Category: International EM
Posted: 5/22/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Clinical Presentation:
- A 40-year-old Hispanic man was admitted to the hospital after being found unconscious. He had a 2-day history of disorientation that manifested itself as his being unable to recognize family members.
- Upon admission he regained consciousness, becoming alert and oriented, but developed urinary retention and was unable to move or feel his lower extremities.
- Spinal MRI (with and without gadolinium) showed the spinal cord to be abnormally diffuse, with swelling and edema in the cervicothoracic region.
Diagnosis:
- After an extensive work up for lymphoma and CNS infection, he was discovered to have toxoplasmosis and was found to be HIV positive, which was previously undiagnosed.
Discussion:
- Approximately 10% of patients with AIDS present with some neurological deficit as their initial complaint, and up to 80% will have CNS involvement during the course of their disease.
- Myelitis is a known complication of AIDS and is occasionally the initial complaint.
The incidence of myelopathy may be as high as 20%, with 50% of the cases reported post-mortem
- Toxoplasmosis is the most common cause of cerebral mass lesions in patients with AIDS
Occurring in 3–10% of patients in the United States and in up to 50% of AIDS patients in Europe, Latin America, and Africa
Bottom Line:
New neurological deficit in any patient should raise suspicion of HIV infection
Most patients with AIDS that present with evolving myelopathy, characterized by extremity weakness, sensory involvement, spinal cord enlargement, enhancing lesions in brain or spinal cord CT or MRI, have toxoplasmic myelitis
University of Maryland Section of Global Emergency Health
Author: Terrence Mulligan DO, MPH
"Spinal cord toxoplasmosis as an unusual presentation of AIDS: case report and review of the literature", Int J Emerg Med (2010) 3:439–442
Category: Critical Care
Posted: 5/21/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The Macklin Effect
Pneumomediastinum (click here for image) may be caused by many things:
The "Macklin Effect" is typically a self-limiting condition leading to spontaneous pneumomediastinum and massive subcutaneous emphysema after the following:
Pneumomediastinum secondary to the Macklin effect frequently leads to an extensive workup to search for other causes of mediastinal air. Although, no consensus exists regarding the appropriate workup, the patient's history should guide the workup to avoid unnecessary imaging, needless dietary restriction, unjustified antibiotic administration, and prolonged hospitalization.
Treatment of spontaneous pneumomediastinum includes:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/20/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
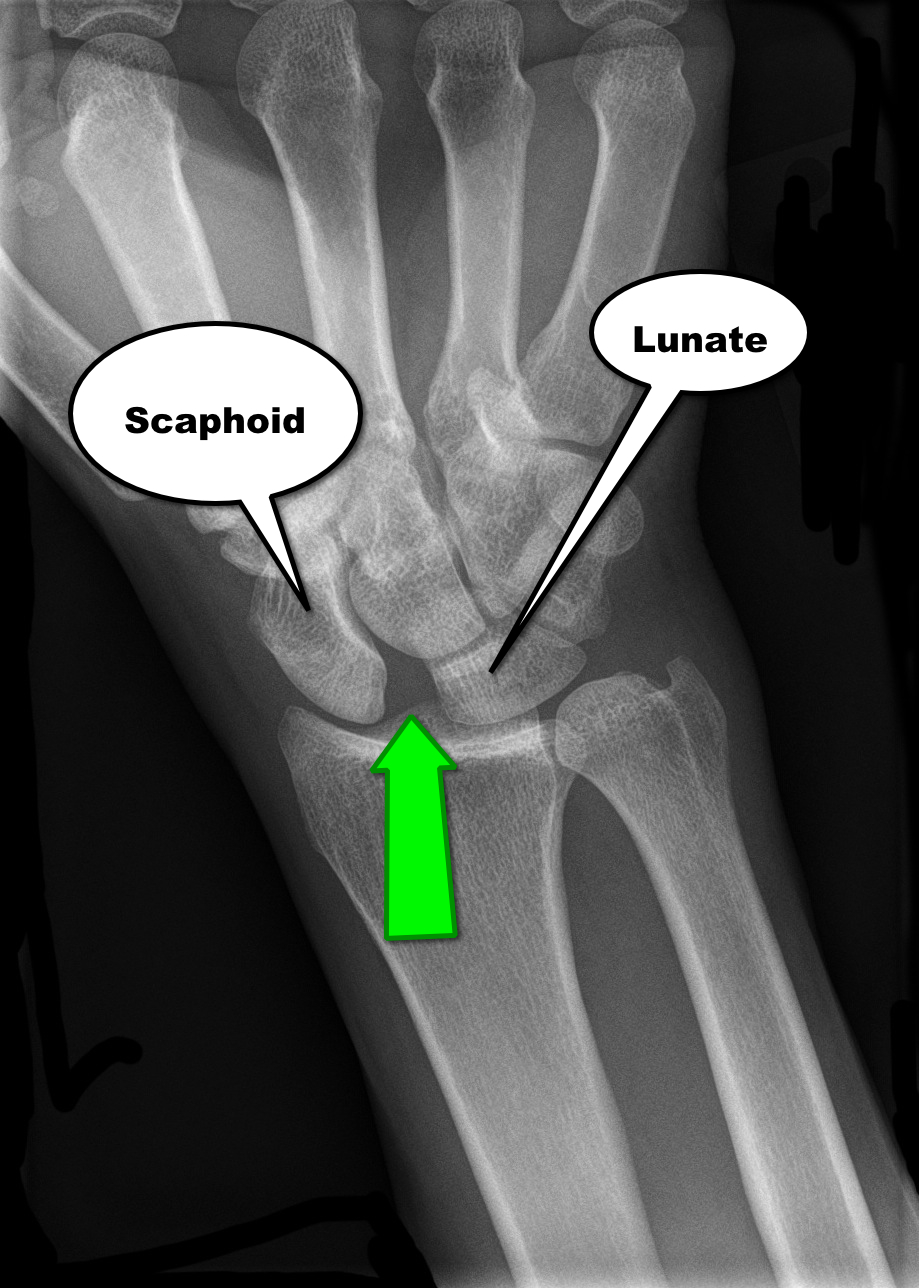
30 year-old male presents with right wrist pain after falling off his bicycle. What's the diagnosis?
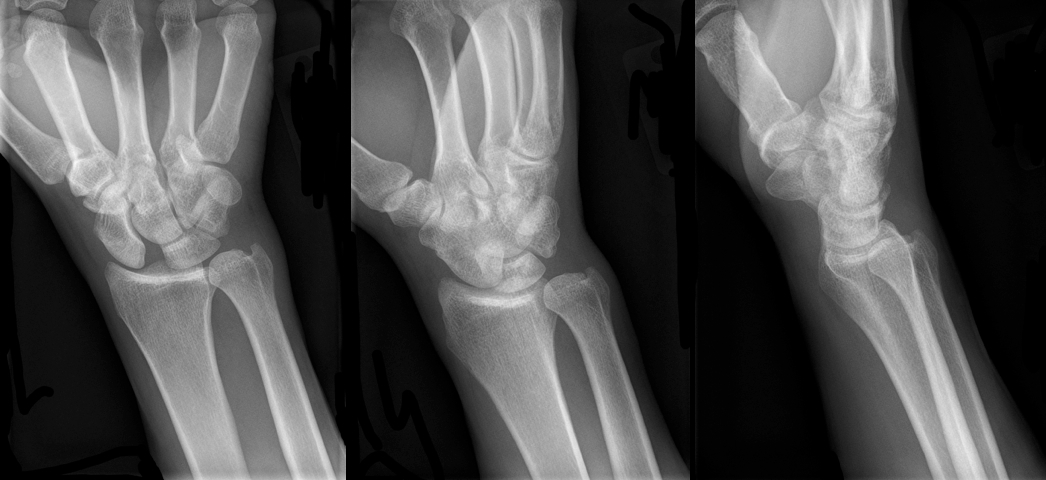
Scapholunate dislocation
Scapholunate Dislocation (a.k.a. “Terry Thomas” or “David Letterman” sign)
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 5/19/2013 by Semhar Tewelde, MD
(Updated: 2/9/2026)
Click here to contact Semhar Tewelde, MD
Than M, Cullen L. 2-Hour Accelerated Diagnostic Protocol to Assess Patients With Chest Pain Symptoms Using Contemporary Troponins as the Only Biomarker. J Am Coll Cardiol. 2012;59(23):2091-2098
Category: Orthopedics
Keywords: Fabella (PubMed Search)
Posted: 5/18/2013 by Michael Bond, MD
(Updated: 2/9/2026)
Click here to contact Michael Bond, MD
Fabella Syndrome
The fabella is a sesamoid bone that is embedded in the tendon of the gastrocnemius muscle where the fibers of the popliteus, arcuate complex and the fibular-fabellar ligament attach.
Fabella syndrome is a painful condition of the posterolateral knee that is exacerbated when the knee is extended. The pain can be exacerbated by palpation of the fabella and if it is compressed against the condyles. The condition is most common in adolescence, but occurs in adults too.
Consider this condition in patients with posterolateral knee pain, which can also be due to tears of the posterior horn of the lateral meniscus, and tendonitis of the lateral head of the gastrocnemius.
Category: International EM
Posted: 5/15/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General information:
· Salmonella typhi – transmission through fecal-oral, contaminated food, human carriers
· Most cases in the US acquired abroad – Africa, Latin American, Asia
· Vaccine available – not life-long immunity, need 1-2 weeks to take effect
Clinical Presentation:
· sustained high fever (103-104)
· Faget sign: fever and bradycardia (also seen in yellow fever, atypical pneumonia, tularemia, brucellosis, Colorado tick fever))
· Abdominal pain, GI bleed/perforation, hepatosplenomegaly, delirium
· “Rose spots” – erythematous macular rash over chest and abdomen
· Without treatment sx can resolve after 3-4 weeks, mortality from secondary infections 12-30%
Diagnosis:
· Pan-culture for S. typhi
· Serologic: Widal test (negative for 1st week of symptoms, 7-14 days to result)
Treatment:
· Abx: amoxicillin, trimethoprim-sulfamethoxazole, and ciprofloxacin
· MDR typhoid: ceftriaxone or Azithromycine 1st line
Bottom Line:
· Get vaccinated if travelling to endemic areas 1-2 weeks before travel
· Suspect in travelers to endemic areas with sustained high fevers
· Spontaneous resolution does occur but may become carriers without abx
Famous victims or Typhoid fever:
· Wilbur Wright (Wright brothers)
· Prince Albert (Queen Victoria’s husband)
· Hakaru Hashimoto (discovered Hashimoto’s thyroiditis)
· Abigail Adams (1st Lady, wife of John Adams)
University of Maryland Section of Global Emergency Health
Author: Veronica Pei, MD
http://www.cdc.gov/nczved/divisions/dfbmd/diseases/typhoid_fever/technical.html#risk
Category: Critical Care
Posted: 5/14/2013 by Mike Winters, MBA, MD
(Updated: 2/9/2026)
Click here to contact Mike Winters, MBA, MD
Monitoring Hyperosmolar Therapy
Hinson HE, Stein D, Sheth KN. Hypertonic Saline and Mannitol in Critical Care Neurology. J Intensive Care Med 2013; 28:3-11.
Category: Visual Diagnosis
Posted: 5/13/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
60 year-old male with a history of pulmonary fibrosis presents to the Emergency Department after a lung biopsy. He is complaining of facial swelling and dyspnea. What's the diagnosis?

Answer: Massive subcutaneous emphysema
Click here
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: CRS (PubMed Search)
Posted: 5/9/2013 by Semhar Tewelde, MD
(Updated: 5/12/2013)
Click here to contact Semhar Tewelde, MD
Ronco C, et al. Cardiorenal Syndrome Type I: Pathophysiological Crosstalk Leading to Combined Heart and Kidney Dysfunction in the Setting of Acutely Decompensated Heart Failure. JACC Vol. 60, No. 12, 2012
Category: Airway Management
Keywords: spine, back pain, osteophyte (PubMed Search)
Posted: 5/11/2013 by Brian Corwell, MD
(Updated: 2/9/2026)
Click here to contact Brian Corwell, MD
Diffuse Idiopathic Skeletal Hyperostosis
aka 1) ankylosing hyperostosis, 2) Vertebral osteophytosis
Large amount of osteophyte formation in the spine, confluent, spanning 3 or more disks
Most commonly seen in the thoracic and thoracolumbar spine.
Osteophytes follow the course of the anterior longitudinal ligaments.
2:1 male to female ratio. Most patients >60yo.
Sx's: Longstanding morning and evening spine stiffness.
PE: Spinal stiffness with flexion and extension.
Dx: plain films
Tx: NSAIDs and physical therapy
http://www.learningradiology.com/caseofweek/caseoftheweekpix2013%20538-/cow542-1arr.jpg
Category: Pediatrics
Posted: 5/10/2013 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
MedStudy Pediatrics Board Review Core Curriculum
Category: Toxicology
Keywords: strychnine, seizure, tetanus (PubMed Search)
Posted: 5/7/2013 by Bryan Hayes, PharmD
(Updated: 5/9/2013)
Click here to contact Bryan Hayes, PharmD
Strychnine poisoning is still occasionally found in rat poisons and in adulterated street drugs and herbal products. The typical symptoms are involuntary, generalized muscular contractions resulting in neck, back, and limb pain. The contractions are easily triggered by trivial stimuli (such as turning on a light) and each episode usually lasts for 30 seconds to 2 minutes, for 12 to 24 hours. Classic signs include opisthotonus, facial trismus, and risus sardonicus.
Differential diagnosis includes:
Chan Y. Chapter 112. Strychnine. In: Chan Y, ed. Goldfrank's Toxicologic Emergencies. 9th ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=6528306. Accessed May 7, 2013.
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Posted: 5/8/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Case Presentation:
A Spanish speaking man in his late 20s is brought in by ambulance for severe dyspnea. Given the language barrier and his clinical status you are unable to obtain any history. He is tachypnic, had a low pulse ox, and was placed on BiPAP. On exam you hear bibasilar rales and a faint holosystolic murmur.
Clinical Question:
What should be included in the differential?
Answer:
Rheumatic heart disease is the result of valvular damage due to an abnormal immune response following a group A streptococcal infection. It affects 15.6 to 19.6 million people worldwide. Most patients present with dyspnea between the ages 20-50. The most common valvular disease is mitral insufficiency, but it may present with mitral stenosis or aortic regurgitation. The disease is most prevalent in sub-Saharan Africa and among the Indigenous population of Australia but it can be found in many developing countries. People who live in rural areas without access to medical care are those at highest risk for developing rheumatic fever and subsequently rheumatic heart disease.
Bottom Line:
Rheumatic heart disease should be considered in patients who present from an endemic region.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg, MD, MPH
Marijon E, Mirabel M, Celermajer DS, Jouven X. Rheumatic heart disease. Lancet. 2012 Mar 10;379(9819):953-64. doi: 10.1016/S0140-6736(11)61171-9.
(Not really a reference but a short documentary nominated for an Oscar this year.)
Category: Critical Care
Posted: 5/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Fluid boluses are often administered to patients in shock as a first-line intervention to increase cardiac output. Previous literature states, however, that only 50% of patients in shock will respond to a fluid bolus.
Several validated techniques exist to distinguish which patients will respond to a fluid bolus and which will not; one method is the passive leg raise (PLR) maneuver (more on PLR here). A drawback to PLR is that it requires direct measurement of cardiac output, either by invasive hemodynamic monitoring or using advanced bedside ultrasound techniques.
Another technique to quantify changes in cardiac output is through measurement of end-tidal CO2 (ETCO2). The benefits of measuring ETCO2 is that it can be continuously measured and can be performed non-invasively on mechanically ventilated patients.
A 5% or greater increase in end-tidal CO2 (ETCO2) following a PLR maneuver has been found to be a good predictor of fluid responsiveness with reliability similar to invasive measures.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 5/5/2013 by Haney Mallemat, MD
(Updated: 5/6/2013)
Click here to contact Haney Mallemat, MD
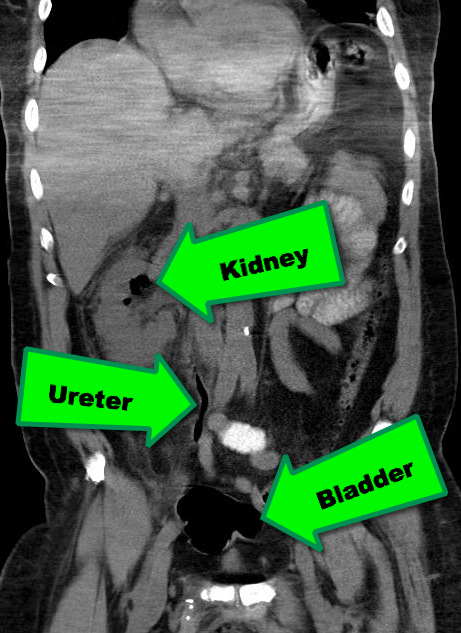
38 year-old male with a past medical history of diabetes presents with back pain and hypotension. CT scan is shown below. What's the diagnosis?
Emphysematous Pyelonephritis (EPN)
EPN is a necrotizing infection of the renal and peri-nephric tissues with accumulation of gas within the tissues and collecting system of the kidney; it is rapidly fatal if not recognized and aggressively treated early.
Risk factors include an immunocompromised host; Diabetics are at particularly increased risk.
The most common etiologic organisms are Escherichia coli, Klebsiella pneumoniae, Proteus mirabilis, and Pseudomonas aeruginosa. Infection with anaerobic species is relatively uncommon.
In addition to the classic signs / symptoms of pyelonephritis, (e.g., flank pain, fever, pyuria, etc.), patients presenting with EPN may experience the passage of air in the urine (pneumaturia) or crepitus over their flank.
Abdominal CT scan is the diagnostic test of choice when clinical presentation and laboratory tests are suggestive (see below)
Treatment should include:
Follow me on Twitter (@criticalcarenow) or Google+(criticalcarenow)
Category: Cardiology
Keywords: Postural Tachycardia Syndrome, POTS (PubMed Search)
Posted: 5/2/2013 by Semhar Tewelde, MD
(Updated: 5/5/2013)
Click here to contact Semhar Tewelde, MD
Grubb B. Postural Tachycardia Syndrome. Circulation 2008; 117:2814-2817
Category: Pharmacology & Therapeutics
Keywords: phosphate, fosphenytoin, phenytoin, hyperphosphatemia (PubMed Search)
Posted: 4/29/2013 by Bryan Hayes, PharmD
(Updated: 5/2/2013)
Click here to contact Bryan Hayes, PharmD
Introduction
Fosphenytoin is a prodrug and is metabolized quickly to phenytoin after administration. The conversion of fosphenytoin to phenytoin involves the release of phosphate. In fact, each mmol of fosphenytoin releases 1 mmol of phosphate.
Clinical Question
Are patients at risk for hyperphosphatemia after fosphenytoin loading?
Data
There are only two cases of reported hyperphosphatemia.
Bottom Line
Despite the phosphate load from fosphenytoin administration, hyperphosphatemia is very rare and probably associated with renal insufficiency and dosing errors.
McBryde KD, et al. Hyperphosphatemia due to fosphenytoin in a pediatric ESRD patient. Pediatr Nephrol. 2005;20(8):1182-5. [PMID 15965770]
Rose R, et al. Fosphenytoin-induced bradyasystole arrest in an infant treated with charcoal hemofiltration [abstract]. J Toxicol Clin Toxicol. 1998;36:473.
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: stroke, children, infection (PubMed Search)
Posted: 5/3/2013 by Jenny Guyther, MD
(Updated: 2/9/2026)
Click here to contact Jenny Guyther, MD
Acute ischemic stroke occurs in 3.3/100,000 children per year. Up to 30% of these are caused by varicella. This can be diagnosed if the patient has had varicella infection within the past 12 months, has a unilateral stenosis of a great vessel, and has a positive PCR or IgG from the CSF.
Treatment includes anticoagulation, acyclovir for at least 7 days and steroids for 3-5 days.
Outcome is normally good and spontaneous improvement can be seen.
Inflammation of other arteries, including other areas of the brain, can also be seen. Treatment options for this can include high dose glucocorticoids and possibly immunosuppresive agents.
Simma et al. Therapy in pediatric stroke. Eur J Pediatr. Published online 06 November 2012.
Category: Pharmacology & Therapeutics
Keywords: Prothrombin Complex Concentrate, warfarin, coumadin, vitamin K antagonist, anticoagulant, PCC (PubMed Search)
Posted: 5/2/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Approval of Kcentra™ may open the door for studying treatment of the bleeding patient on newer oral anticoagulants.
Category: International EM
Keywords: antibiotics, concentration-dependent, infectious disease, international, levofloxacin, gentamicin (PubMed Search)
Posted: 5/1/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information: Antibiotics are generally classified as time- and concentration-dependent.
Concentration-dependent antibiotics
-Fluoroquinolones (i.e. Levofloxacin)
-Aminoglycosides (i.e. Gentamicin)
-Azithromycin
Relevance to the EM Physician:
Concentration-dependent antibiotics should be given at the highest appropriate dose for the target tissues (i.e. Levofloxacin 750mg for pneumonia is preferable to 500mg). This is also the rationale for high dose, extended-interval dosing for Gentamicin (>5mg/kg initial dose).
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Levison ME and Levison JH. Pharmacokinetics and Pharmacodynamics of Antibacterial Agents. Infect Dis Clin N Am. 23(2009): 791-815.
