Category: Pediatrics
Posted: 9/15/2012 by Rose Chasm, MD
(Updated: 2/8/2026)
Click here to contact Rose Chasm, MD
Category: Toxicology
Keywords: cyanide, smoke inhalation, enclosed-space fire, carbon monoxide (PubMed Search)
Posted: 9/7/2012 by Bryan Hayes, PharmD
(Updated: 9/13/2012)
Click here to contact Bryan Hayes, PharmD
Carbon monoxide (CO) and hydrogen cyanide (HCN) are two of the main gases causing injury and death from smoke inhalation in fire victims. During the first phase of a fire, and prior to depletion of oxygen reserves and subsequent production of CO, formation of HCN from the thermal breakdown of nitrogen-containing materials may be the primary cause of lethal poisoning in an enclosed-space fire.
A recent, retrospective, observational study from Poland assessed the prevalence of toxic HCN exposure in victims of enclosed-space fires.
Important findings:
Conclusion: The high prevalence of coincident HCN concentrations and COHb levels in victims of enclosed-space fires emphasises the need to suspect HCN as a co-toxin in all persons rescued from fire who show signs and symptoms of respiratory distress.
Grabowska T, et al. Prevalence of hydrogen cyanide and carboxyhaemoglobin in victims of smoke inhalation during enclosed-space fires: a combined toxicological risk. Clin Toxicol 2012;50:759-63.
Follow me on Twitter (@PharmERToxGuy)
Category: Critical Care
Posted: 9/11/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
40 year-old male with severe uncontrolled hypertension presents with altered mental status (head CT below). The CXR is from the same patient. What's the connection?
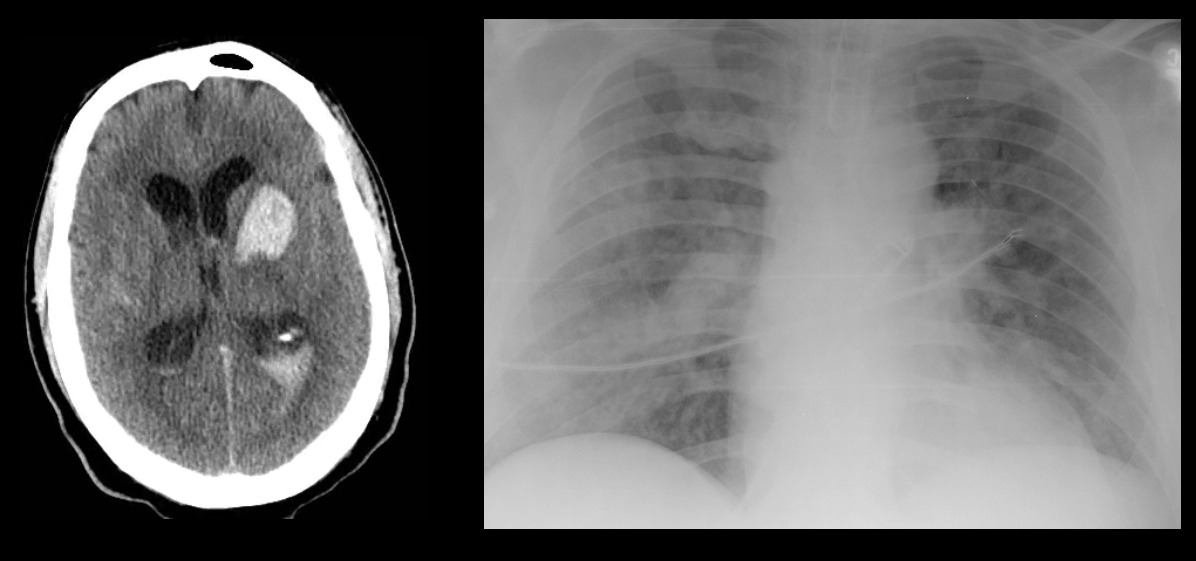
Answer: Neurogenic pulmonary edema (NPE)
NPE is defined as acute pulmonary edema following central nervous system (CNS) insult; NPE has been recognized for over 100 years, but its incidence is underreported due to a lack objective clinical criteria.
The pathophysiology of NPE is poorly understood but it is generally believed that both cardiogenic and non-cardiogenic pulmonary edema play a role. CXR (see above) demonstrates a pattern similar to acute respiratory distress syndrome (i.e., bilateral interstitial infiltrates).
CNS insults that are abrupt, rapidly progressive, and increase intracranial pressure (e.g., subarachnoid hemorrhage, intraparenchymal hemorrhage, traumatic brain injury, subdural, etc.) have the highest risk for NPE. Neural injury leads to sympathetic activation, the release of catecholamines, and one or all of the following:
Treatment of NPE includes:
Davidson, D. et al. Neurogenic pulmonary edema. Crit Care. 2012 Mar 20;16(2):212.
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Visual Diagnosis
Posted: 9/10/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
40 year-old male with severe uncontrolled hypertension presents with altered mental status. Head CT is shown here. Name three common anatomic locations generally seen for non-traumatic intracerebral hemorrhage.
Answer: The most common anatomic sites for intra-cerebral hemorrhage are:
...and, don't forget the most common causes of non-traumatic intra-cerebral hemorrhage:
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Cardiology
Keywords: mean arterial pressure, blood pressure (PubMed Search)
Posted: 9/9/2012 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Which patient has a better blood pressure, the patient with a blood pressure of 110/40 or the patient with a blood pressure of 90/60?
Mean arterial pressure (MAP) is generally considered to be the organ perfusion pressure in an individual. Because MAP requires an inconvenient calculation, we've all been taught...misled perhaps...into focusing on systolic blood pressure (SBP) as a marker of how well-perfused a patient is, and we tend to ignore the diastolic blood pressure (DBP).
It's important to remember, however, that we spend most of our lives in diastole, not systole. As a result, our organs spend more time being perfused during diastole than systole. The MAP takes this into account: MAP = (SBP + DBP + DBP)/3. DBP is more important than SBP!
So which patient is perfusing his vital organs better, the one with a BP of 110/40 or the one with a BP of 90/60? Do the MAP calculation...90/60 is better than 110/40!
Pay more attention to those diastolic BPs!
Category: Orthopedics
Keywords: Apprehension test, patellar dislocation, (PubMed Search)
Posted: 9/8/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Apprehension test for patellar dislocation
Test is used to access for the possibility of a patellar dislocation, prior to evaluation, now spontaneously reduced.
Similar to the shoulder apprehension test
Designed to place the patella in a position of imminent subluxation or dislocation
http://mulla.pri.ee/Kelley%27s%20Textbook%20of%20Rheumatology,%208th%20ed./HTML/f4-u1.0-B978-1-4160-3285-4..10042-7..gr16.jpg
http://www.youtube.com/watch?v=9AJxcbd9g8A
Place the knee in 20 - 30 degrees of flexion with the quadripces relaxed. Grasp the patella and attempt to place lateral directed stress.
If the patella is about to dislocate, the patient will experience apprehension due to the familiar pattern of dislocation, report the laxity and resist further motion by contracting the quadriceps
Category: Pediatrics
Keywords: cervical spine, trauma, pediatrics (PubMed Search)
Posted: 9/7/2012 by Lauren Rice, MD
Click here to contact Lauren Rice, MD
Ligamentous laxity is increased in children and ligamentous injury is more common than fractures.
If fractures occur, they are more likely to be in the upper cervical spine in infants and the lower cervical spine in older children.
Pseudosubluxation: physiologic subluxation between C2-3 and C3-4 may exist until age 16 years
Screening Assessment/Clearance for Verbal Children
-Midline C-spine tenderness?
-Pain with active motion?
-Altered level of alertness?
-Evidence of intoxication?
-Focal neurological deficit?
-Distracting painful injury?
-High impact injury?
Screening Assessment/Clearance for Pre-Verbal Children
-Neurological assessment of basic reflexes
-Response to painful stimuli
-Equal movements of all extremities
-Response to sound (eye tracking)
-Extremity strength and resistance
-Palpate posterior C-spine (observe for facial grimace)
-Feel for step-offs, deformities
-Verify full range of motion of neck (may need to be creative)
-Repeat neurological assessment
If concern arises on screening assessment, keep child in hard cervical collar and image (may start with x-ray and progress to CT if still concerned and x-rays negative).
If imaging negative, but persistent suspicion based on neurological deficits consider SCIWORA (Spinal Cord Injury WithOut Radiographic Abnormality) which exists in up to 50% of children with cervical cord injury, and may require MRI to further identify injury.
Category: Toxicology
Keywords: organophosphates, intermediate syndrome (PubMed Search)
Posted: 9/6/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Category: Critical Care
Posted: 9/4/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Right Heart Failure in the Critically Ill
Greyson CR. Right heart failure in the intensive care unit. Curr Opin Crit Care 2012; 18:424-31.
Category: Visual Diagnosis
Posted: 9/3/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
32 year-old female presents with 5 days of fever, chills, and flank pain. She is hypotensive on presentation and urinalysis shows pyuria. Click here for the non-contrast CT scan. What's the diagnosis and what type of antibiotics should be started empirically?
Answer: Staghorn caliculi secondary to struvite stone. Broad-spectrum antibiotics to cover anaerobic bacteria should be initiated.
Follow me on Twitter (@criticalcarenow) and Google+ (+haneymallemat)
Category: Cardiology
Keywords: Lyme disease, Lyme carditis, AV block (PubMed Search)
Posted: 9/2/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Lyme disease is the most prevalent arthropod zoonosis in the Northern hemisphere
Rostoff P, Gajos G, Konduracka E, Gackowski A, Nessler J, Piwowarsk W. Lyme carditis: Epidemiology, pathophysiology, and clinical features in endemic areas. International Journal Cardiology
Category: Pharmacology & Therapeutics
Keywords: carbapenem, penicillin, allergy, skin test, cross-reactivity (PubMed Search)
Posted: 8/26/2012 by Bryan Hayes, PharmD
(Updated: 9/4/2013)
Click here to contact Bryan Hayes, PharmD
Carbapenems (meropenem, ertapenem, doripenem, imipenem/cilastatin) are broad-spectrum antibiotics that have good gram-negative and anaerobic coverage and are used to treat resistant bacterial infections.
Early retrospective studies showed ~10% cross-reactivity in penicillin-allergic patients.
More recent prospective studies verified penicillin allergy by the accepted standard (ie, skin test to the major and minor penicillin determinants) and tested for carbapenem allergy by administering a full therapeutic dose to carbapenem skin test-negative patients.
The cross-reactivity between skin tests appears to be around 1%, with all carbapenem skin test-negative patients tolerating the challenge.
Frumin J, Gallagher JC. Allergic cross-sensitivity between penicillin, carbapenem, and monobactam antibiotics: what are the chances? Ann Pharmacother 2009;43(2):304-15.
Herbert ME, Brewster GS, Lanctot-Herbert M. Medical myth: ten percent of patients who are allergic to penicillin will have serious reactions if exposed to cephalosporins. West J Med 2000;172:341.
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: septic shock, fluid resuscitation, PALS (PubMed Search)
Posted: 8/31/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: LSD, hashish, marijuana, jobs (PubMed Search)
Posted: 8/30/2012 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
I was reading the biography of Steve Jobs looking for incredible insights into leadership and innovation. I have realized that you basically have to be a genuis and it doesn't matter what you do. His favorite drug was LSD which he believed was necessary to improve creativity and innovation. His description of the hallucinations confirm that he was taking this drug.
We describe LSD hallucinations as a crossing of the senses or "synesthesias" - you hear the color blue, you see the smell of roses.
Steve Jobs describes a moment in a wheat field while on LSD and (paraphrasing from the biography) ..." the wheat was playing Bach beautifully"
If you have a patient describing this type of hallucination you can almost be guaranteed that they have taken LSD or some other tryptamine.
Category: Critical Care
Posted: 8/28/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A Cochrane review of 37 studies concluded that Succinylcholine (SUC) is superior to Rocuronium (ROC) during rapid sequence intubation.
The authors claim that compared to ROC, SUC has a faster onset of action (45 vs. 60 seconds) and overall a shorter duration of action (10 vs. 60 minutes).
Dr. Reuben Strayer wrote a letter to the journal editors and stated that these findings should be interpreted carefully; he highlighted that most of the studies in the review used doses of ROC less than 0.9 mg/kg (most studies used 0.6mg/kg).
Dr. Strayer asserted that ROC’s onset of action is dose dependent; when using doses of 1.2 mg/kg, ROC’s onset is indistinguishable from that of SUC. He also stated another major benefit of ROC is the lack of adverse effects that SUC possesses (hyperkalemia and malignant hyperthermia).
What are your thoughts on this? Go to http://www.facebook.com/Criticalcarenow and take the poll (there are 5 choices). Results will be posted next week.
Seupaul RA, Jones JH. Evidence-based emergency medicine. Does succinylcholine maximize intubating conditions better than rocuronium for rapid sequence intubation? Ann Emerg Med. 2011 Mar;57(3):301-2. Epub 2010 Nov 18.
Strayer RJ. Rocuronium versus succinylcholine: Cochrane synopsis reconsidered. Ann Emerg Med. 2011 Aug;58(2):217-8.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 8/27/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
56 year-old male presents with chest pain. You perform an ultrasound of the heart and see the clip below. What's the diagnosis? Thanks to Dr. Ken Butler for the case.
Answer: Type A Dissection
Click here for an explanation.
Follow me on Twitter (@criticalcarenow) and Google+ (+haney mallemat)
Category: Cardiology
Keywords: ARVD, ARVC, cardiomyopathy, triangle of dysplasia, ICD (PubMed Search)
Posted: 8/26/2012 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Arrhythmogenic right ventricular dysplasia (ARVD) is a heritable form of cardiomyopathy, characterized by the replacement of myocytes with adipose and fibrous tissue leading to arrhythmias, right ventricular failure, and sudden cardiac death (SCD)
ECG findings include T-wave inversions in V1–V3 (85% ), epsilon waves (in 33%), as well as a QRS duration >110 ms in V1-V3 (64%)
Azaouagh A, Churzidse S, Konorza T, Erbel R. Arrhythmogenic right ventricular cardiomyopathy/dysplasia: a review and update. Clin Res Cardiol (2011) 100:383–394.
Category: Orthopedics
Keywords: shoulder dislocation, apprehension (PubMed Search)
Posted: 8/25/2012 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Apprehension test for shoulder dislocation
Tests for chronic shoulder dislocation
Similar to the patellar apprehension test
Designed to place the humeral head in a position of imminent subluxation or dislocation
http://www.maitrise-orthop.com/corpusmaitri/orthopaedic/112_kelly/kelly-fig11.jpg
ABduct and externally rotate arm to a position where the shoulder may dislocate
If the shoulder is about to dislocate, the patient will experience apprehension due to the familiar pattern of dislocation, report the laxity and resist further motion.
Category: Pediatrics
Posted: 8/24/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Types:
- Uniphasic anaphylaxis: occuring immediately after exposure to allergen, resolves over minutes to hours and does not recur
- Biphasic anaphylaxis: occuring after apparent resolution of symptoms typically 8 hours after the first reaction. Occur in up to 23% of adults and up to 11% of children with anaphylaxis
Treatment:
1. First line: IM epinephrine 1:1000 solution
- vasoconstrictor effects on hypotension and peripheral vasodilation; bronchodilator effects on upper respiratory obstruction
- NO absolute contraindication for use in anaphylaxis
- Dosage: Adult: 0.3 - 0.5mg; Peds: 0.01mg/kg (max 0.3mg)
- can be repeated every 5-15 minutes
2. Adjunctive therapy:
- H1 Blocker: diphenhydramine 1-2mg/kg up to 50mg IV
- H2 Blocker: ranitidine 1-2mg/kg
- Corticosteroid: 1-2 mg/kg for prevention of biphasic reactions
- Bronchodilator: Albuterol for bronchospasm
- Glucagon: for refractory hypotension or if patient is on beta blocker
- Dosage: Adult: 1-5 mg; Peds 20-30microgm/kg
- Dose may be repeated or followed by infusion of 5-15 mg/min
- place patient in recumbent position if tolerated with lower extremities elevated
- supplemental O2
- IV fluids for hypotension
Fatalities: typically seen with peanut or treenut ingestions from cardiopulmonary arrest. Associated with delayed or inappropriate epinephrine dosing
Disposition:
- Mild reaction with symptom resolution: observe for 4-6 hrs (ACEP, AAP)
- Recurrent symptoms or incomplete resolution: admit
Reference:
1. World Allergy Organization Guidelines for the Assessment and Management of Anaphylaxis, Feb 2011
2. Guidelines for the Diagnosis and Management of Food Allergy in the United States: Report of the NIAID-Sponsored Expert Panel Oct 2010
Category: Toxicology
Keywords: valproic acid, carnitine (PubMed Search)
Posted: 8/23/2012 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Patients that experience altered mental status (specifically lethargy) and are on valproic acid - check a serum ammonia level regardless if it is an overdose or just therapeutically on VPA.
If the ammonia is elevated in combination with the mental status change consider administration of L-carnitine either po or IV. It will lower the ammonia and improve the mental status within hours.
High risk patients for hyperammonia who therapeutically take VPA are certain pediatric patients that experience malnutrition, have seizure disorder and are on multiple seizure medications.
Department of Emergency Medicine, Erasme University Hospital, Universite Libre de Bruxelles, Brussels, Belgium. plheureu@ulb.ac.be
