Category: Orthopedics
Keywords: Posterolateral Corner, knee (PubMed Search)
Posted: 9/17/2011 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
Posterolateral Corner Injuries
The posterolateral corner “PLC” of the knee is becoming increasingly recognized as an extremely important structure to maintain the stability of the knee joint.
PLC injuries occur with hyperextension, varus load and tibial external rotation. So the most common mechanism is a posterolaterally directed blow to the anteromedial tibia when the knee is hyperextended. PLC injuries are commonly associated with injury to other ligaments (ACL, PCL, LCL) and occur in isolation in <5% of cases. If suspected make sure to check for other ligamentous injuries.
Since this injury can be missed and is associated with significant disability it is important to test for it. This YouTube video, http://youtu.be/bnXaTdvZZ6o, demonstrates several examination techniques that can identify the injury.
Wheeless Online Ortho Reference http://www.wheelessonline.com/ortho/posterolateral_rotary_instability_of_the_knee
Category: Neurology
Keywords: bell palsy, bell's palsy, cranial nerve seven palsy, facial paralysis (PubMed Search)
Posted: 9/14/2011 by Aisha Liferidge, MD
(Updated: 2/7/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: Procedures, Arterial lines, Axillary, hemodynamic monitoring (PubMed Search)
Posted: 9/13/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Radial and femoral arteries are common sites for arterial-line placement, but are not without complications (e.g., Radial artery: malfunction with positioning and Femoral artery: contamination and infection); an alternative site to consider is the axillary artery.
The axillary artery's superficial location and large size make it a desirable choice for cannulation.
The "anatomical-landmark" and "palpation" methods have been the traditional techniques of axillary arterial cannulation, however these methods may be difficult for to a variety of reasons (e.g., obesity, anasarca, arterial disease, etc.)
Ultrasound allows visualization of the axillary artery and avoids unintended injury to structures in close proximity (e.g., brachial plexus, pleura, axillary vein, etc.); please see figures 1 and 2 in the referenced Sandhu article and http://www.youtube.com/watch?v=Z31YiyV7cNQ.
A recent study (Killu, 2011) found that ultrasound increases success rates when compared to the traditional landmark approach.
Killu, K. et al. Utility of Ultrasound Versus Landmark-Guided Axillary Artery Cannulation for Hemodynamic Monitoring in the Intensive Care Unit. ICU Director; 2011. 2(3), 54–59.
Sandhu, N. The Use of Ultrasound for Axillary Artery Catheterization Through Pectoral Muscles: A New Anterior Approach. Anesthesia and analgesia. 2004; 562–565.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 9/12/2011 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
A 50 year-old patient presents after a self-inflicted eye injury. The patient had taken some type of needle and inserted it into their eye.
What is the diagnosis and what complications might result?
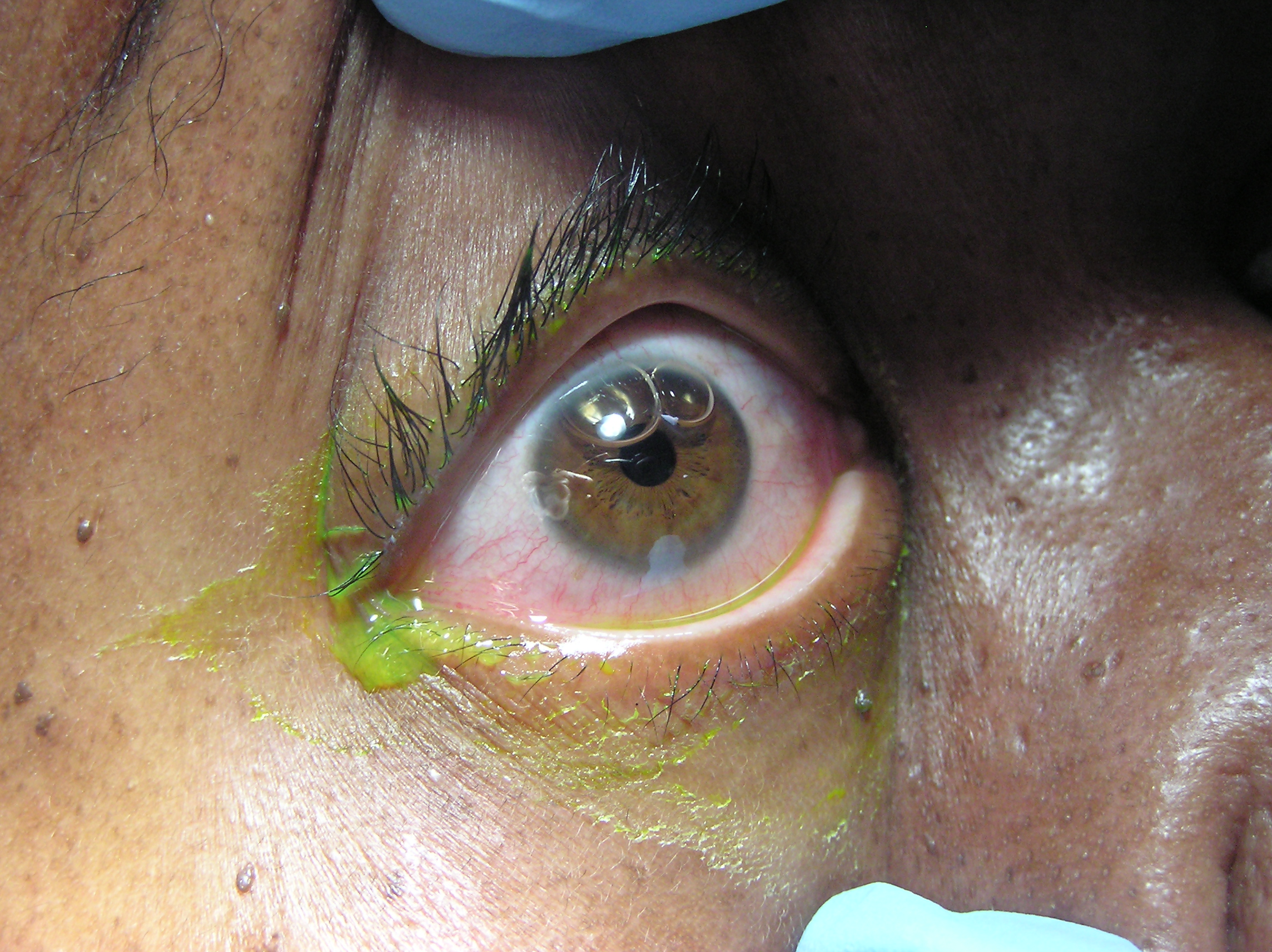
The image shows air bubbles in the anterior chamber. Since air has been introduced into the eye, the patient is at risk for elevated intraocular pressures. In addition, you would need to consider endophthalmitis as a complication.
Category: Cardiology
Keywords: troponin, supraventricular tachycardia, svt, dysrhythmia, tachydysrhythmia, tachycardia (PubMed Search)
Posted: 9/11/2011 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
SVT is rarely, if ever, the presenting rhythm associated with an acute MI. As a result, physicians should not feel compelled to send troponin levels and perform rule-outs purely based on an SVT presentation. Instead, the decision to rule out a patient presenting with SVT should be based on whether there is a constellation of other concerning symptoms, exclusive of the SVT (e.g. if the patient presented with chest pressure radiating down the arm and diaphoresis, in addition to the SVT).
Two recent studies confirmed that routine troponin testing in patients with SVT is extremely low-yield, and instead often produces false-positive troponin results that lead to unnecessary admissions and workups. In other words, mild troponin elevations may occur in SVT but they do not correlate with true ACS.
Bukkapatnam RN, Robinson M, Turnipseed S, et al. Relationship of myocardial ischemia and injury to coronary artery disease in patients with supraventricular tachycardia. Am J Cardiol 2010;106:374-377.
Carlbert DJ, Tsuchitani S, Barlotta KS, et al. Serum troponin testing in patients with paroxysmal supraventricular tachycardia: outcome after ED care. Am J Emerg Med 2011;29:545-548.
Category: Orthopedics
Keywords: knee dislocation, ABI, vascular (PubMed Search)
Posted: 9/10/2011 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Evaluation of circulatory status is the most important aspect of post reduction care.
Look for hard findings such as cool/cold lower extremity, diminished or absent pulses, pale or dusky skin, paralysis, etc.
However, the absence of these findings should not lull the clinician into a false sense of security. The degree of initial joint deformity, presence of full bounding pulses and warm skin over the dorsum of the foot can all be present in the setting of vascular injury.
The next step will be to perform an ABI (ankle-brachial index).
In one small study, no patient with an ABI greater than or equal to 0.9 had a vascular injury.
Patients with a reassuring physical exam and ABIs should be admitted for vascular checks without further imaging.
Patients with a reassuring physical examination but with an abnormal ABI should have an imaging study obtained (arteriogram/CT angiogram).
Patients with hard findings of a vascular injury should have an emergent vascular surgery consultation.
The value of the ankle-brachial index for diagnosing arterial injury after knee dislocation: a prospective study.
Category: Pediatrics
Posted: 9/9/2011 by Rose Chasm, MD
(Updated: 2/7/2026)
Click here to contact Rose Chasm, MD
MedStudy Pedatrics Board Review, Core Curriculum, Book 3 2004
Category: Toxicology
Keywords: adenosine, central line (PubMed Search)
Posted: 8/29/2011 by Bryan Hayes, PharmD
(Updated: 9/8/2011)
Click here to contact Bryan Hayes, PharmD
Every so often a patient arrives in PSVT with their only intravenous access being through a hemodialysis port.
Initial dose of adenosine should be reduced to 3 mg if administered through a central line. Remember a central line delivers the adenosine right where you need it. This recommendation is supported by the 2010 ACLS guidelines. Second and third doses should be 6 mg (instead of 12 mg).
Cases of prolonged bradycardia and severe side effects have been reported after full-dose adenosine through a central line. Other situations to consider lower doses include patients currently receiving carbamazepine or dipyridamole or in those with a transplanted heart.
McIntosh-Yellin NL, et al. Safety and efficacy of central intravenous bolus administration of adenosine for termination of supraventricular tachycardia. J Am Coll Cardiol 1993;22:741–5.
Chang M, et al. Adenosine dose should be less when administered through a central line. J Emerg Med 2002;22(2):195-8.
Neumar RW, et al. Part 8: Adult Advanced Cardiovascular Life Support: 2010 American Heart Association Guidelines for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care. Circulation 2010;122:S729-S767.
Category: Neurology
Keywords: encephalitis, meningitis, acyclovir, headache, fever (PubMed Search)
Posted: 9/7/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 9/6/2011 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Fungal Sepsis in the Critically Ill
Lepak A, Andes D. Fungal sepsis: Optimizing antifungal therapy in the critical care setting. Crit Care Clin 2011; 27:123-147.
Category: Visual Diagnosis
Posted: 9/4/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
26 year old male presents s/p basketball dunk. Diagnosis?

Answer: Talar dislocation
Below, a post-reduction Xray, as well as a link to a video demonstrating a few ankle reductions (the video's background music makes all the difference): http://www.youtube.com/watch?v=AzqCsLX1K1E

Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: atherosclerosis, coronary artery disease (PubMed Search)
Posted: 9/4/2011 by Amal Mattu, MD
(Updated: 2/7/2026)
Click here to contact Amal Mattu, MD
Approximately 7-10% of cases of ACS are not related to atherosclerotic coronary disease. Some other causes of ACS include the following:
trauma
vasculitis
congenital abnormalities
emboli (e.g. bacterial)
thoracic aortic dissection
infectious diseases
DIC, TTP
These conditions can produce ST-segment changes that resemble those of true STEMI or non-STEMI, and therefore some of these patients are diagnosed retrospectively after a negative catheterization.
Category: Orthopedics
Keywords: Sugar Tong Splint (PubMed Search)
Posted: 9/3/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Sugar Tong Splint
The sugar tong splint is ideal for splinting fractures of the radius, ulna, or wrist. It prevents flexion and extension at the wrist, limits flexion and extension at the elbow, and prevents supination and pronation. A posterior long arm splint does not prevent supinaton and pronation, therefore, it is of limited use for radius and ulna fractures.
The traditional sugar tong can be difficult to put on a patient without an assistant as it is often hard to hold the splint in position as you begin to ace wrap it. A variation on the sugar tong, the reverse sugar tong, prevents this frustration. The splinting material is cut so that a small piece suspends the splint from the web space between the thumb and index finger. The open ends at the elbow are also easily folded under each other, preventing any bulky splint material from extending out.

The reverse sugar tong is on the left, the original sugar tong on the right.
Check out this video showing how to place a reverse sugar tong splint.
http://www.youtube.com/watch?v=r-RHdttOMf0
Category: Pharmacology & Therapeutics
Keywords: thrombin,dabigatran,partial thromboplastin,bleeding (PubMed Search)
Posted: 9/1/2011 by Ellen Lemkin, MD, PharmD
(Updated: 2/7/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Rye J, Stangier J, Haertter S, et al. Dabigatran etexilate - a novel, reversible, oral direct thrombin inhibitor: Interpretation of coagulation assays and reversal of anticoagulant activity. Thrombosis and Haemostasis 2010. 103;1116-27.
Category: Neurology
Keywords: delirium (PubMed Search)
Posted: 8/31/2011 by Aisha Liferidge, MD
(Updated: 2/7/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: ultrasound, tracheal intubation, esophageal intubation, critical care, airway (PubMed Search)
Posted: 8/30/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Multiple methods of confirming endotracheal tube placement exist, however quantitative waveform capnography is the most reliable method. Unfortunately this may not be immediately available at all medical centers.
Recent studies demonstrate that bedside ultrasound may assist in the detection of proper endotracheal tube placement.
The T.R.U.E. (Tracheal Rapid Ultrasound Exam) was demonstrated to be 99% sensitive, 94% specific, 99% PPV, and 94% NPV during intubation.
The basic exam involves placing a high-frequency linear-array probe on the anterior neck above the sternal notch and identifying the trachea and esophagus during intubation.
The following video is an example of what you DO NOT want to see during an intubation: http://www.youtube.com/watch?v=LvfThxhQ93A
Chou, H. et al. Tracheal rapid ultrasound exam (T.R.U.E.) for confirming endotracheal tube placement during emergency intubation. Resuscitation. Jun 2011
Werner SL,et al. Pilot study to evaluate the accuracy of ultrasonography in confirming endotracheal tube placement. Ann Emerg Med 2007;49:75–80.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/29/2011 by Rob Rogers, MD
(Updated: 2/7/2026)
Click here to contact Rob Rogers, MD
Patient presents with right-sided chest and shoulder pain....
What's the diagnosis?

Herpes Zoster
Category: Cardiology
Keywords: therapeutic hypothermia, induced hypothermia, cardiac arrest, post arrest care (PubMed Search)
Posted: 8/28/2011 by Amal Mattu, MD
(Updated: 2/7/2026)
Click here to contact Amal Mattu, MD
If you're like me, you've been a bit confused about what exactly defines "coma" in the current recommendations for post-arrest hypothermia in "comatose" patients with return of spontaneous circulation. Fortunately, a recent NEJM article has helped clarify this by suggesting that hypothermia should be induced in these post-arrest patients with either:
Naturally, if the patient was comatose before the arrest, don't bother.
Holzer M. Targeted temperature management for comatose survivors of cardiac arrest. N Engl J Med 2010;363:1256-1264.
Category: Orthopedics
Keywords: knee dislocation (PubMed Search)
Posted: 8/27/2011 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Stability from 4 major ligaments (ACL, PCL, MCL and LCL)
Knee dislocation causes injury to multiple ligaments (usually 3 of the above).
Many of these dislocation spontaneously reduce prior to medical evaluation. Therefore, consider knee dislocation in a patient with multi ligament injury, significant hemarthrosis and bruising.
Vascular injury in up to 40% (popliteal artery)
Nerve injury in up to 23% (peroneal nerve) ((ankle dorsiflexion and sensation to the first web space of the foot))
After reduction, immobilize knee in 15-20 degrees flexion.
The degree of initial deformity, presence of strong pulses, or warm skin cannot be used to rule out popliteal injury.
Category: Pediatrics
Keywords: severe asthma, decreased hospitalization (PubMed Search)
Posted: 8/26/2011 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
