Category: Orthopedics
Keywords: Distal radius fracture, wrist, splint (PubMed Search)
Posted: 2/27/2021 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Home management versus PCP follow-up of patients with distal radius buckle (torus) fractures
A recent study investigated outcomes of patients with distal radius buckle fractures who were randomized to
Versus
Noninferior study
Torus/buckle fractures of the distal radius are the most common fractures in childhood occurring on average in 1 in 25 children
This is a stable fracture typically treated with removable wrist splint and very rarely require orthopedic intervention
Outcome: functional recovery at 3 weeks
Randomized controlled trial at a tertiary care children’s hospital
All radiographs reviewed by pediatric radiologist with MSK specialization
149 patients. Mean age 9.5 years. 54.4% male
Telephone follow-up at 3 and 6 weeks following ED discharge by blinded interviewer
Primary outcome was comparison of Activities Scale for Kids-performance scores between groups at 3 weeks
Outcomes: Home management performance score was 95.4% and PCP follow-up group was 95.9%. Mean cost savings were $100.10.
Conclusion: Home management is at least as good as PCP follow-up with respect to functional recovery in ED patients with distal radius buckle fractures.
Colaco et al. Home management versus primary care physician follow-up of patients with distal radius buckle fractures: A randomized controlled trial. Ann Emerg Med. 2021
Category: Neurology
Keywords: Bell's palsy, facial palsy, Lyme disease, Borrelia burgdorferi (PubMed Search)
Posted: 2/24/2021 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: In a Lyme-endemic area, the incidence of positive Lyme tests and Bell’s palsy are highest in the Lyme months. This seasonal variation may help guide the management of patients with Bell’s palsy.
Pacheco A, Rutler O, Valenzuela I, Feldman D, Eskin B, Allegra JR. Positive tests for Lyme disease and emergency department visits for Bell’s Palsy patients. J Emerg Med. 2020;59(6):820-827.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: HACOR, NIV, noninvasive ventilation, acute respiratory failure (PubMed Search)
Posted: 2/2/2021 by Kami Windsor, MD
(Updated: 2/23/2021)
Click here to contact Kami Windsor, MD
Background: In respiratory failure due to COPD and cardiogenic pulmonary edema, noninvasive positive pressure ventilation decreases need for intubation and improves mortality,1 while its utility in other scenarios such as ARDS and pneumonia has yet to be proven.1,2 We know that patients on NIV with delays to needed intubation have a higher mortality,1,3 but intubation and mechanical ventilation come with risks that it is preferable to avoid if possible.
So how and when can we determine that NIV is not working?
The HACOR (Heart rate, Acidosis, Consciousness, Oxygenation, Respiratory rate) score at 1 hour after NIV initiation has been demonstrated to be highly predictive of NIV failure requiring intubation.4,5
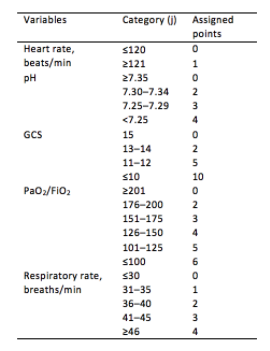
Initial development/validation: Score > 5 after 1 hour of NIV corresponds to >80% risk of NIV failure4
Earlier intubation (before 12 hours) in these patients = better survival
External validation: Score > 8 after 1 hour of NIV most predictive of eventual NIV failure 5
Average score @ 1-hour of patients with NIV success = 3.8
Score remained predictive at 6, 12, 24, 48 hours as well & mortality worsened as delay to intubation time increased
Baseline, pre-NIV score not predictive
Better predictive agreement in pneumonia and ARDS
Bottom Line:
Patients on NIV require close reassessment to prevent worsened survival due to intubation delay should invasive mechanical ventilation be indicated.
A HACOR score >8 after 1 hour of NIV should prompt intubation in most instances, with strong consideration given to a score >5.
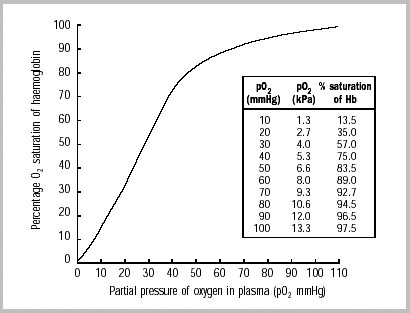
*Note: ABGs were obtained for PaO2 assessment in the above studies -- the use of SpO2 was not evaluated -- but we are often not obtaining ABGs in our ED patients with acute respiratory failure. The following chart provides an estimated SpO2 to PaO2 conversion.
WHO 2001
Caveats:
Category: Pediatrics
Keywords: Congestive heart failure, trouble breathing, basic natriuretic peptide (PubMed Search)
Posted: 2/19/2021 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
In children with known congenital heart disease, BNP measurements are higher in those patients with heart failure compared to those without heart failure.
The utility of BNP in differentiating a cardiac from pulmonary pathology in patients with respiratory distress has been studied in pediatrics. In one study involving 49 infants with respiratory distress, the patients with a final diagnosis of heart failure had a higher mean BNP concentration than those patients with other causes. Also, there is a suggestion that the relative change in NT proBNP levels may be useful in patients with underlying pulmonary hypertension. However, currently there is not enough literature to support the routine use of BNP or NT proBNP in acute management.
Bottom line: BNP can be useful in your patient with congenital heart disease who is decompensating and may be used in a patient where there is difficulty in differentiating a primary respiratory from cardiac etiology.
Davis GK, Bamforth F, Sarpal A, et al. B-type natriuretic peptide in pediatrics. Clin Biochem. 2006 Jun;39(6):600-5.
Nir A, Lindinger A, Rauh M, et al. NT-pro-B-type natriuretic peptide in infants and children: reference values based on combined data from four studies. Pediatr Cardiol. 2009 Jan;30(1):3-8.
Ten Kate CA, Tibboel D, Kraemer US. B-type natriuretic peptide as a parameter for pulmonary hypertension in children. A systematic review. Eur J Pediatr. 2015 Oct;174(10):1267-75.
Category: Toxicology
Keywords: Haloperidol, ondansetron, cannabis hyperemesis syndrome (PubMed Search)
Posted: 2/18/2021 by Hong Kim, MD
Click here to contact Hong Kim, MD
Patients with cannabis hyperemesis syndrome experience recurrent/protracted nausea/vomiting. Cases of cannabis hyperemesis syndrome may increase as cannabis use becomes more common in the United States.
A randomized control trial (triple-blind) was conducted to compare haloperidol (0.05 or 0.1 mg/kg) IV or ondansetron 8 mg IV. Primary outcome was reduction of abdominal pain and nausea from baseline (on a 10 cm visual analog scale) 2 hours after treatment.
Results
Conclusion
Ruberto AJ. et al. Intravenous haloperidol versus ondansetron for cannabis hyperemesis syndrome (HaVOC): a randomized controlled trial. Annals of Emergency Medicine. Nov 2020
https://doi.org/10.1016/j.annemergmed.2020.08.021
Category: Orthopedics
Keywords: diabetes, exercise, weight loss (PubMed Search)
Posted: 2/13/2021 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
What time of day is best for exercise to achieve weight loss goals?
Working out in the morning has traditionally held the edge, especially if done on an empty stomach.
Upon walking, elevated levels of cortisol and GH will aid in fat metabolism.
Switching to a morning workout may also decrease appetite throughout the day.
Morning exercise may also induce significant circadian phase?shifting effects. Patients report feeling more alert in the morning and get more tired at night. This may “force” people to get increased rest as poor sleep quality and duration has been associated with weight gain.
Moderate intensity aerobic exercise has been shown to cause immediate mood improvement and mental productivity. These effects can last up to 12 hours and may be a simple aid to combat job stress.
However, a recent small study looked at this question with a group of men at high risk for Type 2 diabetes.
Those that exercised in the morning had better blood sugar control and lost more abdominal fat than those who exercised in the morning.
Study: 32 adult males (58 ± 7 years) at risk for or diagnosed with type 2 diabetes performed 12 weeks of supervised exercise training either:
In the morning (8.00–10.00 a.m., N = 12) OR
In the afternoon (3.00–6.00 p.m., N = 20)
Test: Graded cycling test with ECG monitoring until exhaustion
Results: Compared to those who trained in the morning, participants who trained in the afternoon experienced superior beneficial effects of exercise training on peripheral insulin sensitivity, insulin?mediated suppression of adipose tissue lipolysis, fasting plasma glucose levels, exercise performance and fat mass.
Conclusion: Metabolically compromised patients may benefit from shifting their exercise routine to the afternoon from the morning. Ultimately, any exercise is great in this population, but this study may be worth sharing to your patients.
Mancilla R, Brouwers B, Schrauwen-Hinderling VB, Hesselink MKC, Hoeks J, Schrauwen P. Exercise training elicits superior metabolic effects when performed in the afternoon compared to morning in metabolically compromised humans. Physiol Rep. 2021 Jan;8(24):e14669.
Category: Critical Care
Keywords: Oxygenation, Mechanical Ventilation, Critical Care (PubMed Search)
Posted: 2/9/2021 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Optimal oxygenation targets and the possible, theoretical, benefits of hyperoxygenating critically ill patients have long been points of controversy. Multiple studies have suggested harm in pursuing aggressive hyperoxygenation amongst critical patients with various conditions ranging from myocardial infarction to sepsis to neurologic conditions. In addition, oxygen toxicity is a known mechanism causing ARDS.
The HOT-ICU trial adds to the list of arguments against hyperoxygenation, by looking at 2928 ICU patients on high levels of supplemental oxygen and targeting a paO2 of 60 mm Hg (low oxygen group) vs paO2 of 90 mm Hg (high oxygen group). There was no difference in mortality, or other significant difference in outcomes.
Bottom Line: A lower paO2 goal of 60 (correlates to an O2 sat of 90%) is noninferior to a higher paO2 goal of 90 (O2 sat of approximately 96%). When titrating oxygen, targeting a pulse ox of 90-96% is reasonable in critically ill patients. Be sure to include an upper limit on the sat goal, beware an O2 sat of 100%, and titrate down supplemental oxygen when the spO2 is above goal, as the paO2 may be dangerously high.
Schjørring OL, Klitgaard TL, Perner A, Wetterslev J, Lange T, Siegemund M, Bäcklund M, Keus F, Laake JH, Morgan M, Thormar KM, Rosborg SA, Bisgaard J, Erntgaard AES, Lynnerup AH, Pedersen RL, Crescioli E, Gielstrup TC, Behzadi MT, Poulsen LM, Estrup S, Laigaard JP, Andersen C, Mortensen CB, Brand BA, White J, Jarnvig IL, Møller MH, Quist L, Bestle MH, Schønemann-Lund M, Kamper MK, Hindborg M, Hollinger A, Gebhard CE, Zellweger N, Meyhoff CS, Hjort M, Bech LK, Grøfte T, Bundgaard H, Østergaard LHM, Thyø MA, Hildebrandt T, Uslu B, Sølling CG, Møller-Nielsen N, Brøchner AC, Borup M, Okkonen M, Dieperink W, Pedersen UG, Andreasen AS, Buus L, Aslam TN, Winding RR, Schefold JC, Thorup SB, Iversen SA, Engstrøm J, Kjær MN, Rasmussen BS; HOT-ICU Investigators. Lower or Higher Oxygenation Targets for Acute Hypoxemic Respiratory Failure. N Engl J Med. 2021 Jan 20. doi: 10.1056/NEJMoa2032510. Epub ahead of print. PMID: 33471452.
Category: Pharmacology & Therapeutics
Keywords: Buprenorphine, Acute Pain (PubMed Search)
Posted: 2/6/2021 by Wesley Oliver
Click here to contact Wesley Oliver
Buprenorphine is a partial opioid receptor agonist that has a higher binding affinity than pure opioid agonists. There can be unease in managing acute pain in patients sustained on buprenorphine for opioid use disorder due to many factors.
The main barriers to effective pain management in these patients are:
Take Home Points
In general, the treatment strategy for acute pain in patients on buprenorphine should be:
Category: Critical Care
Posted: 2/2/2021 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Mechanical Ventilation in COPD
Demoule A, et al. How to ventilate obstructive and asthmatic patients. Intensive Care Med. 2020; 46:2436-2449.
Category: Neurology
Keywords: seizure, status epilepticus, nonconvulsive, electrographic, EEG (PubMed Search)
Posted: 1/27/2021 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Persistent or recurrent seizures are not uncommon in the first 24 hours after status epilepticus even in patients with resolved clinical seizure activity. Early use of EEG can help identify patients who need further escalation of treatment.
Follow me on Twitter @EM_NCC
Category: Airway Management
Keywords: Myocarditis, Covid-19 (PubMed Search)
Posted: 1/23/2021 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Exercise and Covid-19
The majority of COVID-19 cases fall into the mild-to-moderate category, with symptoms lasting less than 6 weeks on average.
The disease presents a challenge for clinicians seeking to offer counsel for patients wishing to return to exercise.
A recent cohort study in Germany looked at 100 patients (avg. age 49, 53% male) who had recovered from Covid-19 infection.
Most had been healthy, with no pre-existing medical conditions, before becoming infected.
The group had cardiac MRI (CMR) performed.
Average time interval between Covid-19 diagnosis and CMR was 71 days.
Cardiac involvement was seen in 78% of patients and ongoing myocardial inflammation in 60%.
Evidence based return to activity guidelines being developed are more conservative than in the past with other viral infections
https://link.springer.com/article/10.1007/s11420-020-09777-1/tables/1
1) Puntmann VO, Carerj ML, Wieters I, et al. Outcomes of Cardiovascular Magnetic Resonance Imaging in Patients Recently Recovered From Coronavirus Disease 2019 (COVID-19). JAMA Cardiol. 2020;5(11):1265–1273. doi:10.1001/jamacardio.2020.3557
2) Metzl, J.D., McElheny, K., Robinson, J.N. et al. Considerations for Return to Exercise Following Mild-to-Moderate COVID-19 in the Recreational Athlete. HSS Jrnl 16, 102–107 (2020).
Category: Toxicology
Keywords: alcoholic ketoacidosis, toxic alcohol ingestion, anion gap metabolic acidosis (PubMed Search)
Posted: 1/21/2021 by Hong Kim, MD
Click here to contact Hong Kim, MD
Anion gap metabolic acidosis is often found in ED patients. It can be difficult to distinguish between toxic alcohol (TA) ingestion and alcoholic ketoacidosis (AKA). A retrospective study attempted to identify risk factors associated with AKA when TA ingestion was the alternative diagnosis.
New York City poison center data was reviewed from Jan 1, 2000 to April 30, 2019.
Case definition of AKA included
Case definition of TA ingestion
Results
Univariate analysis showed following variables to be associated with AKA diagnosis
Multivariate logistic regression showed elevated ethanol concentration was associated with increased odd of AKA diagnosis
Conclusion
Category: Misc
Posted: 1/20/2021 by Michael Bond, MD
Click here to contact Michael Bond, MD
Title: Mammalian meat allergy (alpha-gal syndrome) following tick bites
Author: Dan Gingold, MD, MPH
Development of IgE antibodies to the oligosaccharide galactose-alpha-1-3-galactose (alpha-gal) appears to be responsible for an acquired allergy to non-primate mammalian meat (i.e., beef and pork) and derived products. Antigen in the salivary apparatus of certain ticks (gross!!) can sensitize an IgE-mediated response to alpha-gal which is present in mammalian meat.
Symptoms are similar to other IgE-mediated hypersensitivity reactions, and can cause a delayed-onset reaction with hives, GI upset, or anaphylaxis after ingestion of red meat. Treatment with standard anti-histamines and epinephrine is effective. Individuals with no prior history of meat sensitivity can develop the syndrome at any age, often after exposure to the outdoors in tick-endemic areas. Skin and blood allergy testing can confirm the diagnosis. Symptoms can persist for years, but can recede over time if not exposed to further tick bites.
In the US, the primary tick responsible is Lone Star Tick (Amblyomma americanum), found primarily in the Eastern, Southeastern, and Midwestern US. Other tick species in Europe, Australia, and Asia have been found to induce the syndrome as well. Interestingly, there is a cross-reactivity with the monoclonal antibody Cetuximab (used to treat colorectal and head and neck cancers), an allergic reaction to which can also induce similar alpha-gal meat sensitivity.
Having first been described in 2009, the syndrome often goes unrecognized; increased physician awareness can inform the evaluation, diagnosis, and education of patients presenting to the ED with undifferentiated allergic reaction.
Further Reading:
Khoury JK, Khoury NC, Schaefer D, Chitnis A, Hassen GW. A tick-acquired red meat allergy. Am J Emerg Med. 2018 Feb;36(2):341.e1-341.e3. doi: 10.1016/j.ajem.2017.10.044. Epub 2017 Oct 16. PMID: 29074067.
Crispell G, Commins SP, Archer-Hartman SA, Choudhary S, Dharmarajan G, Azadi P, Karim S. Discovery of Alpha-Gal-Containing Antigens in North American Tick Species Believed to Induce Red Meat Allergy. Front Immunol. 2019 May 17;10:1056. doi: 10.3389/fimmu.2019.01056. PMID: 31156631; PMCID: PMC6533943.
Category: Critical Care
Posted: 1/19/2021 by Lindsay Ritter, MD
Click here to contact Lindsay Ritter, MD
| Ever wonder what to tell the families regarding prognosis of the sickest COVID-19 patients you intubate in the ED or ICU? Introduction: Case fatality rates (CFR) for COVID-19 patients requiring invasive mechanical ventilation have been widely variable. A study in the Blue Journal (AJRCCM) examined patients requiring intubation in a systemic review and meta-analysis. The case fatality risk of an infection is represented by the proportion of patients who die among all infected cases in a population over a period of time. Methods: 69 studies axross 23 countries for a total of 57,420 patients with COVID-19 who required mechanical ventilation were included in analysis. Results: Overall case fatality rate was 45%, or about 1 death for every two intubated patients.. Among studies that included age stratification, pooled estimates of CFR were 47.9% in patients <40 (CI 46.4-49.4%) and 84.4% in patients >80 (CI 83.3-85.4%). Overall heterogeneity is high (I 2 .90%), In early COVID epicenters, CFR was 70% among patients aged more than 60 years of age. CFR increased exponentially with increasing age. Specifically in the US across 21 studies (3,811 intubated patients), CFR was 47% (95% CI, 36–57%). Studies from New York reported a CFR of 54% (95% CI, 36–72%) whereas other regions in the United States reported a CFR of 41% (95% CI, 30–53%). Definitive hospital CFR (aka for those with hospital discharge outcomes, 13,120 patients) was 56% (CI 47-65%). Conclusion: Almost half of patients with COVID-19 receiving IMV died based on the reported CFR. The reported CFR was higher in older patients and in early pandemic epicenters, which may be influenced by limited ICU resources. Limitations: Overall CFR of 45% still included patients in the hospital. Definitive hospital outcomes were only for 13,120 patients (36.6%). Significant variation in CFR exists between studies. |
Lim ZJ, Subramaniam A, Ponnapa Reddy M, Blecher G, Kadam U, Afroz A, Billah B, Ashwin S, Kubicki M, Bilotta F, Curtis JR, Rubulotta F. Case Fatality Rates for Patients with COVID-19 Requiring Invasive Mechanical Ventilation. A Meta-analysis. Am J Respir Crit Care Med. 2021 Jan 1;203(1):54-66.
Angriman F, Scales DC. Estimating the Case Fatality Risk of COVID-19 among Mechanically Ventilated Patients. Am J Respir Crit Care Med. 2021 Jan 1;203(1):3-4.
Category: Pediatrics
Keywords: Infection, sepsis, lactic acid (PubMed Search)
Posted: 1/15/2021 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Despite a lack of formal guidelines and evidence, lactate measurement has become a component of many pediatric emergency sepsis quality programs, with one survey showing that up to 68% of responding pediatric emergency medicine providers routinely measured it.
The Surviving Sepsis Campaign, last updated in February 2020, could not make a recommendation on the use of lactate in pediatric patients with suspected shock. The authors did state that lactate levels are often measured during the evaluation of septic shock if the lab can be obtained rapidly. However, lactate levels alone would not be an appropriate screening test.
Weiss SL, Peters MJ, Alhazzani W, et al. Surviving sepsis campaign international guidelines for the management of septic shock and sepsis-associated organ dysfunction in children. Intensive Care Med. 2020;46(Suppl 1):10-67.
Scott HF, Brou L, Deakyne SJet al. Association between early lactate levels and 30-day mortality in clinically suspected sepsis in children. JAMA Pediatr. 2017 Mar 1;171(3):249-255.
Category: Neurology
Keywords: stroke, thrombolysis, tissue plasminogen activator, tPA, monitoring (PubMed Search)
Posted: 1/13/2021 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
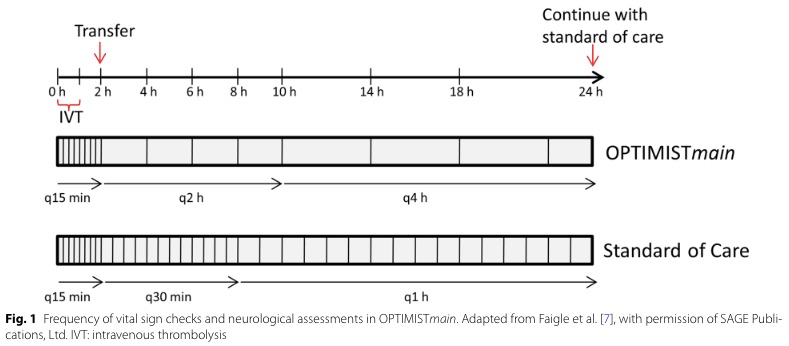
Bottom Line: Patients with NIHSS <10 may be safe for low-intensity post-tPA monitoring if they do not require critical care after an initial period of q15 min standard monitoring for the first 2 hours.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: COVID-19, Awake proning, intubation (PubMed Search)
Posted: 1/12/2021 by Quincy Tran, MD, PhD
(Updated: 2/8/2026)
Click here to contact Quincy Tran, MD, PhD
A single center (Nebraska, USA), retrospective analysis investigated the prevalence of intubation during hospital stay for 105 patients who had COVID-19 between March 24 to May 5, 2020 (1). 40 patients underwent awake proning vs. 60 patients did not undergo awake proning.
After adjusting for either SOFA or APACHE scores, patients with awake proning were associated with lower Hazard Ratios of intubation for SOFA (HR 0.30, 95% CI 0.09-0.96, p=0.043) and APACHE (HR 0.30, 95%CI 0.1-0.91, p=0.034).
Discussion
While this US study seemed promising, another Brazilian study being published earlier in July 2020 showed no difference in the prevalence of intubation between COVID-19 patients with proning or without proning (2).
These 2 studies highlighted the nature of this disease: high practice variability, uncertainty of therapeutic modalities. However, the complications from awake proning had been very low.
Conclusion:
Awake proning for hypoxic COVID-19 patients is a promising intervention but we will need more studies. In the meanwhile, we can try this therapeutic modality as the risk is low.
Category: Orthopedics
Keywords: tendon, antibiotics (PubMed Search)
Posted: 1/9/2021 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
A recent retrospective observational study looked at the association of oral antibiotics (primarily fluroquinolones) and tendon rupture.
Outcome data is very interesting for our practice, deviates from traditional teaching.
Population: 1 million Medicare fee for service beneficiaries from 2007-2016 (>65 years old)
Antibiotics queried: Seven total oral antibiotics of mixed class:
Outcome measures: all combined tendon ruptures and 3 by anatomic site (Achilles, rotator cuff {RC} and other)
Results: Of the 3 quinolones, only LEVOfloxacin showed a significant increase in risk of tendon rupture (16% for RC) and (120% for Achilles) in a 1 month window. The others did not show an increased risk
Among the other antibiotics, cephalexin showed an increase risk across all anatomic sites.
The authors note that the risk with levofloxacin never exceeded the risk of cephalexin in any comparison!
Baik S, Lau J, Huser V, McDonald CJ. Association between tendon ruptures and use of fluoroquinolone, and other oral antibiotics: a 10-year retrospective study of 1 million US senior Medicare beneficiaries.
BMJ Open. 2020;10(12):e034844. Published 2020 Dec 21.
Category: Critical Care
Posted: 1/6/2021 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Study Question: What is the association of relative hypotension (degree and duration of MPP deficit) in patients with vasopressor-dependent shock with the incidence of new significant AKI and major adverse kidney events (MAKE)?
Methods:
Results:
Take-aways:
Panwar R, Tarvade S, Lanyon N, et al. Relative hypotension and adverse kidney-related outcomes among critically ill patients with shock. A multicenter, prospective cohort study. Am J Respir Crit Care Med. 2020;202(10):1407-1418.
Category: Pharmacology & Therapeutics
Keywords: Octreotide, Vasopressin, Variceal Bleeding (PubMed Search)
Posted: 1/2/2021 by Wesley Oliver
Click here to contact Wesley Oliver
With a national shortage of octreotide an alternative treatment plan had to be implemented at our institution for patients presenting with variceal bleeding.
Drug references recommend a continuous infusion of vasopressin at 0.2 to 0.4 units/minute. Dose may be titrated as needed to a maximum dose of 0.8 units/minute with maximum duration of 24 hours to reduce incidence of adverse effects. Administer IV nitroglycerin concurrently to prevent ischemic complications and monitor closely for signs/symptoms of myocardial, peripheral, and bowel ischemia.
Protocol at our institution:
Vasopressin
Initiate vasopressin at 0.2 units/min.
Increase by 0.2 units/min if bleeding is not controlled after one hour (max dose: 0.8 units/min).
If bleeding controlled for 2 hours, can decrease by 0.2 units/min and reassess.
Limit use to 24 hours.
Nitroglycerin
Use nitroglycerin infusion to prevent adverse effects from vasopressin.
Initiate nitroglycerin at 40 mcg/min, titrate by 40 mcg/min to a max dose of 400 mcg/min.
Goal systolic blood press pressure of 90-100 mmHg. Do not start nitroglycerin if SBP <90 mmHg.
***Please note the vasopressin dose for this indication is significantly higher than the typical dose of 0.03 units/min we use for shock.***
Garcia-Tsao G, Abraldes JG, Berzigotti A, Bosch J. Portal hypertensive bleeding in cirrhosis: risk stratification, diagnosis, and management: 2016 practice guidance by the American Association for the Study of Liver Diseases [published correction appears in Hepatology. 2017;66(1):304]. Hepatology. 2017;65(1):310-335.
Terés J, Planas R, Panes J, Salmeron JM, Mas A, Bosch J, Llorente C, Viver J, Feu F, Rodés J. Vasopressin/nitroglycerin infusion vs. esophageal tamponade in the treatment of acute variceal bleeding: a randomized controlled trial. Hepatology. 1990 Jun;11(6):964-8.
Vasopressin. Lexicomp. UpToDate. Waltham, MA: UpToDate Inc. Available at: https://www.uptodate.com. Accessed on December 31, 2020.
