Category: Toxicology
Keywords: valproic acid, carnitine (PubMed Search)
Posted: 8/23/2012 by Fermin Barrueto
(Updated: 2/9/2026)
Click here to contact Fermin Barrueto
Patients that experience altered mental status (specifically lethargy) and are on valproic acid - check a serum ammonia level regardless if it is an overdose or just therapeutically on VPA.
If the ammonia is elevated in combination with the mental status change consider administration of L-carnitine either po or IV. It will lower the ammonia and improve the mental status within hours.
High risk patients for hyperammonia who therapeutically take VPA are certain pediatric patients that experience malnutrition, have seizure disorder and are on multiple seizure medications.
Department of Emergency Medicine, Erasme University Hospital, Universite Libre de Bruxelles, Brussels, Belgium. plheureu@ulb.ac.be
Category: Critical Care
Posted: 8/21/2012 by Mike Winters, MBA, MD
(Updated: 2/9/2026)
Click here to contact Mike Winters, MBA, MD
AKI and Fluid Balance
Bellomo R, et al. An observational study fluid balance and patient outcomes in the Randomized Evaluation of Normal vs. Augmented Level of Replacement Therapy trial. Crit Care Med 2012; 40:1753-60.
Category: Visual Diagnosis
Posted: 8/20/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
36 year-old female presents with left knee-pain following a motor vehicle crash (XRs are shown). What's the diagnosis AND what is the first test that should be performed to assess for vascular injury?
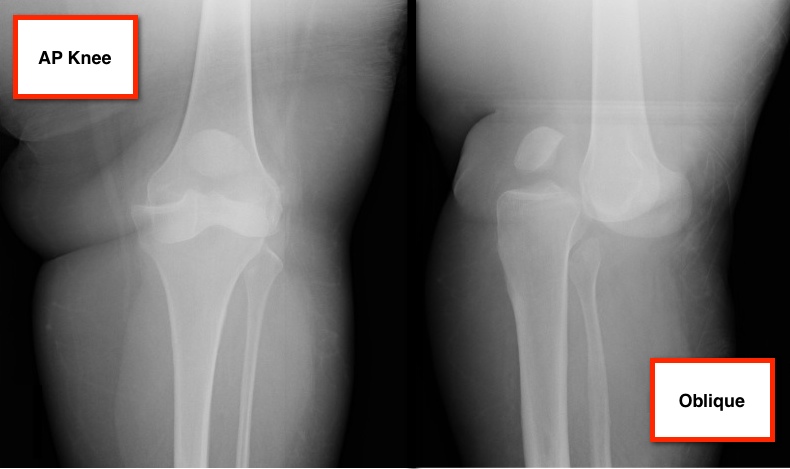
Answer: Anterior knee-dislocation and Ankle-Brachial Index (ABI)
Both anterior and posterior knee-dislocations have the potential for popliteal arterial injury.
ABI compares Doppler pressures of arms to legs to screen for lower limb ischemia (click here to learn more ABIs). ABIs can be used to accurately predict whether patients with knee dislocations have sustained vascular injury.
A prospective study by Mills et al. demonstrated the sensitivity, specificity, and positive predictive values of an ABI lower than 0.90 were 100% for arterial injury, requiring surgical treatment.
Conversely, the negative predictive value of an ABI that was 0.90 or higher was 100%, suggesting no further workup is required.
Mills W, Barei D, McNair P. The Value of the Ankle-Brachial Index for Diagnosing Arterial Injury After Knee Dislocation: A Prospective Study. Journal of Trauma-Injury Infection & Critical Care: June 2004 - Volume 56 - Issue 6 - pp 1261-1265.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Cardiology
Keywords: T wave inversions, negative T waves, ACS, PE (PubMed Search)
Posted: 8/19/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Pulmonary P waves (S1Q3T3 pattern + clockwise rotation) are specific for PE, but not sensitive.
This study examines if an ECG can discriminate between ACS vs. PE
- 40 patients with PE & 87 patients with ACS
- All had negative T waves in the precordial leads (V1-V4) on the admission ECG
The PE group had negative T waves commonly present in leads II, III, aVF, V1, V2, but less frequent in leads I, aVL, and V5 to V6 (p <0.05).
The ACS group had negative T waves in leads III and V1 in 1% compared with 88% of patients with PE (p <0.001).
Sensitivity, specificity, positive predictive value, and negative predictive value for Dx of PE were 88%, 99%, 97%, and 95%, respectively.
Negative T waves in both leads III and V1 may suggest PE can be differentiated from ACS in patients with negative T waves in the precordial leads.
Kosuge M, Kimura K, et al. Electrocardiographic differentiation between acute pulmonary embolism and acute coronary syndromes on the basis of negative T waves. Am J Cardiol. 2007 Mar 15;99(6):817-21.
Category: Orthopedics
Keywords: lactate, synovial fluid, (PubMed Search)
Posted: 8/18/2012 by Michael Bond, MD
(Updated: 2/9/2026)
Click here to contact Michael Bond, MD
The Analysis of Synovial Fluid Analysis
When trying to diagnosis a septic joint, it is common to order the following labs on the synovial fluid:
Unfortunately, there is no value of glucose or protein that has enough sensitivity and specificity to make the tests diagnostically helpful. Gram stains are only postive in culture positive septic joints in approximately 50% of the cases. Cultures take too long to be helpful in the ED. The synovial WBC count can be helpful if very high, but a low value does not ensure that the patient does not have a septic joint.
The one test that has been shown to have a Positive Likelihood ratio of Infinity is a synovial lactate level >10. A synovial lactate should be sent on all synovial fluid as a level of 10 and greater makes the diagnosis of septic arthritis, regardless of the gram stain or synovial WBC level.
Carpenter CR, Schuur JD, Everett WW, Pines JM. Evidence-based diagnostics: adult septic arthritis. Acad Emerg Med. 2011 Aug;18(8):781-96.
Category: Pediatrics
Keywords: vaccination, whooping cough (PubMed Search)
Posted: 8/17/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
If you have a patient who meets (or has had close exposure to someone meeting) the clinical case definition of pertussis (a cough lasting at least 2 weeks with one of the following: paroxysms of coughing, inspiratory “whoop,” or post-tussive vomiting) here are some important points to keep in mind:
Vaccination
Testing
Treatment
References:
Altunaiji SM, Kukuruzovic RH, Curtis NC, Massie J. Antibiotics for whooping cough (pertussis). Cochrane Database of Systematic Reviews 2007, Issue 3. Art. No.: CD004404. DOI: 10.1002/14651858.CD004404.pub3
http://www.cdc.gov/vaccines/pubs/surv-manual/chpt10-pertussis.html
Category: Critical Care
Posted: 8/14/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Femoral venous access is typically limited to the acute resuscitation of critically-ill patients. Several practice-guidelines recommend avoiding the femoral site, or removal once admitted to the ICU, because of the risk of catheter-related bloodstream infection (CRBI) and deep-vein thrombosis (DVT).
A recent systematic review and meta-analysis (including two randomized-control trials and eight cohort-studies) evaluated the risk of CRBI and DVT for catheters placed in either the internal jugular, subclavian, or femoral-venous sites. No difference in the rate of CRBI or DVT was found between the three sites, although the DVT data was less robust (i.e., contained heterogeneous data).
The authors hypothesized that improvements in sterility during central-line placement (e.g., full-barrier precautions), improved nursing care (e.g., central-line site care), and ultrasound guidance may have led to a reduction in femoral site complications.
Although a prospective randomized-control trial is necessary to confirm these results, this meta-analysis challenges the traditional teaching that femoral central-access should be avoided.
Marik, P. et al. The risk of catheter-related bloodstream infection with femoral venous catheters as compared to subclavian and internal jugular venous catheters: A systematic review of the literature and meta-analysis Crit Care Med. 2012 Aug;40(8):2479-85.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/13/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Placement of central-lines through the subclavian (SC) route has several advantages over other sites of venous cannulation:
• Lower rates of infection
• Lower rates of deep vein thrombosis
Placing a central-line through the "blind" SC approach increases the risk of non-compressible vessel injury and pneumothorax as compared to other approaches (e.g. internal jugular).
Ultrasound can help place central-lines in the SC vein while reducing the risk of complications; this video demonstrates the technique: http://ultrarounds.com/Ultrarounds/Subclavian_Ultrasound.html
Fragou, M. et al. Real-time ultrasound-guided subclavian vein cannulation versus the landmark method in critical care patients: a prospective randomized study. Crit Care Med. 2011 Jul;39(7):1607-12.
Category: Cardiology
Keywords: hypertrophic cardiomyopathy (PubMed Search)
Posted: 8/12/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Hypertrophic cardiomyopathy (HCM) is characterized by left ventricular hypertrophy (typically asymmetric) that occurs in the absence of pressure overload or storage/infiltrative disease.
HCM demonstrates remarkable diversity in disease course, age of onset, pattern and extent of LVH, degree of obstruction, and risk for sudden cardiac death.
Patients with HCM are at increased risk for sudden death, annual rate of SCD is ~1%. ICDs are recommended for all patients with prior arrest/sustained ventricular tachycardia (class I recommendation).
Category: Misc
Keywords: jet lag, sleep, athletic performance (PubMed Search)
Posted: 8/11/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Apologies for the long pearl, I did not want to split this into 3 parts)
Disruptions in sleep and circadian rhythms (from travel across time zones and jet lag) are known to alter cognitive functions. Mood and complex mental performance tasks deteriorate faster than do simpler mental performance tasks.
An athlete’s circadian rhythms are believed to be optimal for performance in the early evening (reaction time to light and sound in the fastest). Interestingly, the evening is the time of day when most world records have been broken. However, activities that require fine motor control and accuracy (hand steadiness and balance) are best in the morning.
In the normal population, travel effects are seen in inattention and an increase in errors and injuries in the workplace.
Athletes who perform in international competitions immediately after time zone transitions demonstrate a decline in performance involving complex mental activities, with an associated feeling of lethargy and a general loss of motivation.
British Olympic athletes demonstrated a decrease in leg and back strength in addition to reaction time when traveling westward across 4 time zones. In the NFL, west coast teams consistently beat east coast teams in evening games.
Of course, this type of outcome data is multifactorial and travel effects likely are only one of many complex factors.
Treatment:
Full adaptation to the new time zone is NOT recommended for short trips (1 – 2 days), only for longer stays (> 3 days).
Nonpharmacologic:
Preadaptation and bright light therapy: Remember that exposure to light is the primary cue for circadian rhythms. Bright light exposure in the mornings (after eastward travel) will advance the body clock, while exposure in the evenings (after westward travel) will delay it (Level B).
Shifting the sleep schedule 1 - 2 hours towards the destination time zone in the days preceding departure may shorten the duration of jet lag (Level B).
Strategic napping: Napping in the new time zone during typical sleep times in the destination time zone will delay adaptation. Power naps (20 minutes) may be helpful in decreasing daytime sleepiness in those with jet lag (Level B). The best time to nap (in flight or post flight) is nighttime in the destination time zone (Level B).
Pharmacologic:
Melatonin: Cochrane review concludes that it is safe and effective in both treating and preventing jet lag. It is recommended for adults traveling across 5 or more times zones; and may be effective for travel across 2 to 4 time zones. Take melatonin in the morning when traveling westward, and at the local bedtime when traveling eastward (Level B). Doses of 0.5 to 5mg were similarly effective. Melatonin taken in the evening and at higher doses are effective at inducing sleep (Level A).
Sleep aids: Hypnotic sleep aids reliably induce insomnia secondary to jet lag. Benzodiazepines improve sleep quality but may cause a “hangover” effect the next day, possibly impairing performance.
Ambien (zolpidem) and Lunesta (zopiclone) can be effective while limiting the hangover effect especially in those who have previosly tolerated the medication (Level A). Zolpidem may be more effective than melatonin and placebo at countering jet lag symptoms. Note: the use of both medicines together was not more effective than zolpidem alone but did cause daytime somnolence.
Stimulants: Care should be used in the athlete as most of these medications are banned in competition. There is a potential off label use for Provigil (modafinil) for improving daytime sleepiness associated with jet lag (currently approved for narcolepsy).
Caffeine, while not banned for the World Anti-Doping Agency, is a monitored substance. It increases daytime alertness and may accelerate entrainment in new time zones when consumed in the morning (later ingestion may interfere with sleep induction) (Level A).
Aaron Lee and Juan Carlos Galvez. Jet lag in athletes.Sports Health. 2012,211 - 216.
Category: Pediatrics
Posted: 8/10/2012 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
Category: Toxicology
Keywords: acetaminophen, Rumack-Matthew nomogram, diphenhydramine, opioid (PubMed Search)
Posted: 8/8/2012 by Bryan Hayes, PharmD
(Updated: 8/9/2012)
Click here to contact Bryan Hayes, PharmD
There is a growing recognition of patients who have a subtoxic acetaminophen level at the 4-hour mark, but then still go on to have a toxic level later.
This is concerning in that we usually can exclude the chance for toxicity if the 4-hour, post-ingestion level is < 150 mcg/mL following an acute ingestion (plotted on Rumack-Matthew nomogram).
It still is not clear exactly what subset of patients need to have a second level drawn, but a recurring theme seems to be ingestion of acetaminophen in combination with agents that slow GI motility, such as diphenhydramine or opioids. It may be worth ordering a second APAP level (possibly at 8 hours) in patients ingesting these prodcuts.
Dougherty PP, Klein-Schwartz W. Unexpected late rise in plasma acetaminophen concentrations with change in risk stratification in acute acetaminophen overdoses. J Emerg Med 2012;43:58-63.
Category: Critical Care
Posted: 8/7/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Lung Protective Ventilator Settings Still Underutilized
Needham DM, et al. Lung protective mechanical ventilation and two-year survival in patients with acute lung injury: A prospective cohort study. BMJ 2012;344:e2124.
Category: Visual Diagnosis
Posted: 8/5/2012 by Haney Mallemat, MD
(Updated: 8/6/2012)
Click here to contact Haney Mallemat, MD

Answer: Mandibular dislocation...and the Gromis method?
• The Gromis method (a.k.a. the "Masseteric Massage" technique) is an alternative method for reducing mandibular dislocations.
• Firm, direct, and constant pressure is applied bilaterally to the masseter muscles, which relaxes the muscles (i.e., reduces spasm) and allows mandibular reduction with less traction than traditional reduction techniques and with no procedural sedation.
• Rob Orman (@emergencypdx) posts a video of Dr. Daniel Gromis demonstrating the technique: http://vimeo.com/46453741
• Finally, UMEM pearl regulars may recognize this Xray from a post last year where we described another alternative method to reduce mandibular dislocations. Here it is again: http://www.youtube.com/watch?v=Kp8AzHIC0hM
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Cardiology
Keywords: takotsubo cardiomyopathy, stress cardiomyopathy, broken-heart syndrome (PubMed Search)
Posted: 8/5/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Takotsubo cardiomyopathy a.k.a. stress cardiomyopathy is an acute reversible disorder characterized by left ventricular (LV) dysfunction most commonly affecting postmenopausal women
The LV adopts the shape of an octopus trap (“takotsubo”) describing the narrow neck and broad base globular form during systole
Symptoms include precordial chest pain, dyspnea, or heart failure presenting with pulmonary edema mimicking ACS
Mayo Clinic Diagnostic Criteria
- Suspicion of AMI based on symptoms and STEMI on ECG
- Transient hypokinesia or akinesia of the middle and apical regions of LV
- Functional hyperkinesia of the basal region of LV
- Normal coronary arteries (luminal narrowing <50%)
- Absence of recent head injury, ICH, HCOM, myocarditis, or pheochromocytoma
Treatment is symptomatic and determined based on complications during the acute phase; occasionally requiring IABP or ECMO
Prognosis is better than those with ACS, however initial LVEF is similar to those seen with ischemic heart disease
Castillo Rivera AM, Ruiz-Bailen M, Rucabado Aguilar L. Takotsubo Cardiomyopathy – a clinical review. Medical Science Monitor. 17 (6): RA 135-47, 2011 Jun.
Category: Pharmacology & Therapeutics
Keywords: vasopressor, cardiac arrest, epinephrine, vasopression (PubMed Search)
Posted: 7/30/2012 by Bryan Hayes, PharmD
(Updated: 8/4/2012)
Click here to contact Bryan Hayes, PharmD
A recent paper reviewed 53 articles to assess the utility of vasopressors in cardiac arrest. The authors aimed to determine if vasopressors improved ouctomes in this patient population. Here are their conclusions:
Although these conclusions don't support the use of vasopressors in cardiac arrest, we should not abandon these therapies. Most of the trials were completed before wide-spread recognition of the post-cardiac arrest syndrome, implementation of therapeutic hypothermia protocols, and early cardiac catheterization.
Larabee TM, Liu KY, Campbell JA, et al. Vasopressors in cardiac arrest: a systematic review. Resuscitation. 2012;83(8):932-9.
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Posted: 8/3/2012 by Lauren Rice, MD
(Updated: 2/9/2026)
Click here to contact Lauren Rice, MD
Henoch-Schonlein Purpura (aka. Anaphylactoid purpura) is a small vessel vasculitis.
Background:
Clinical Features:
Etiology:
Diagnosis:
Treatment:
Category: Pharmacology & Therapeutics
Keywords: Uti,bactrim,smx/tmp,ciprofloxacin,levofloxacin (PubMed Search)
Posted: 8/2/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Acute, uncomplicated cystitis (in the non-pregnant female):
· The drug of choice is SMX/TMP (provided the resistance rate is <20%) X 3 days.
· An alternative is nitrofurantoin X 5 days.
Acute, uncomplicated pyleonephritis (in the non-pregnanct female) may be treated with:
· Levofloxacin X 5 days, or ciprofloxacin X 7 days (provided resistance rate is <10%).
· Alternatively, SMX/TMP may be used X 14 days.
The Medical Letter. July 23, 2012. Vol 54(1395):57-60.
Category: Critical Care
Posted: 7/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Crystalloids (i.e., 0.9% saline and lactated ringers) have been used during resuscitation for more than a century. Their invention, however, was more accidental than intentional.
Crystalloids were first used during the European Cholera epidemic of 1831. Hartog Hamburger later modified this solution in 1896 to the solution we know today as "normal" saline. Hamburger's solution was only intended for in vitro study of RBC lysis and was never intended for clinical use.
Around this time, Sydney Ringer was testing several fluids to use for physiologic studies. Ringer's lab assistant was erroneously substituting tap water for distilled water when preparing these solutions. Ringer later discovered that this tap water contained minerals making the solution "physiologic", isotonic, and safe for human use; Alexis Hartmann later added sodium lactate to create Ringer's Lactate.
Since the invention of crystalloids, many types of resuscitation fluids have been created and studied (i.e., albumins, gelatins, and starches); all have been shown to be more expensive, with no more benefit, and with possibly more harm when compared to crystalloids.
The "perfect" resuscitation fluid still alludes us today, but of all of the solutions marketed crystalloids are arguably the best...despite their accidental history.
Awad, S. et al. The history of 0.9% saline. Clinical Nutrition 2008 Apr;27(2):179-88.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 7/30/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old male was struck by a car while crossing the street. Chest X-ray and CT Chest with 3D reconstruction are shown below. What's the diagnosis?


Answer: Aortic dissection / transection
Blunt Aortic Injury

Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
