Category: Critical Care
Posted: 11/20/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A low-tidal volume (or protective) strategy of mechanical ventilation (i.e., tidal volume of 6-8cc/kg of ideal body weight) has previously been demonstrated to be beneficial in patients with acute respiratory distress syndrome (ARDS).
A meta-analysis was recently performed to determine whether this strategy of mechanical ventilation is also beneficial for patients without lung injury prior to initiation of mechanical ventilation.
Dr. Neto, et al. performed a meta-analysis of 20 studies (total of 2,822 mechanically ventilated patients) comparing a conventional ventilation strategy (average tidal volume was 10.6 cc/kg) to a protective ventilation strategy (average tidal volume was 6.4 cc/kg) of mechanical ventilation.
The authors concluded that patients ventilated with a protective lung-strategy had reductions in:
Bottom-line: This meta-analysis supports the notion that a strategy of low-tidal volume ventilation may have benefits for patients without ARDS, however prospective studies are needed.
Neto, S. et al. Association between use of lung-protective ventilation with lower tidal volumes and clinical outcomes among patients without acute respiratory distress syndrome. JAMA, Oct. 24/31; 308;16.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/19/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Do you like placing ultrasound-guided IV catheters? Check out this trick for covering the probe during the procedure.
http://ultrarounds.com/Ultrarounds/The_Vascular_Probe_Protector.html
or
https://www.youtube.com/watch?v=ZuOq6Ea_FbA&feature=plcp
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Torsades de pointes, prolonged QT syndrome (PubMed Search)
Posted: 11/18/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Congenital and Acquired Long QT Syndrome.Cardiology in Review. 12(4):222-34, 2004 Jul-Aug.
Category: Orthopedics
Keywords: tarsal tunnel syndrome (PubMed Search)
Posted: 11/17/2012 by Michael Bond, MD
(Updated: 2/7/2026)
Click here to contact Michael Bond, MD
Tarsal Tunnel Syndrome (TTS)
Prior pearls have addressed Carpal Tunnel Syndrome and Cubital Tunnel Syndrome, which affect the median and ulnar nerves, respectively. Tarsal tunnel syndrome, is a similar compression neuropathy of the tibial nerve as it transverses through the tarsal tunnel of the foot.
The tarsal tunnel is located behind the medial malleolus, and is where the posterior tibial artery, tibial nerve and several tendons transverse. Patients will present complaining of numbness of the foot radiating into Digits 1-4, pain, burning , and tingling of the base of the foot and heel. TTS has many causes and is more common in athletes.
Consider the diagnosis in patients with foot pain and numbness. If interested in more information about TTS please consider reading this eMedicine article, http://emedicine.medscape.com/article/1236852-overview
Category: Pediatrics
Keywords: meningitis, neck pain, retropharyngeal abscess (PubMed Search)
Posted: 11/16/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
A 1 year old gets sent from their pediatrician’s office for rule out meningitis. They presented with fever for 2 days and neck rigidity. Your LP results are normal. What additional test should you consider?
Answer:
Lateral neck x-ray
http://www.hawaii.edu/medicine/pediatrics/pemxray/v2c20.html

Retropharyngeal abscess (RPA) can commonly present like meningitis. Have a high suspicion in
children who are too young to complain of sore throat or difficulty swallowing.
A recent article in Pediatric Infectious Disease Journal detailed the rising incidence of retropharyngeal abscess, especially in younger patients, which is attributed to community acquired MRSA.
From 2004-2010 there was a 2.8 fold increase in RPA from the previous study period (1993-2003).
Children whose abscess grew MRSA were younger (mean 11 months) than the others (mean 62 months) (P < 0.001) and required longer duration of hospitalization (mean 8.8 days) than the rest (mean 4.5 days) (P = 0.002).
Bottom line: Consider a plain film in the child you are preparing to LP for meningitis.
Reference:
Abdel-Haq, N, Quezada M, Asmar BI. Retropharyngeal abscess in children: the rising incidence
of methicillin-resistant Staphylococcus aureus. Pediatr Infect Dis J 2012; 31: 696–699
Category: International EM
Posted: 11/14/2012 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
· Explosions can cause a complex series of injuries, which may include subtle or delayed findings. Repeated evaluations, such as serial abdominal exams, may be required.
· Blast injuries are divided into 4 categories:
o Primary blast injuries: Injury from blast wave over-pressure. Found in gas filled structures (ear, lung, hollow organs)
o Secondary blast injuries: Injury from thrown objects (primarily penetrating trauma, but may blunt)
o Tertiary blast injuries: Injuries from patient being thrown by blast wave (blunt trauma)
o Miscellaneous (quaternary) blast injuries: Injuries from other causes, such as burns, crush injuries, rhabdomyolysis, and toxic chemicals.
· The most common primary blast injury is tympanic membrane rupture.
University of Maryland Section for Global Emergency Health
Author: Jon Mark Hirshon
Category: Critical Care
Posted: 11/13/2012 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Burn Patients and Antibiotic Dosing
Jamal JA, et al. Improving antibiotic dosing in special situations in the ICU: burns, renal replacement therapy and extracorporeal membrane oxygenation. Curr Opin Crit Care 2012; 18:460-71.
Category: Visual Diagnosis
Posted: 11/12/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
33 year-old male found unconscious by EMS and complains of right shoulder pain upon waking up in the ED. Diagnosis?
Answer: Posterior shoulder dislocation
Follow me on Twitter (@criticalcarenow) or Google+ (+Haney Mallemat)
Category: Cardiology
Posted: 11/11/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Bazett's Formula QTc = QT/RR1/2
Category: Cardiology
Keywords: Long QT Syndrome (PubMed Search)
Posted: 11/11/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Congenital and Acquired Long QT Syndrome.Cardiology in Review. 12(4):222-34, 2004 Jul-Aug
Category: Orthopedics
Keywords: calf tear, muscle tear (PubMed Search)
Posted: 11/10/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Injury is often caused by sudden dorsiflexion on a plantar flexed foot w/ the knee in extension or similarly sudden knee extension with the ankle in a dorsiflexed position.
Injury has a predilection for the poorly conditioned middle-aged athlete, with "thick calves" who are engaged in strenuous activity
Strains are treated with ice, analgesics, and compression (decreases hematoma size and facilitates healing)
Also, consider casting/splinting as dictated by injury severity, such as with a night splint or a CAM boot.
Severe strains and ruptures can be splinted in plantar flexion for 3 weeks.
Gallo et al. Common Leg injuries of long-distance runners:Anatomic and Biomechanical approach. Sports Health. 2012
Category: Toxicology
Keywords: PCP, phencyclidine, haloperidol (PubMed Search)
Posted: 11/7/2012 by Bryan Hayes, PharmD
(Updated: 11/8/2012)
Click here to contact Bryan Hayes, PharmD
Background
Patients who are intoxicated with, or emerging from, phencyclidine (PCP) highs present with acute agitation that can be challenging to treat
Risks of physical restraints for combative patients include injury, hyperthermia, rhabdomyolysis, and increased agitation or excited delirium
Haloperidol is an option for chemical restraint that is typically safe and rapid acting
Some concerns related to haloperidol use in PCP-intoxicated patients include worsened PCP-induced hyperthermia, dystonic or anticholinergic reactions, lower seizure threshold, and hypotension
Data
A recent retrospective case series assessed the frequency of adverse effects from the combination of PCP and haloperidol
Of 59 cases, only two patients experienced an adverse reaction, and neither could be conclusively linked to haloperidol administration
This analysis had several major limitations including retrospective design for identifying adverse reactions, potential for false positive PCP screens, and possible haloperidol administration more than 24 hours after PCP intoxication
Bottom Line
While haloperidol may be safe for agitated PCP-intoxicated patients, this paper adds nothing to refute or support its use. Benzodiazepines and calm environment are still first-line therapy.
It should be noted that no data exist showing poor outcomes in PCP-intoxicated patients administered haloperidol, which begs the question "Is there even an issue?" Dr. Leon Gussow, author of The Poison Review, provides a nice answer and summary of the article here.
MacNeal JJ, et al. Use of haloperidol in PCP-intoxicated individuals. Clin Toxicol 2012;50:851-3.
Gussow L. The Poison Review. http://www.thepoisonreview.com/2012/11/07/is-haloperidol-dangerous-in-pcp-associated-agitation-a-non-answer-to-a-non-problem/ Accessed Nov 8, 2012.
Category: International EM
Keywords: Hantavirus, Sin Nombre, Pulmonary, Infectious Disease (PubMed Search)
Posted: 11/7/2012 by Andrea Tenner, MD
(Updated: 11/16/2012)
Click here to contact Andrea Tenner, MD
University of Maryland Section for Global Emergency Health
Author: Andi Tenner
Center for Disease Control. (2012). Hantavirus. Retrieved September 3, 2012, from http://www.cdc.gov/hantavirus/index.html
Berger, S. A., Calisher, C. H., and Keystone, J. H., (2003). Exotic Viral Disease: A Global Guide. Hamilton, Ontario: BC Decker.
Category: Critical Care
Posted: 11/6/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Previous pearls have described the increasing evidence against colloid (e.g., hydroxyethyl starch) use during resuscitation. Now it appears that the crystalloid 0.9% normal saline (NS) may be under fire.
The use of large volumes of NS has been associated with hyperchloremic metabolic acidosis and harm in animal studies. The risk of harm in humans, however, has been less clear.
Bellomo et al. conducted a prospective observational study in which patients being resuscitated in the control group received NS at the clinicians' discretion; i.e., chloride-liberal strategy. The use of NS was restricted in the intervention group, where other less chloride containing fluids were used for resuscitation (e.g., Ringer's Lactate); i.e., a chloride-restrictive strategy.
The authors found that when compared to patients in the chloride-liberal group, the chloride-restrictive group had significantly less rise in baseline creatinine, less overall AKI, and a reduced need for renal replacement therapy.
Bottom line: Although this was only an observational study, the liberal use of normal saline during resuscitation may increase the risk of AKI and renal replacement therapy.
Bellomo, R. et al. Association between a chloride-liberal vs. chloride-restrictive intravenous fluid administration strategy and kidney injury in critically ill adults. JAMA. 2012 Oct 17;308(15):1566-72. doi: 10.1001/jama.2012.13356.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 11/5/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
11 year-old male is tackled and falls on his outstretched hand while playing football. X-rays are shown below. What's the diagnosis?
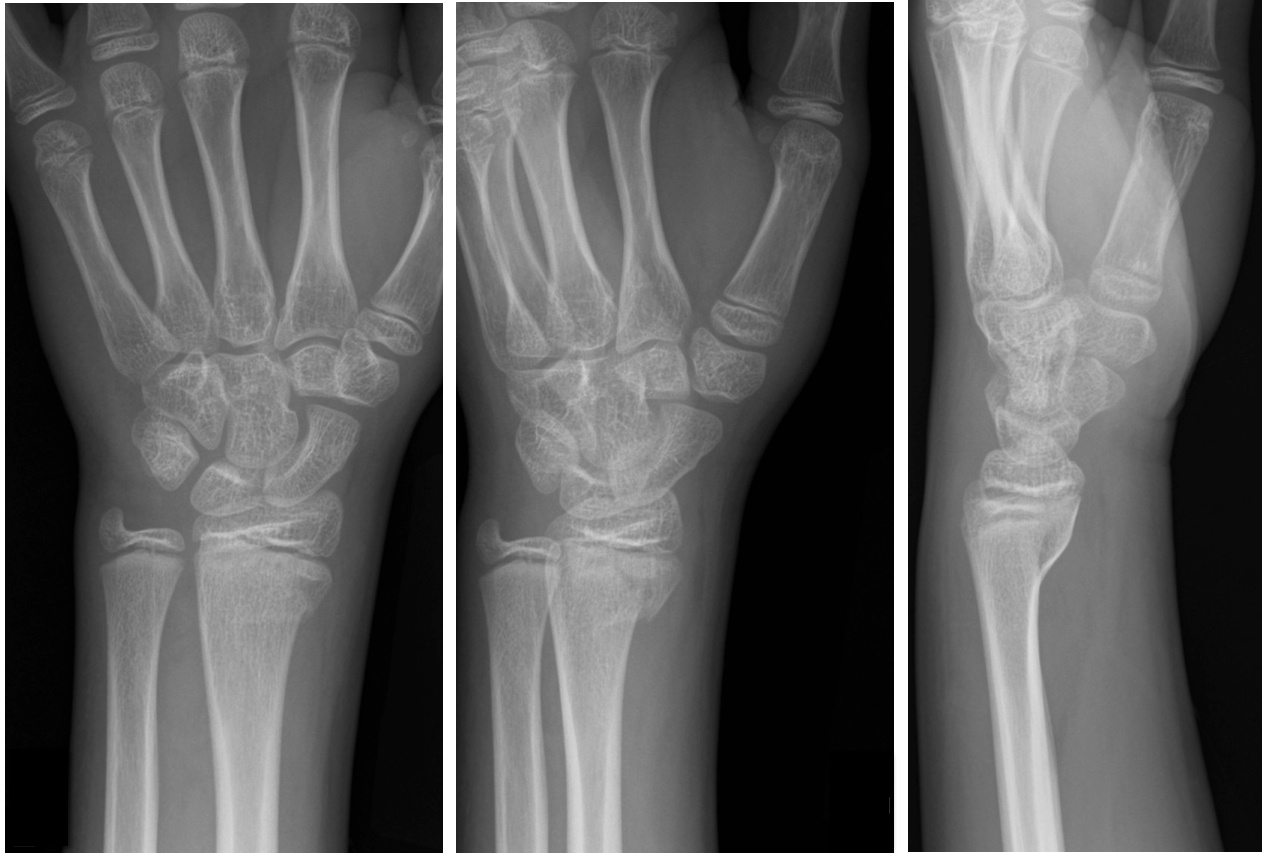
Answer: Salter-Harris Fracture - Type II
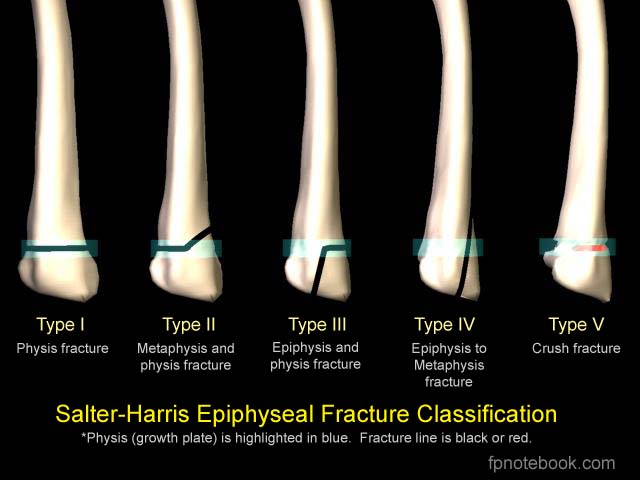
Salter-Harris Fracture (SHF)
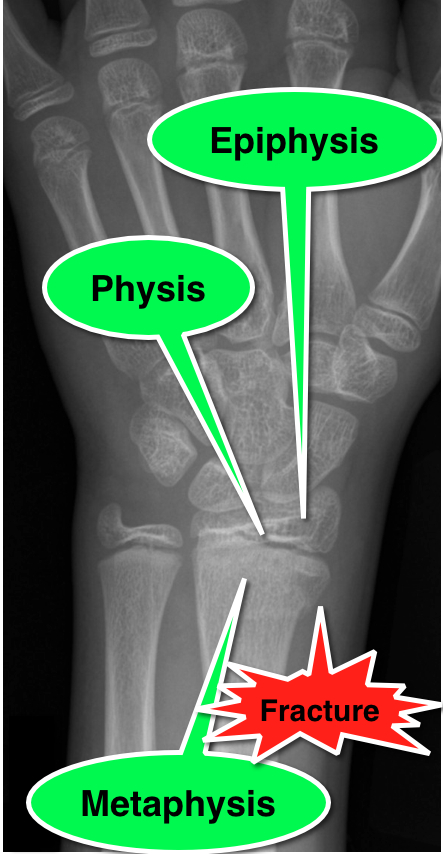
SHF are fractures through the growth plate (a.k.a. the physis), therefore are unique to pediatric patients.
Fractures are categorized according to involvement of the physis, metaphysis, and epiphysis. Proper injury classification is important because it affects both the treatment and potential long-term complications. Radiographic findings can sometimes be subtle; especially Type 1 SHF.
Occult SHF should be suspected when there is tenderness or swelling over an epiphyseal surface with X-rays negative for fracture. In this case, children should be splinted and urgently followed up.
SHF classification
Bonus Pearl:
Use mnemonic SALTR to remember fracture type (Type I-Slipped, II-Above physis, III-Lower physis, IV-Through physis, V-Rammed)
emedicine.medscape.com/article/412956-overview
Salter, R and Harris R. Injuries involving the Epiphyseal Plate. Journal of Bone and Joint Surgery. Vol 45-A. Issue 3, April 1963.
fpnotebook.com/_media/OrthoFractureSalterHarris.jpg
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: de Winter T wave, proximal LAD occlusion (PubMed Search)
Posted: 11/3/2012 by Semhar Tewelde, MD
(Updated: 11/4/2012)
Click here to contact Semhar Tewelde, MD
An ECG pattern that signifies occlusion of the proximal left anterior descending coronary artery (LAD) without ST-segment elevation
de Winter R, et al. A New ECG Sign of Proximal LAD Occlusion. NEJM Nov, 2008:359;19
Category: Pharmacology & Therapeutics
Keywords: penicillin, cross-reactivity, cephalosporin, IgE, allergy (PubMed Search)
Posted: 10/29/2012 by Bryan Hayes, PharmD
(Updated: 11/3/2012)
Click here to contact Bryan Hayes, PharmD
It seems we've finally put to bed the myth that 10% of penicillin-allergic patients will also react to cephalosporins. Dr. Campagna, et al. recently published a review article concluding that the true cross-reactivity is negligible except when side-chains are similar [PMID 21742459].
This topic was also the subject of a recent post on the Academic Life in EM blog (http://academiclifeinem.blogspot.com/2012/08/busting-myth-10-cephalosporin.html).
But what about the reverse question? Can I give a penicillin to a cephalosporin-allergic patient?
Dr. Romano's group tested 98 patients with skin-test postitive cepahlosprin allergy (mostly IgE -mediated anaphylaxis). Patients were then skin tested for penicillin allergy. Those testing negative were challenged with a penicillin.
25% of patients reacted to the penicillin
Similar side-chain was a strong predictor of cross-reactivity
A Letter to the Editor response to this study pointed out that the authors used a smaller-than-standard size threshold for a positive response to the penicllin AND used a higher-than-standard dose of amoxicillin for testing. In light of this, the rate of subjects with cephalosporin allergy who do not have a history of penicillin allergy but with true IgE-mediated allergy to penicillin might be much closer to 5%.
Bottom line: The cross-reactivity of penicillins in cephalosporin-allergic patients is somewhere between 5-25%.
Romano A, et al. IgE-mediated hypersensitivity to cephalosporings: cross-reactivity and tolerability of penicillins, monobactams, and carbapenems. J Allergy Clin Immunol 2010;126(5):994-9.
Macy E. Penicillin allergy might not be very common in subjects with cephalosporin allergy. J Allergy Clin Immunol 2011;127(6):1638-9.
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Posted: 11/2/2012 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Conventional pediatric nasal cannula can safely deliver up to 4 lpm but are limited by cooling and drying of the airway. This leads to decreased airway patency, nasal mucosal injury, bleeding and possibly increase in coagulase negative staph infections.
HFNC delivers flow up to 40 lpm with 95-100% relative humidity at a controlled temperature. In infants, the initial flow rate is set between 2-4 lpm and can be increased to 8 lpm. Older children and can be started at 10 lpm and increased as high as 40 lpm. Oxygen is also adjustable.
Studies have shown improved comfort, respiratory rate and oxygenation compared to nasal CPAP.
Noninvasive Ventilation Techniques in the Emergency Department: Applications in Pediatric Patients. Pediatric Emergency Medicine Practice. Vol 6 No 6. June 2009.
Spentzas et al. Children with Respiratory Distress Treated with High-Flow Nasal Cannula. Journal of Intensive Care Medicine. Vol 24 No 5. September/October 2009.
Category: Pharmacology & Therapeutics
Keywords: ACE inhibitors, angioedema, icatibant (PubMed Search)
Posted: 11/1/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Category: Pharmacology & Therapeutics
Keywords: ACE inhibitors, angioedema, icatibant (PubMed Search)
Posted: 11/1/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Wilerson G. Angioedema in the Emergency Department: An evidence-based review. Emergency Medicine Practice, Nov 2012.
