/full/archinternmed.2011.1666v1
Category: Critical Care
Keywords: fungal, endopthalmitis, ocular, critically ill, systemic infection, immunosupression, IVDA (PubMed Search)
Posted: 1/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Fungal endopthalmitis is an intraocular infection of the aqueous and/or vitreous humor secondary to fungal pathogens; Candida and Aspergillus species are the most common pathogens.
Risk factors: intravenous drug abuse (#1 risk factor), critical illness, systemic fungal infection, immunosuppression (from cancer or medications), diabetes, and alcoholism.
Have a high-index of suspicion for endopthalmitis when patients with systemic fungal disease have visual symptoms; endopthalmitis is present in up to 33% of patients with systemic fungal disease.
Symptoms include:
Inspection of both the anterior and posterior chamber is essential to during evaluation; several small yellow-white circular or “fluffy” lesions with surrounding hemorrhage are demonstrated.
Definitive diagnosis made by vitreous biopsy, culture, or PCR; presumptive treatment is acceptable if systemic fungal disease has been demonstrated.
Treatment with Amphotericin B or Voriconazole may be used for broad-spectrum fungal coverage until specific culture and sensitivities return.
Shah CP, McKey J, Spirn MJ, Maguire J. Ocular candidiasis: a review. Br J Ophthalmol. Apr 2008;92(4):466-8.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: acute MI, MI, myocardial infarction, acute coronary syndrome, painless, presentations (PubMed Search)
Posted: 1/15/2012 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
As many as 1/3 of patients with proven ACS have no chest pain at presentation. Among the more common alternative presentations (anginal equivalents) are dyspnea, diaphoresis, nausea/vomiting, and syncope/near-syncope.
Note also that the absence of pain does not confer a better prognosis. The overall in-hospital mortality rate for patients with painless presentations is 13% vs. 4.3% for patients with chest pain.
Brieger D, et al. Chest 2004; 126:461-469.
Category: Orthopedics
Keywords: intra-articular lidocaine, shoulder dislocation (PubMed Search)
Posted: 1/15/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Approximately 48% of shoulder dislocations occur during sports and recreation.
These are usually first managed in the clinic and sideline setting.
In 6 reviewed studies, 5 used 20mL of 1% lidocaine and 1 used 4 mg/kg of 1% lidocaine.
Patients incurred significantly reduced cost compared to IV sedation
There were no infections, neurovascular damage or systemic effects of the lidocaine.
No significant differences were noted in pain control, success rate or ease of reduction between intra-articular lidocaine and systemic sedation.
The risk of chondrolysis increases with higher concentration and longer duration of exposure to local anesthetics.
There is scant research about the effects of a single exposure of cartilage to lidocaine.
Waterbrook AL & Paul S. Intra-articular lidocaine injection for shoulder reductions: A clinical review. Sports Health, Dec 2011.
Category: Toxicology
Keywords: buprenorphine, Suboxone, overdose, children (PubMed Search)
Posted: 1/10/2012 by Bryan Hayes, PharmD
(Updated: 1/12/2012)
Click here to contact Bryan Hayes, PharmD
Suboxone = buprenorphine and naloxone in a 4:1 ratio, respectively. Formulated in 2 mg or 8mg tablets and film.
Buprenorphine acts as a partial agonist on the mu receptor and an antagonist at the kappa receptor.
If > 2 mg are ingested or age < 2 years old, these patients should be evaluated in an ED as ALL children with > 4 mg ingestion had symptoms.
There is a ceiling effect with respiratory depression however no ceiling with analgesia. This gives buprenorphine a better safety profile compared to methadone.
Onset of symptoms is about an hour and onset of respiratory depression is about 2-3 hours.
Increased doses of naloxone starting at 0.1 mg/kg may be needed to overcome high receptor affinity of buprenorphine. Remember, most children are opioid-naive and will not experience withdrawal symptoms. Repeat doses of naloxone and even infusions may be needed.
In the ED, a minimum of 6 hours observation is necessary. If no clinical effects are noted at 6 hours the patient can safely be discharged, although one small case series recommended 24 hours observation.
Unintentional overdose is common in toddlers, so advise family to keep prescriptions including family pet prescriptions locked (buprenorphine in the IV form is used for veterinary pain control).
Hayes BD, Klein-Schwartz W, Doyon S. Toxicity of buprenorphine overdoses in children. Pediatrics 2008;121(4):e782-6.
Geib AJ, Babu K, Ewald MB, et al. Adverse effects in children after unintentional buprenorphine exposure. Pediatrics 2006;118(4):1746-51.
Category: Critical Care
Posted: 1/10/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Hypertonic Saline for Intracranial Hypertension
Torre-Healy A, Marko NF, Weil RJ. Hyperosmolar therapy for intracranial hypertension. Neurocrit Care 2011.
Category: Visual Diagnosis
Posted: 1/9/2012 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
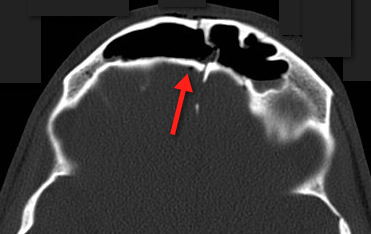
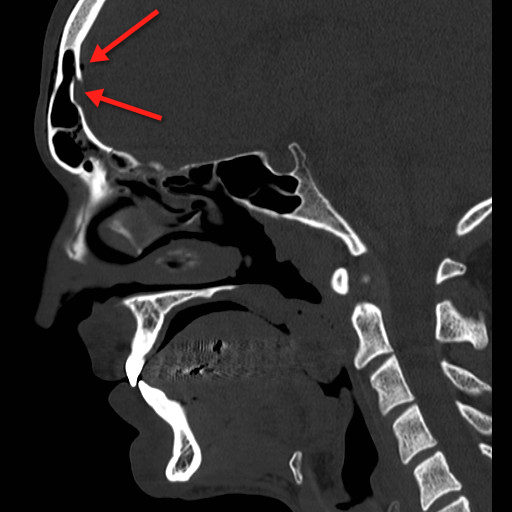
23 year-old male fell off porch while intoxicated. The head CT is shown below. Diagnosis?
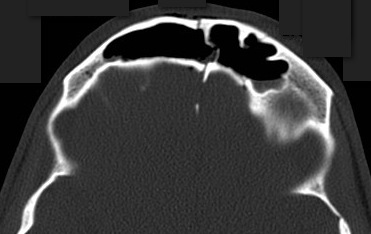
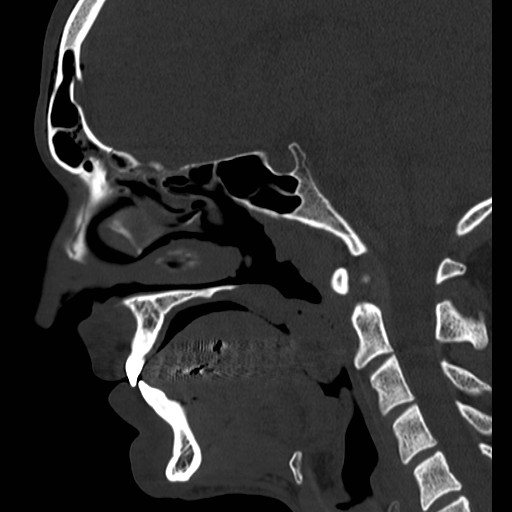
Answer: Frontal sinus fracture (inner and outer table) with pneumocephalus.
A few quick pearls when managing skull fractures:
Medical management:
Surgical management, if:
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: acute MI, MI, myocardial infarction, acute coronary syndrome, cardiac risk factors (PubMed Search)
Posted: 1/8/2012 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
We've noted studies in recent years indicating that cardiac risk factors are ineffective at predicting the likelihood of ACS in patients with acute chest pain (in other words, it's all about the HPI and EKG!). Now there's evidence also that cardiac risk factors are ineffective at predicting in-hospital mortality in patients that rule in for acute MI. [1] In fact, this study actually demonstrated that in-hospital mortality is inversely related to the number of cardiac risk factors!
The bottom line is simple: cardiac risk factors are useful at predicting long-term risk for development of coronary artery disease, but they are NOT useful at in the acute setting.
1. Canto JG, Kiefe CI, Rogers WJ, et al. Number of coronary heart disease risk factors and mortality in patients with first myocardial infarction. JAMA 2011;306:2120-2127.
Category: Pharmacology & Therapeutics
Keywords: cystitis, uti, nitrofurantoin, urinary tract infection (PubMed Search)
Posted: 1/3/2012 by Bryan Hayes, PharmD
(Updated: 1/7/2012)
Click here to contact Bryan Hayes, PharmD
In 2011, updated treatment guidelines were published for acute uncomplicated cystitis and pyelonephritis in women. The recommendations differ from the previous iteration due to increased E. Coli resistance. The good news is we have been ahead of the curve in changing our prescribing habits.
Cystitis (recommendations in order of preference)
Take home points:
Gupta K, et al. International Clinical Practice Guidelines for the Treatment of Acute Uncomplicated Cystitis and Pyelonephritis in Women: A 2010 Update by the Infectious Diseases Society of America and the European Society for Microbiology and Infectious Diseases. Clinical Infectious Diseases 2011;52(5):e103-e120.
Category: Pediatrics
Keywords: sedation, ketamine (PubMed Search)
Posted: 1/6/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
There are limited direct comparisons of (intravenous (IV) vs. intramuscular (IM) ketamine for pediatric procedural sedation in the emergency department. The only RCT comparing IV and IM ketamine was by Roback et al. and compared an IV dose of 1mg/kg vs. IM 4mg/kg. The study authors reported less procedural pain with IM administration compared with IV. However, vomiting occurred more frequently in the IM group, 26.3% compared to 11.9% in the IV group and recovery time was 49 minutes shorter with IV vs IM use.
Route Onset Duration Dose
IM 3-5 min 20-30min 3-5 mg/kg
IV 1 min 5-10 min 1-2 mg/kg
Category: Pharmacology & Therapeutics
Keywords: MRSA, antibiotic, pneumonia, CAP, cephalosporin, infection (PubMed Search)
Posted: 1/5/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Resistance is expected to be limited, with the exception of VRE, and VSE (vanco resistant or sensitive enterococcus faecalis)
Renally excreted
Common side effects: diarrhea, nausea, headache
Serious side effects: anaphylaxis, renal failure, hepatitis, seizure
Low incidence of C. difficile
Dose : 600 mg IV (over 1 hour) q12 hours X 5-7 days
Category: Critical Care
Keywords: blunt trauma, vascular inury, anticoagulation, thrombosis, emboli (PubMed Search)
Posted: 1/3/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Carotid or vertebral artery injury following blunt trauma is a rare (%1 of blunt trauma), but a potentially serious injury potentially causing stroke and long-term disability.
Injury leads to an intimal tear becoming a nidus for platelet aggregation; thrombosis and/or distal emboli may subsequently develop.
Mechanisms of injury include:
Symptoms of carotid injury may include contralateral sensorimotor deficits; Symptoms of vertebral injury may include ipsilateral facial pain and numbness, headache, ataxia, or dizziness.
Angiography is the diagnostic “gold standard” but these days a 16-slice CT angiography (or greater) is a reliable screening tool.
Anticoagulation with heparin is the treatment of choice for severe injury, if there are no contraindications (e.g., intracranial bleeding). Anti-platelet drugs may be acceptable in certain cases.
Kim YK, Schulman S. Cervical artery dissection: pathology, epidemiology and management. Thromb Res. Apr 2009;123(6):810-21.
Schievink WI. Spontaneous dissection of the carotid and vertebral arteries. N Engl J Med. Mar 22 2001;344(12):898-906.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: clopidogrel, cardiogenic shock, acute coronary syndrome (PubMed Search)
Posted: 1/1/2012 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Patients with ACS are often treated early with clopidogrel. However, if the patient with ACS appears to be developing cardiogenic shock, its probably best to withhold the early clopidogrel. The literature indicates that patients with cardiogentic shock benefit most from emergent PCI, and many of these patients will need CABG. Generally it's best to avoid clopidogrel in patients heading for CABG.
The use of clopidogrel in patients with cardiogenic shock can be deferred to the cardiologists in the cath lab once they decide whether the patient will need CABG or not.
Thiele H, Allam B, Chatellier G, et al. Shock in acute myocardial infarction: the Cape Horn for trials? Eur Heart J 2010;31:1828-1835.
Category: Misc
Keywords: Triage, Mass Causality (PubMed Search)
Posted: 12/31/2011 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
START Triage
START triage is a simple system to implement that does not require any special equipment in order to determine who needs immediate, delayed or non-urgent care during a mass causality.
START stands for Simple Triage And Rapid Treatment. Patients are triaged based on 4 factors:
The steps are:
So those that can leave are green, those that do not meet any of the START criteria are YELLOW, and those with any of the four factors are RED or DEAD.
Category: Pediatrics
Posted: 12/30/2011 by Rose Chasm, MD
(Updated: 2/8/2026)
Click here to contact Rose Chasm, MD
Pediatrics Board Review, MedStudy
Category: Toxicology
Keywords: pradaxa, xarelto (PubMed Search)
Posted: 12/29/2011 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Another great example of the generic drug name being so difficult to pronounce you have no choice but to say - Xarelto. The drug touts ease of use and no need for hematologic monitoring like Pradaxa. This drug has the same indication for stroke prevention in nonvalvular atrial fibrillation. It also is being used in DVT prophylaxis in hip and knee surgeries.
Differences:
- Selective Factor Xa inhibitor unlike Pradaxa which is a competetive direct thrombin inhibitor
- Once a day dosing instead of twice a day for Pradaxa
Same concerns:
- No real reversal but can use FFP in a pinch
- Recommend waiting 24 hrs DC med to perform surgical procedure - this includes LP. I am personally waiting for the first case report of LP performed in ED on a patient taking either Xarelto or Pradaxa with subsequent epidural hematoma. Someone is bound to miss this on the med list. Be careful.
Even if your hospital has not added it to its formulary, you will see patients on this drug in the ED.
Category: Neurology
Keywords: NIH Stroke Scale, stroke (PubMed Search)
Posted: 12/28/2011 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 12/27/2011 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
VBG to Assess Respiratory Function?
Kelly AM. Can venous blood gas analysis replace arterial in emergency medical care? Emerg Med Australasia 2010;22:493-498.
Category: Visual Diagnosis
Posted: 12/26/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
64 year old male with emphysema and stage 4 lung cancer presents in respiratory distress. What's the diagnosis?
Answer: Pneumothorax (left chest) and bullous disease (right chest).
In questionable cases like this, bedside ultrasound can help distinguish between bullae and pneumothorax. Bullae should have a positive lung sliding sign whereas pneumothorax does not.
See the referenced case report for more information:
Simon, B. et al. Two cases where bedside ultrasound was able to distinguish pulmonary bleb from pneumothorax. J Emerg Med. 2005 Aug;29(2):201-5.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: obesity, cardiovascular disease, acute myocardial infarction, CAD (PubMed Search)
Posted: 12/25/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Feeling a bit guilty about over-eating during these holidays? Here's a study that might make you feel just a tad bit better about those extra pounds. (Just a tad.)
Auer and colleagues reviewed coronary angiograms of over 1000 patients and correlated them with body fat percentage. After statistical analysis, they found that body fat was not associated with the presence (or absence) or severity (size of coronary lesions) of atherosclerosis in men or women. Furthermore, the results did not differ based on age.
What's the takeaway point? Simple: go ahead and have that second serving of ham and eat that extra slice of cake!
[disclaimer: This study has not necessarily been reproduced, and is not intended to give free license to gorge after the holidays are done. It is fully expected that starting on January 2 you will immediately forget all of the above and renew your commitment to a healthy lifestyle consisting of a bland diet and P90X or Insanity workouts on a daily basis. But until then, forget the guilt!]
Auer J, et al. Obesity, body fat, and coronary atherosclerosis. Int J Cardiol 2005
