Category: Critical Care
Posted: 5/8/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Severe acute pancreatitis (SAP) is a life-threatening form of pancreatitis, with up to 30% mortality.
SAP may lead to hypovolemic shock (secondary to vasodilation and capillary leak), hypoxemia (from acute respiratory distress syndrome), and multi-organ failure.
Suspect SAP with signs and symptoms of pancreatitis plus any of the following:
Treatment of SAP should focus on:
Greer, S. E., & Burchard, K. W. (2009). Acute pancreatitis and critical illness: a pancreatic tale of hypoperfusion and inflammation. Chest, 136(5), 1413–1419.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: mortality, coronary artery disease, myocardial infarction (PubMed Search)
Posted: 5/6/2012 by Amal Mattu, MD
(Updated: 2/9/2026)
Click here to contact Amal Mattu, MD
Increasing literature over recent years has demonstrated that young women (1) DO have MIs, (2) present more atypically than men, and (3) are more often misdiagnosed than men. Two recent trials have now also confirmed that young women have a higher in-hospital mortality compared to men, even when properly diagnosed. They may be due to lack of aggressive workups or treatment, or perhaps other as-yet unidentified factors.
The takeaway points are simple: be very wary when women (incuding young women) present with any cardiopulmonary complaints or anginal equivalent-type symptoms; and treat them aggressively.
1. Zhang Z, et al. Age-specific gender differences in in-hospital mortality by type of acute myocardial infarction. Am J Cardiol 2012;109:1097-1103.
2. Canto JG, et al. Association of age and sex with myocardial infarction symptom presentation and in-hospital mortality. JAMA 2012;307:813-822.
Category: Pharmacology & Therapeutics
Keywords: older adult, Beers Criteria, geriatric (PubMed Search)
Posted: 4/30/2012 by Bryan Hayes, PharmD
(Updated: 6/15/2012)
Click here to contact Bryan Hayes, PharmD
The American Geriatrics Society updated Beers Criteria for potentially inappropriate medication use in older adults is now available.
The update differs in several ways from the 2003 edition. Medications that are no longer available have been removed, and drugs introduced since 2003 have been added. Research on drugs included in earlier versions has been updated and new information is provided about appropriate prescribing of medications for an expanded list of common geriatric conditions.
Here is an abbreviated list of medications/classes on the list that we may use in the ED. Use caution.
The American Geriatrics Society 2012 Beers Criteria Update Expert Panel. American Geriatrics Society Updated Beers Criteria for Potentially Inappropriate Medication Use in Older Adults. J Am Geriatr Soc 2012;60(4):616-31.
Follow me on Twitter (@pharmERtoxguy).
Category: Pharmacology & Therapeutics
Keywords: MRSA, antibiotic, pneumonia, VAP, cephalosporin, infection (PubMed Search)
Posted: 5/3/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
If vancomycin resistance is suspected with MRSA infections, there are several other antibiotic choices. They are all extremely expensive.
| Antibiotic | ORAL | Indication | Precaution |
| Telavancin | N | SSTI | May cause QT prolongation: Caution with azole antifungals, class III antiarrhythmics, antidepressants, antipsychotics. Interferes with coagulation tests. |
| Daptomycin | N | SSTI Bacteremia Endocarditis | Not for pneumonia. May cause rhabdomyolysis; Discontinue statins. |
| Linezolid | Y | VAP SSTI | Not for bacteremia. May cause serotonin syndrome; Caution with antidepressants, antipsychotics, tramadol, methadone. |
| Tigecycline | N |
Intrabdominal infections SSTI | Not for bacteremia. Inhibits clearance of warfarin. Reserve for polymicrobial infections. |
Skin and soft tissue infection (SSTI); ventilator acquired pneumonia (VAP)
Category: Critical Care
Keywords: spontaenous bacterial peritonitis, hepatorenal syndrome, albumin (PubMed Search)
Posted: 5/1/2012 by Mike Winters, MBA, MD
(Updated: 2/9/2026)
Click here to contact Mike Winters, MBA, MD
SBP, HRS, and Albumin
Bernardi M, et al. Human albumin in the management of complications of liver cirrhosis. Crit Care 2012; 16:211.
Category: Visual Diagnosis
Posted: 4/29/2012 by Haney Mallemat, MD
(Updated: 4/30/2012)
Click here to contact Haney Mallemat, MD
68 yo man presents with new-onset seizures; his CT is shown below. What is your differential diagnosis?
Cerebral Ring-Enhancing Lesions
Neoplasm
Infectious
Neurologic
Bonus pearl: Do you like Emergency Ultrasound and want a quick review before you scan your next patient? Well, check out the "One-minute Ultrasound App". It's provides a quick review for many essential ultrasound studies...and yes, it's FREE for both iphone and android.
Iphone: http://itunes.apple.com/us/app/one-minute-ultrasound/id512301845?mt=8&ls=1
Garg, R., Sinha, M. Multiple ring-enhancing lesions of the brain. J Postgrad Med. 2010 Oct-Dec; 56(4):307-16
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: radiation, coronary artery disease, stress testing, cardiac testing (PubMed Search)
Posted: 4/29/2012 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Here's some numbers to consider regarding typical radiation exposre associated with cardiac imaging tests relative to naturally occurring background radiation exposure:
Test type Relative exposure
Naturally occurring annual background radiation
exposure for a person living in the US (~ 3 mSv) 1
Coronary artery calcium score 0.5
Cardiac CT angiography 1-4
Nuclear stress test (single-photon emission CT) 3-4
Exercise treadmiil testing (with no imaging) 0
Cardiac MRI/echocardiogram 0
[above estimates are typical, but may vary between individuals and among different centers]
Blankstein R. Introduction to noninvasive cardiac imaging. Circulation 2012;125:e267-3271.
Category: Orthopedics
Keywords: Inferior shoulder dislocation (PubMed Search)
Posted: 4/28/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Luxatio erecta, aka inferior shoulder dislocation, is an uncommon form of shoulder dislocation (0.5-2%)
2 Mechanisms: 1) Forceful, direct axial loading of an ABducted arm.
2) Hyperabduction of the arm leads to impingement of the humeral head against the acromion, If forceful enough, this leverage can rupture the capsule and drive the humeral head downward, resulting in an inferior dislocation. This mechanism is more common.
Classic presentation: Arm locked in marked ABduction with the flexed forearm lying above the head.
http://uconnemig.files.wordpress.com/2011/11/emimages-8c.jpg
http://img.medscape.com/pi/features/slideshow-slide/sdrt/fig1.jpg
http://www.mypacs.net/repos/mpv3_repo/viz/full/76563/3828172.jpg
One may palpate the humeral head against the lateral chest wall
Bony injuries include fractures to surrounding structures such as the coracoid process, acromion, glenoid rim, clavicle, greater tuberosity and humeral head.
Nerve injuries include damage to the brachial plexus/axillary nerve (usually reversed with reduction)
Vascular injuries: Axillary artery thrombosis
Category: Pediatrics
Keywords: drowning, submersion, seizure, intubation (PubMed Search)
Posted: 4/27/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Submersion injuries are the 2nd leading cause of accidental death in children with 1/3 of survivors sustaining significant neurologic sequelae. 50% of drownings occur from May to August.
40% of all drowning victims are children under age 4, with males affected 3 times as often as females. Most drownings occur with 10 feet of safety. Infants and toddlers drown most often in bathtubs (especially if <1 year old), buckets, toilets, pools and hot tubs (most often the pools are in-ground). Those with seizure disorders have a 10-14 fold higher likelihood of drowning.
Aspiration of as little as 1-3ml/kg of fluid may cause pulmonary edema, surfactant inactivation or washout, pulmonary shunting with resulting V/Q mismatching, or direct injury to the alveolar membrane.
Immediate and adequate resuscitation, including intubation, is the single most important factor determining survival. Always check body temperature as hypothermia is common. In general, prophylactic antibiotics and steroids are not indicated unless drowning occurred in grossly contaminated water/sewage.
Category: Toxicology
Keywords: sedation, dexmedetomidine (PubMed Search)
Posted: 4/26/2012 by Fermin Barrueto
(Updated: 2/9/2026)
Click here to contact Fermin Barrueto
Dexmedetomidine is an alpha2-agonist that has a similiar mechanism of action to clonidine. Short half-life and no respiratory depression make it possibly more effective than propofol in procedural sedation. Cost/Availability are the biggest barriers. Transient bradycardia is also possible but the actual incidence of clinically significant bradycardia is not yet elucidated.
I am still awaiting the first emergency department study looking at dexmedetomidine for procedural sedation.
A recent article actually brought up the possibility of utilizing it intranasally which could have some tantalizing pediatric applications.
Yuen VM, Irwin MG, Hui TW, Yuen MK, Lee LH.
Anesth Analg. 2007 Aug;105(2):374-80.
Category: Critical Care
Posted: 4/24/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
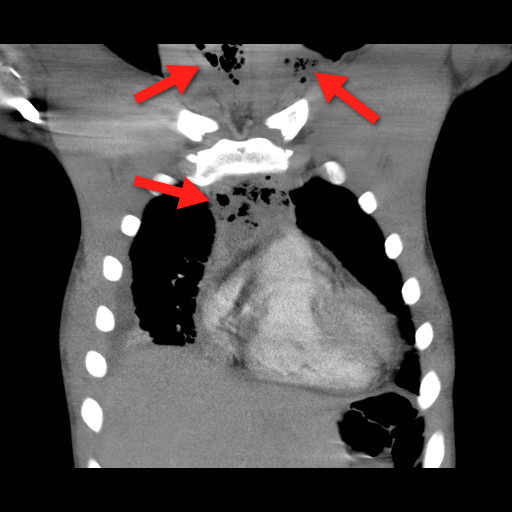
Mediastinitis is an infection of the mediastinum; a rapidly fatal surgical emergency if not recognized and treated early.
Causes include esophageal perforation, oropharyngeal infections (e.g., Ludwig’s angina), prevertebral or carotid space infections, and iatrogenically (endoscopy, hypopharyngeal perforations during intubation, etc.).
Plain films (neck / chest) may serve as a screening tool, but CT best defines the source and extent of disease; the CT below demonstrates gas within the soft-tissues and the mediastinum (red arrrows).
Infections may be polymicrobial and broad-spectrum antibiotics with anaerobic coverage (e.g., pipercillin-tazobacam) should be started initially.
Immediate treatment should also include:
Bonus Pearl
Can't keep up with all the great educational stuff in Emergency Medicine and Critical Care? Let the professionals at Life in the Fastlane do it for you (http://lifeinthefastlane.com). These guys scour the web and blog about the best educational pearls, podcasts, and radoiolgic finds...and they're also quite the laugh. Check them out today!
Ridder G, et al. Descending necrotizing mediastinitis: contemporary trends in etiology, diagnosis, management, and outcome. Ann Surg. Mar 2010;251(3):528-34.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: ECG, EKG, electrocardiogram, electrocardiography, acute coronary syndrome (PubMed Search)
Posted: 4/23/2012 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
[Pearl provided by Dr. Semhar Tewelde]
Who are the experts at deciphering ECG's
Authors looked at 240 ECGs which activated the cath lab activation for STEMI. They excluded patients with LBBB or paced rhythms. Retrospective chart reviews were used to determine if there was actually a STEMI. The ECGs were then shown to 7 experienced interventional cardiologists and interpreted for acute STEMI.
Of 84 subjects, there were 40 patients with a true STEMI and 44 without (13 of whom had NSTEMI) Recommendations for immediate PCI varied widely, from 33%-75%. Sensitivities were 53%-83%, specificities 32%-86%, PPV 52%-79%, and NPV 67%-79%. When the cardiologist chose non-ischemic ST elevation, LVH was thought to be the cause in 6% to 31% and old MI/aneurysm in 10% to 26%.
Moral, even cardiologists can be wrong... EM physicians must scrutinize every ECG and challenge ourselves to be the best at interpreting ECG's.
Reference:Tran V, Huang HD, Diez JG, et al. Differentiating ST-elevationmyocardial infarction from nonischemic ST-elevation in patients with chestpain. Am J Cardiol 2011;108(8):1096-101.
Category: Orthopedics
Posted: 4/21/2012 by Michael Bond, MD
(Updated: 2/9/2026)
Click here to contact Michael Bond, MD
Some quick board review pearls. Remember these fractures/dislocations and the neurologic injury that is associated with them
Category: Pediatrics
Keywords: transfusion, anemia, hemoglobin (PubMed Search)
Posted: 4/20/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Children are at higher risk for complications related to the transfusion of blood products compared with adults. So when should we consider transfusion?
Normal hemoglobin values:
- highest at birth (14 - 24 g/dL),
- decreasing to 8 to 14 g/dL at 3 months,
- increasing to 10 to 14 g/dL at age 6 months to 6 years, 11 to 16 g/dL at age 7 to 12 years, and 11.5 to 18 g/dL in adulthood.
- Although the number of platelets are in the normal range at birth, their function is impaired.
For infants younger than 4 months, thresholds for red blood cell transfusions:
- hemoglobin levels are 12 g/dL for preterm infants or term infants born anemic,
- 11 g/dL for chronic oxygen dependency,
- 12 to 14 g/dL for severe pulmonary disease,
- 7 g/dL for late anemia in a stable infant,
- 12 g/dL for acute blood loss exceeding 10% of estimated blood volume.
For infants older than 4 months, thresholds for red blood cell transfusions:
- hemoglobin levels are 7 g/dL in a stable infant,
- 7 to 8 g/dL in a critically unwell infant or child,
- 8 g/dL in an infant or child with perioperative bleeding,
- 9 g/dL in an infant or child with cyanotic congenital heart disease (increased oxygen demand).
- 9 g/dl in children with thalassemia major (to slow bone marrow stimulation)
For children with sickle cell disease (SCD):
- threshold is 7 to 9 g/dL, or more than 9 g/dL if the child has previously had a stroke.
- perioperatively for major surgery: 9 to 11 g/dL, and sickle hemoglobin should be less than 30%, or less than 20% for thoracic or neurosurgery.
Bottom line:
A threshold of 7 g/dL is indicated for the transfusion of packed red blood cells in most children.
Reference:
1) Transfusion guidelines in children. Anasethesia and Intensive Care Medicine. 2012;13(1);20–23.
2) Medscape clinical education briefs
Category: Critical Care
Posted: 4/17/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Cuff Pressures and the Prevention of VAP
Grap MJ, et al. Ventilator-associated pneumonia: The potential critical role of emergency medicine in prevention. JEM 2012; 42:353-362.
Category: Visual Diagnosis
Posted: 4/15/2012 by Haney Mallemat, MD
(Updated: 4/16/2012)
Click here to contact Haney Mallemat, MD
67 yo male presents with burning substernal chest pain; worse with meals and when supine. What's the diagnosis?
Answer: Hiatal hernia
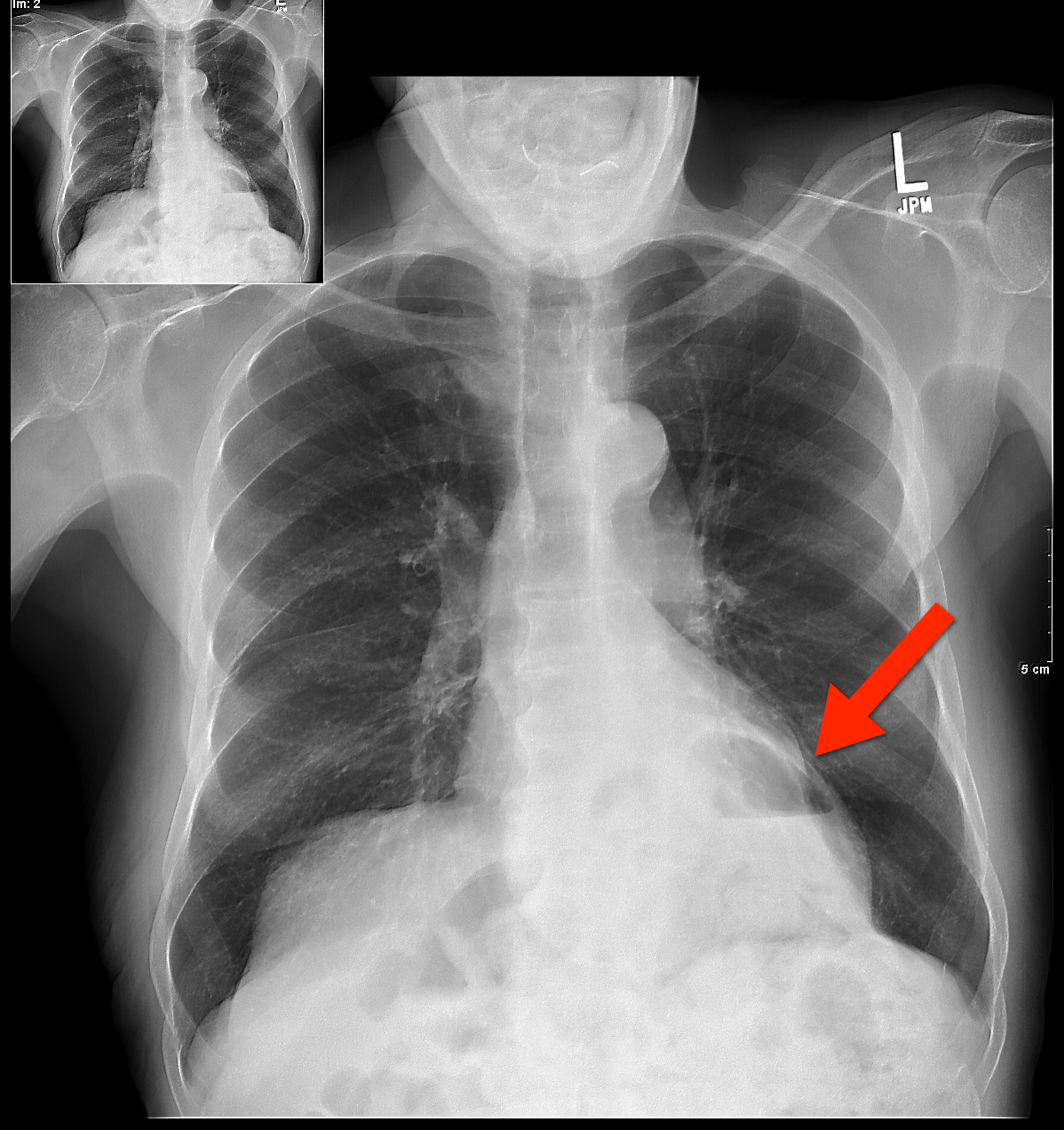
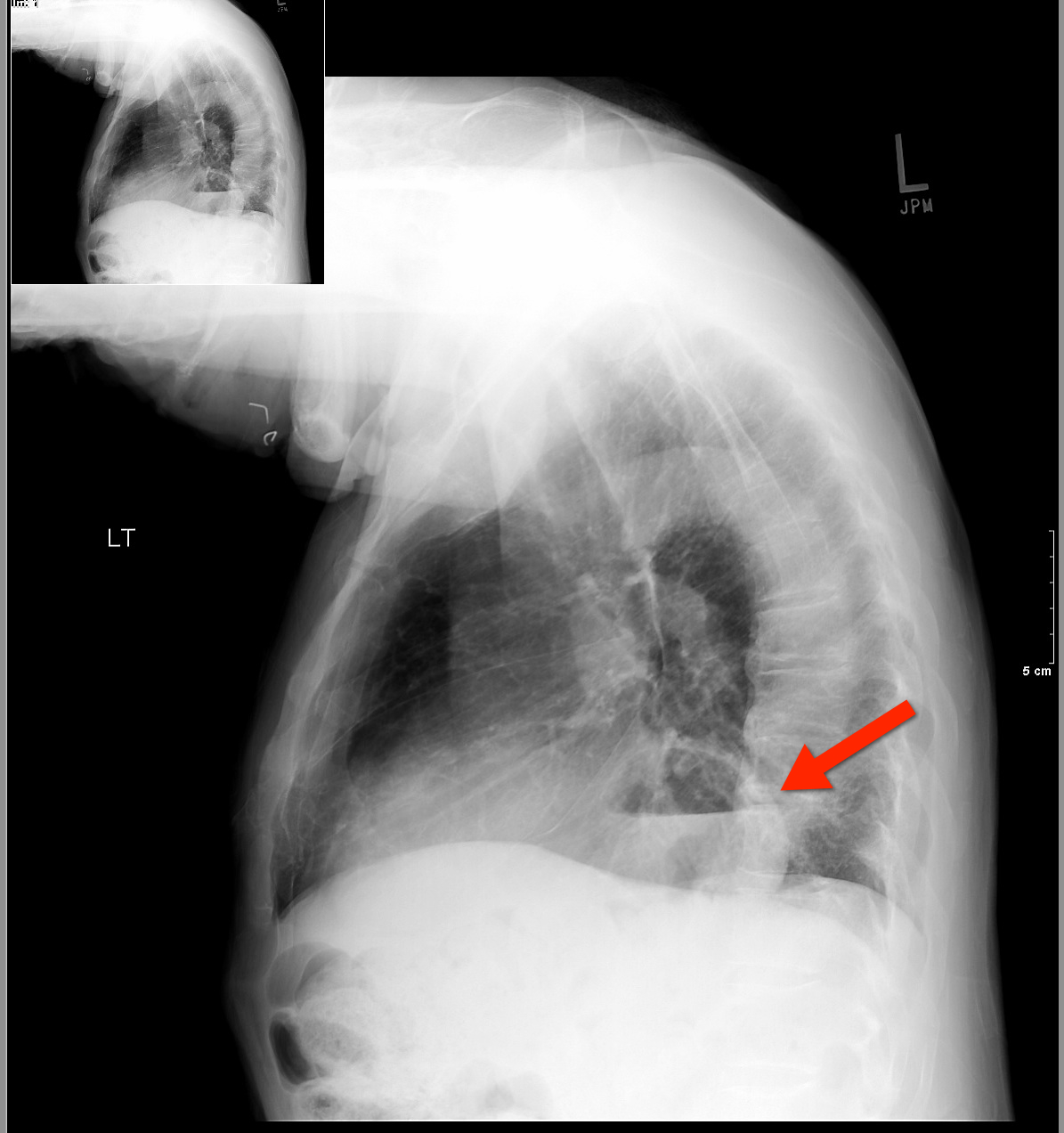
The differential diagnosis for circumscribed air-fluid levels on chest X-ray includes:
Bonus Pearl
Do you like listening to pre-recorded lectures, especially when they’re free? Then check out Free Emergency Medicine Talks (http://freeemergencytalks.net) where you can listen to millions (ok, more like 1,384) of free lectures recorded at major conferences around the world.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: coronary artery disease, acute coronary syndromes, stress test (PubMed Search)
Posted: 4/15/2012 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
(from Dr. Semhar Tewelde)
Stress testing is one modality used to screen for CAD. The goal is to identify a fixed obstruction to coronary blood flow (typically plaque > 50%) such as in stable angina. However, in ACS, both USA and AMI, the underlying pathophysiology is plaque rupture (typically plaque < 50%) and thrombus formation that may not have been significant enough to cause a positive stress test.
The use of a prior negative stress test to determine the disposition of ED chest pain patients is questionable. The history of present illness should dictate patient disposition. In one study 20.7% of patients presenting to the ED with a negative stress test within three years of presentation still had significant CAD defined as a positive cardiac markers, subsequent positive stress test of any type, cardiac catheterization requiring intervention, or death due to medical cardiac arrest within 30 days of ED presentation.
Walker J, Galuska M, Vega D. Coronary Disease in Emergency Department Chest Pain Patients With Recent Negative Stress Test. Western Journal of Emergency Medicine. September 2010; Volume XI, Num. 4
Category: Airway Management
Keywords: Compartment syndrome, leg pain (PubMed Search)
Posted: 4/14/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Chronic exertional compartment syndrome (CECS)
An overuse injury common in young endurance athletes
In athletes with lower leg pain, CECS was found to be the cause in 13.9% - 33%.
*This is likely under diagnosed as most recreation athletes will discontinue or modify their activity level at early symptom onset
Common in runners and most often involves the anterior compartment
Occurs due to increased pressure within the fascial compartments, primarily in the lower leg
Symptoms are bilateral 85 - 95% of the time
Exercise increases blood flow to leg muscles which expand against tight surrounding noncompliant fascia. This, in turn, increases compartment pressures and eventually reduces blood flow which leads to ischemic pain. Pain usually begins within minutes of starting exercise and experienced athletes can often pinpoint the time/distance required for symptom onset.
Symptoms are primarily pain (tightness, cramping, squeezing) but may also include paresthesias and numbness. Symptoms gradually abate with cessation of activity.
Diagnosis: Although some physicians’ make a clinical diagnosis based on Hx and exam, definitive diagnosis requires measurement of compartment pressures both at rest and post exercise.
Nonsurgical treatment: activity modification and rest
Surgical treatment: >80% success with anterior and lateral compartments vs. 50% with deep posterior compartment.
Category: Pediatrics
Posted: 4/13/2012 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
AAP Prep Curriculum
Category: Toxicology
Keywords: Opioid, breastfeeding, breast milk, newborn, infant (PubMed Search)
Posted: 4/5/2012 by Bryan Hayes, PharmD
(Updated: 4/12/2012)
Click here to contact Bryan Hayes, PharmD
Over the last few decades, the rate of breastfeeding has increased steadily in the developed countries of the world. During this time, opioid use in the general population has steadily increased as well. Despite this, clinicians remain unclear whether opioid use is safe during breastfeeding.

Hendrickson RG, McKeown NJ. Is maternal opiod use hazardous to breast-fed infants? Clin Toxicol. 2012;59(1):1-14.
Follow me on Twitter (@pharmacytoxguy)
