Category: Toxicology
Keywords: creatine, supplement, weight lifting (PubMed Search)
Posted: 1/3/2013 by Ellen Lemkin, MD, PharmD
(Updated: 2/7/2026)
Click here to contact Ellen Lemkin, MD, PharmD
Creatine
Adverse effects: weight gain, edema, GI cramping, fatigue and diarrhea
Dandoy C, Gereige RS. Performance-Enhancing Drugs. Pediatrics in Review June 2012;33(6):265-72.
Category: International EM
Keywords: Leptospirosis, Baltimore, jaundice, thrombocytopenia, international, tropical (PubMed Search)
Posted: 1/2/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
-Leptospirosis is a tropical infectious disease that is also endemic in the US. (Estimated 16% seroprevalence in inner city Baltimore!)
-The spirochete is spread through animal urine and can survive in water or soil for weeks.
-Risk factors: rural exposure to animal urine (farming, adventure sports) or urban exposure to rat urine.
-Infection is acquired through breaks in the skin or mucus membranes
-Outbreaks are often seen following rain or floods.
Clinical Presentation:
-Non-specific febrile illness (usually not diagnosed in these cases)
-If untreated, 5-10% progress to jaundice, renal failure, thrombocytopenia, hemorrhage, and respiratory failure.
Diagnosis:
- Primarily based on clinical presentation and history
- Paired serum sent to CDC (the acute serum sample should be drawn in the ED)
Treatment:
- Doxycycline, Ceftriaxone and Penicillin are all effective
Bottom Line:
Consider and treat for Leptospirosis in patients with possible exposure animal urine (especially after a flood) who present in extremis with renal failure, jaundice, and thrombocytopenia.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Center for Disease Control. (2012) Leptospirosis. Retrieved January 1, 2013 from http://www.cdc.gov/leptospirosis/infection/index.html.
Childs JE, Schwartz BS, Ksiazek TG, et al. Risk Factors Associated with Antibodies to Leptospires in Inner-city Residents of Baltimore: A Protective Role for Cats. Am J Public Health. 1992;82:597-599.
Leung J, Schiffer J. Feverish, Jaundiced. Am J Med. 2009;122:129-131.
Category: Critical Care
Posted: 1/1/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
DRESS (Drug Reaction with Eosinophilia and Systemic Symptoms) or DIHS (Drug-Induced Hypersensitivity Syndrome) is a potentially life-threatening adverse drug-reaction.
Incidence is 1/1,000 to 1/10,00 drug exposures. It occurs 2-6 weeks after the drug is first introduced, distinguishing it from other adverse drug-reactions which typically occur sooner.
The syndrome classically includes:
The most commonly implicated drugs are anticonvulsants (e.g., carbamazepine, phenobarbital, and phenytoin), sulfonamides, and allopurinol.
Recovery is typically complete after discontinuing the offending drug; systemic steroids may promote resolution of the illness.
Cacoub P. et al. The DRESS syndrome: a literature review. Am J Med 2011 Jul;124(7):588-97. http://www.ncbi.nlm.nih.gov/pubmed/21592453
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 12/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
31 year-old male with recently diagnosed hypertension presents with rapid lip swelling. He started taking an unknown medication for his hypertension last week. Further history reveals that he has had prior, although milder, episodes previously. Name two medications that may help treat him.

Answer: The patient has hereditary angioedema with an episode triggered by an ACE inhibitor. Treatment includes the usual cocktail of histamine blockers and steroids plus:
The precipitant cause is unknown in most cases, but common etiologies include drugs (e.g. ACE inhibitors), infections, dental work, or stress.
Serum C4 level may assist in the diagnosis, but are rarely helpful acutely.
Fifty percent of patients will have laryngeal swelling at one point in their lives and asphyxiation is the leading cause of death; mortality is ~14-33%
The airway must be emergently evaluated to determine the need for intubation. If required, the most skilled person should take the first look.
If access to the oropharynx is limited (secondary to lip and tongue swelling) fiberoptic nasolaryngoscopy may be considered however, always be prepared to perform an emergent surgical airway.
Bonus Pearl: Check out this months V-Cast hosted by Dr. Amal Mattu. Dr. Jim Roberts (of Roberts and Hedges fame) reviews angioedema. Check out this great review here: http://cmedownload.com/lecture/angioedema-v-cast
References
Joseph J. Moellman, and Jonathan A. Bernstein. Diagnosis and Management of Hereditary Angioedema: An Emergency Medicine Perspective. Journal of Emergency Medicine 2012 http://www.jem-journal.com/article/S0736-4679(11)01116-4/abstract
Follow me on Twitter (@criticalcarenow) or on Google+ (+criticalcarenow)
Category: Cardiology
Posted: 12/30/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Category: Orthopedics
Keywords: metacarpal, neck, fracture (PubMed Search)
Posted: 12/29/2012 by Michael Bond, MD
Click here to contact Michael Bond, MD
Metacarpal Neck Fractures (i.e.: Boxer’s Fracture if 5th Metacarpal)
Depending on the MCP joint involved a certain amount of angulation is permissible before it adversely affects normal function.
Wishing everybody a Happy and Healthy New Year.
Category: Pediatrics
Posted: 12/28/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: ketamine, pain (PubMed Search)
Posted: 12/27/2012 by Fermin Barrueto
(Updated: 2/7/2026)
Click here to contact Fermin Barrueto
Despite a paucity of data, pain management clinics are administering topical gel mixtures that have included ketamine, tricyclics, calcium channel blockers and baclofen. Internet blogs have already identified this gel mixture as a way to "get high". This is one of those google searches you have to do on your own.
1: Lynch ME, Clark AJ, Sawynok J, Sullivan MJ. Topical 2% amitriptyline and 1% ketamine in neuropathic pain syndromes: a randomized, double-blind, placebo-controlled trial. Anesthesiology. 2005 Jul;103(1):140-6. 2: Lynch ME, Clark AJ, Sawynok J. A pilot study examining topical amitriptyline, ketamine, and a combination of both in the treatment of neuropathic pain. Clin J Pain. 2003 Sep-Oct;19(5):323-8. 3: Uzaraga I, Gerbis B, Holwerda E, Gillis D, Wai E. Topical amitriptyline, ketamine, and lidocaine in neuropathic pain caused by radiation skin reaction: a pilot study. Support Care Cancer. 2012 Jul;20(7):1515-24.
Category: International EM
Posted: 12/25/2012 by Walid Hammad, MD, MBChB
(Updated: 2/7/2026)
Click here to contact Walid Hammad, MD, MBChB
Bottom Line: A mild increase in blood parasite count after initiation of treatment is not uncommon. Marked increases should indicated treatment failure and the treatment drug should be changed to another class.
University of Maryland Section for Global Emergency Health
Author: Emilie J.B. Calvello, MD, MPH
Wurts, N. Et al. Early treatment failure during treatment of Plasmodium falciparum malaria with atovaquone-proquanil in the Repulic of Ivory Coast. Malar J 2012 May; 2(11): 146.
Silachomroon, U. Et al. Frequency of Early Rising Parasitemia in Falciparum Malaria Treated with Artemisinin Derivatives. Southeast Asian J Trop Med Pub Health 2001 Mar; 32(1): 50 – 56.
Category: Critical Care
Posted: 12/25/2012 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
VV-ECMO for Refractory Hypoxemia
Combes A, et al. What is the niche for extracorporeal membrane oxygenation in severe acute respiratory distress syndrome? Curr Opin Crit Care 2012; 18:527-32.
Category: Visual Diagnosis
Posted: 12/24/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
52 year-old male with diabetes complains of severe left foot pain for one month and now inability to ambulate. Vital signs are normal and X-rays are shown below. What's the diagnosis and why should you get a biopsy early?

Answer: Osteomyelitis and a bone biopsy (with culture) should be obtained early and before starting antibiotics.
Osteomyelitis is inflammation of a bone secondary to an infecting organism.
Risk factors include:
Causative bacteria typically include S. Aureus, Pseudomonas, Salmonella (classically with Sickle cell)
Diagnosis
Early and long-term antibiotic treatment (4-6 weeks) is required, but should be done AFTER obtaining bone biopsy and culture; long-term antibiotics are the rule and the most narrow spectrum antibiotic should be determined.
Operative management is sometimes required; especially if secondary to infected prosthetics.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Posted: 12/23/2012 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
Armstrong E, MD, Kulkarni A, Hoffmayer K, et al. Am J Cardiol 2012;110: 345–349
Category: Orthopedics
Keywords: Exercise, NSAIDs, bowel injury (PubMed Search)
Posted: 12/22/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
NSAIDs are commonly used by professional and recreational athletes to both reduce existing and/or prevent anticipated exercise induced musculoskeletal pain
NSAIDs have potential hazardous effects on the gastrointestinal (GI) mucosa during strenuous physical exercise
Potential effects include mucosal ulceration, bleeding, perforation. and short-term loss of gut barrier function in otherwise healthy individuals
Intense exercise by itself has previously been shown to induce small intestine injury
Human intestinal fatty acid binding protein (1-FABP) is a protein found in mature small bowel enterocytes which diffuses into the circulation upon injury
Ibuprofen and endurance exercise (cycling) independently result in increased 1-FABP levels
When occurring together, ibuprofen ingestion with subsequent exercise causes significantly increased small bowel injury and intestinal permeability
Small bowel injury was found to be reversible in 2 hours
Taking empiric NSAIDs before endurance exercise may be an unhealthy practice and should be discouraged in the absence of a clear medical indication
Aggravation of exercise-induced intestinal injury by Ibuprofen in athletes. VAN Wijck K, Lenaerts K, VAN Bijnen AA, et al. Med Sci Sports Exerc. 2012 Dec;44(12):2257-62.
Category: Pediatrics
Posted: 12/15/2012 by Mimi Lu, MD
(Updated: 12/21/2012)
Click here to contact Mimi Lu, MD
Parents bring in their child who placed a bead, seed, or other object up her nose. What do you do? Who should you call?
Research suggests that a decades-old home remedy (of sorts) known as the “mother’s kiss” may do the trick for children 1-8 years of age. It’s also much less invasive or frightening than some of the tools and techniques used in emergency departments with a success rate approaching 60%
First described in 1965, here’s how the mother’s kiss technique works:
Category: Toxicology
Keywords: poinsettia (PubMed Search)
Posted: 12/20/2012 by Fermin Barrueto
(Updated: 2/7/2026)
Click here to contact Fermin Barrueto
Myth: The ornamental red plant - poinsettia - gained a reputation as a poisonous plant from a case report. In 1919, a 2-year-old child reportedly died from an ingestion and later an 8-month-old developed mucosal burns. These anectdotal case reports perpetuated the myth that poinsettia plants are poisonous. In the modern literature there is one single case of anaphylaxis(1) due to poinsettia ingestion/exposure, an allergic dermatitis(2) and one case of dermatitis(4).
Krenzelok et al.(3) showed there were 22,793 cases of poinsettia exposure and there were no fatalities reported to poison centers. 96.1% were kept at home without sequelae.
1: Kimata H. Anaphylaxis by poinsettia in infants with atopic eczema. Allergy. 2007 Jan;62(1):91-2. 2: Bala TM, Panda M. No poinsettia this Christmas. South Med J. 2006 Jul;99(7):772-3. 3: Krenzelok EP, Jacobsen TD, Aronis JM. Poinsettia exposures have good outcomes...just as we thought. Am J Emerg Med. 1996 Nov;14(7):671-4. 4: Edwards N. Local toxicity from a poinsettia plant: a case report. J Pediatr.1983 Mar;102(3):404-5.
Category: International EM
Keywords: trypanosomiasis, Human African Trypanosomiasis, sleeping sickness, international (PubMed Search)
Posted: 12/19/2012 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
· A parasitic disease transmitted by the bite of the 'Glossina' insect (tsetse fly.)
· The disease is most prevalent in rural areas of Africa. Untreated, it is usually fatal. Infection with the genus Trypanosoma brucei gambiense may lead to chronic asymptomatic illness.
· Travelers to endemic areas in Africa are risk becoming infected.
· Symptoms resemble a viral illness; headaches, fever, weakness, pain in the joints, and stiffness. The parasite is able to crosses the blood-brain barrier and causes neurological symptoms, mainly psychiatric disorders, seizures, coma and ultimately death.
· Diagnosis is by serological tests (Card Agglutination Trypanosomiasis Test or CATT). Confirmation of infection requires the performance of parasitological tests to demonstrate the presence of trypanosomes in the patient.
· Treatment: four drugs are registered for the treatment of HAT: pentamidine, suramin, melarsoprol and eflornithine.
World Health Organization. (2010). Working to overcome the global impact of neglected tropical diseases. First WHO report on neglected tropical diseases. Available: http://whqlibdoc.who.int/publications/2010/9789241564090_eng.pdf. Last accessed 12/17/2012
Category: Critical Care
Posted: 12/18/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Management of patients with severe traumatic brain injury (TBI) typically involves the use of invasive intra-parenchymal pressure monitors. Although use of these monitors is recommended by TBI management guidelines, good quality evidence of benefit is lacking.
A recently published study evaluated the outcomes of TBI patients using a management protocol incorporating either an intracranial pressure (ICP) monitor compared to use of the clinical exam PLUS serial neuroimaging; a total of 324 patients were prospectively randomized into either group.
The primary study outcome was a composite of survival, impaired consciousness, and functional status at both three and six months.
The results of the study did not show a significant difference in the:
Bottom line: This study suggests that clinical exam PLUS serial neuroimaging may perform as well as invasive intra-parenchymal monitors for guiding therapy in TBI patients.
Chestnut, R. et al. A Trial of Intracranial-Pressure Monitoring in Traumatic Brain Injury. NEJM 2012 Dec 12. http://www.ncbi.nlm.nih.gov/pubmed/23234472
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 12/17/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
50 year-old man with presents with acute-onset sharp left-sided chest pain and dyspnea. What's the diagnosis and the name of the abnormality on chest x-ray?
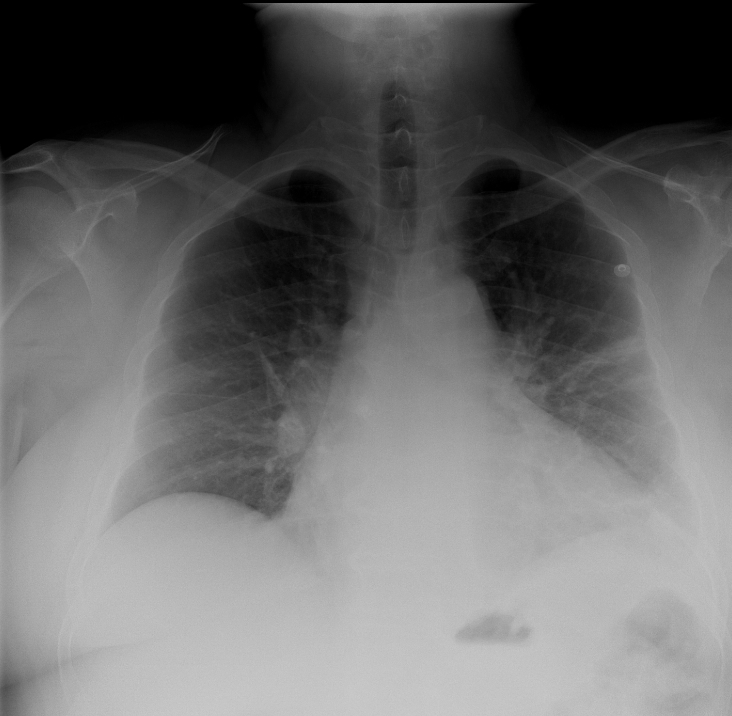
Answer: Pulmonary embolism with CXR demonstrating "Hampton Hump".
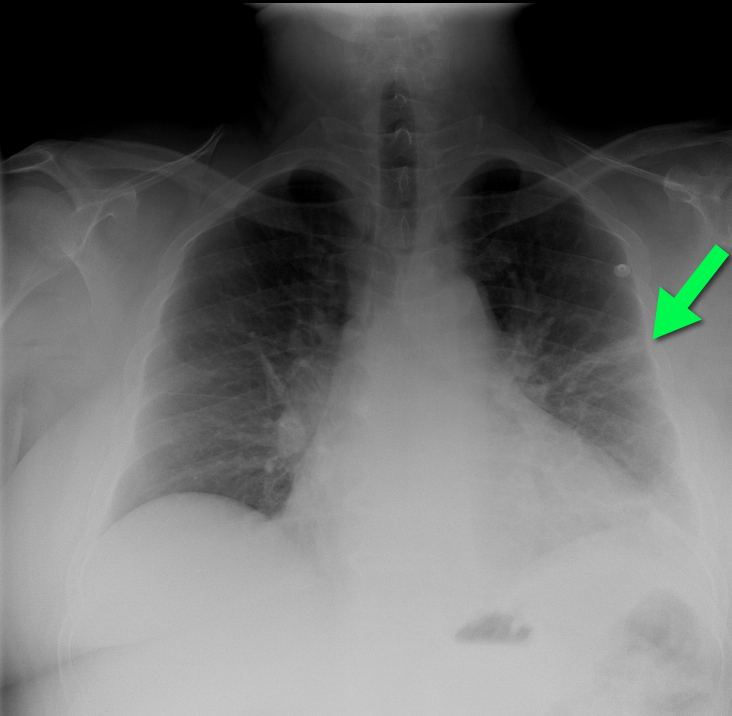
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: Pulmonary Arterial Hypertension (PAH) (PubMed Search)
Posted: 12/17/2012 by Semhar Tewelde, MD
(Updated: 2/7/2026)
Click here to contact Semhar Tewelde, MD
A. Yao. Journal of Cardiology 60 (2012) 344–349
Category: ENT
Keywords: epistaxis (PubMed Search)
Posted: 12/15/2012 by Michael Bond, MD
Click here to contact Michael Bond, MD
Epistaxis can be a difficult thing to control in the ED, but there are several techniques you can learn that will make your life easier.
The majority of epistaxis cases are from kiesselbach's plexus therefore you can control it with:
Direct Pressure: Can be held with two fingers pinching the nares, or you can tape 4 tongue blades together and make your own "clothes pin" that can then be used to pinch the nares.
Vasoconstrictor and Anesthesia: A 1:1 mixture of topical lidocaine 4% and oxymetazoline can often be mixed together in the same oxymetazoline spray container enabling you to just spray it into the nares. This will often slow or stop the bleeding and provides anesthesia in case you need to cauterize the bleeding site. Some IV/IM narcotic pain medication will also help increase patient cooperation.
Visualize the bleeding site: Use a HEAD LAMP with an appropriate sized nasal speculum. You may look like Marcus Welby, MD but nothing works as well to see into the nose.
Cauterization It is best to cauterize circumferential around the bleeding site prior to directly cauterizing the actual site. Be careful with electrical cautery so has not to perforate the septum.
Nasal Packing: Instead of using surgilube to lubricate the packing; use Muprion, Bactroban or Bacitracin ointment to lubricate the packing. This will reduce the chance of Toxic Shock Syndrome.
