Category: Critical Care
Keywords: dexamethasone, steroids, respiratory failure, COVID-19, SARS-CoV-2, RECOVERY (PubMed Search)
Posted: 7/14/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
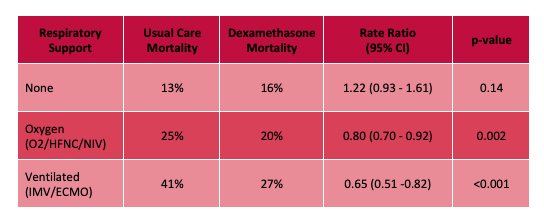
The RECOVERY (Randomized Evaluation of COVid-19 thERapY) investigators recently published a non-peer reviewed article on their findings utilizing dexamethasone to treat patients with COVID-19.
Rx: Dexamethasone 6mg daily* x 10 days (PO or IV) *or steroid equivalent
Primary outcome: All-cause mortality at 28-days
Secondary outcomes:
Results:
Limitations:
Bottom Line: Strongly consider admininstering dexamethasone to your patients with known COVID-19 who require respiratory support, and look for the peer-reviewed publication from the RECOVERY Trial investigators.
Horby P, Lim WS, Emberson et al. Effect of Dexamethasone in Hospitalized Patients with COVID-19: Preliminary Report. https://www.medrxiv.org/content/10.1101/2020.06.22.20137273v1 (Accessed July 14th, 2020)
Category: Orthopedics
Keywords: carpal tunnel syndrome, neuropathy, (PubMed Search)
Posted: 7/11/2020 by Brian Corwell, MD
(Updated: 2/9/2026)
Click here to contact Brian Corwell, MD
Treatment for carpal tunnel syndrome (CTS)
The management of CTS depends of the severity of the disease
If symptoms or on the mild to moderate range, a trial of conservative treatment is encouraged.
Possible therapeutic approaches can include splinting in wrist neutral position. Some even extend to keep the CMP joints extended. Extreme flexion and extension can increase pressure within the carpal tunnel. Usually for nighttime use only. May be used during day based on work and activity demands.
Has been shown to improve electrophysiologic findings after 12 weeks of use in moderate CTS.
Formal hand physical therapy (by an experienced therapist) may also be of some benefit including carpal bone mobilization, ultrasound and nerve glide exercises.
There is small evidence for the benefit of prednisone (20mg/d) as it has been shown to be more effective than placebo with improvements lasting an average of 8 weeks.
There is no benefit to NSAIDs or diuretics.
There is poor evidence for therapeutic ultrasound and acupuncture.
While more invasive than the above modalities, steroid injections may decrease inflammation and pressure in the carpal tunnel. Patients randomized to steroid injection may do better than those randomized to nighttime splinting.
Early referral in those with positive electrodiagnostic findings is encouraged as they do best with earlier surgical release and have better recovery.
If however the patient has severe, progressive or persistent symptoms or there is known evidence of nerve injury on diagnostic testing, referral for surgical decompression is warranted.
Category: Toxicology
Posted: 7/9/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
What is the name of the toxin found in this seed/bean and its mechanism of toxicity?

Name: Jequirity bean or rosary pea (Abrius precatorius)
Toxin: Abrin (toxalbumin)
Mechanism of toxicity:
Exposure
Signs and symptoms of toxicity:
Treatment:
Category: Neurology
Keywords: idiopathic intracranial hypertension, papilledema, intracranial pressure, cranial nerve palsy (PubMed Search)
Posted: 7/8/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Idiopathic intracranial hypertension (IIH) is a vision-threatening illness with significant morbidity and needs to be considered as a possible headache diagnosis in the ED. Most often, this occurs in women of childbearing age with a BMI >30, but atypical varieties exist.
Symptoms: Headache (90%), visual disturbance, pulsatile tinnitus, horizotal diplopia.
Signs: Papilledema, 6th cranial nerve (abducens) palsy.
Evaluation: Neuroimaging including CTV or MRV to identify alternate cause including cerebral venous outflow obstruction, lumbar puncture with opening pressure >30 cmH2O (25-30 cmH2O is gray zone), blood work per clinical presentation, CSF analysis.
Treatment: No clear consensus, but typically acetazolamide. Severe or refractory symptoms may require surgical intervention such as optic nerve sheath fenestration, VP shunt, venous sinus stenting.
Hoffmann J, Mollan SP, Paemeleire K, et al. European Headache Federation guideline on idiopathic intracranial hypertension. J Headache Pain. 2018;19(1):93.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: Contrast induced nephropathy; acute kidney injury; consensus statement (PubMed Search)
Posted: 7/7/2020 by Kim Boswell, MD
Click here to contact Kim Boswell, MD
We all know the frustration that comes with the phone call from radiology asking if you “really want IV contrast” for your patient’s CT because the creatinine is elevated…
Recently, a joint statement was published between the American College of Radiology and the National Kidney Foundation regarding the safety of IV contrast in patients with kidney disease. The recommendations are based on GFR and apply to those with both chronic kidney disease as well as those who have an acute kidney injury. Summary points of the statement are below:
Every decision to use contrast should be made based on clinical need for contrast as well as individual patient risk factors and underlying disease processes.
Use of Intravenous Iodinated Contrast Media in Patients With Kidney Disease: Consensus Statements From the American College of Radiology and the National Kidney Foundation. Radiology. 2020 Mar;294(3):660-668. doi: 10.1148/radiol.2019192094. Epub 2020 Jan 21.
Category: Pharmacology & Therapeutics
Keywords: opioid, renal failure, dialysis (PubMed Search)
Posted: 7/6/2020 by Ashley Martinelli
(Updated: 2/9/2026)
Click here to contact Ashley Martinelli
Pain management can be challenging in patients with acute or chronic renal failure. Opioid medications should always be used with caution, but some are safer than others. Morphine and codeine specifically should be avoided in these patients due to accumulation of active metabolites that can prolong the duration of effect and adverse events.
| Opioid | Renal Failure Impacts | Renal Failure Recommendation | Dialysis Recommendation |
| Morphine | Active metabolites accumulate | | |
| Codeine | Active metabolites accumulate | | |
| Hydromorphone | Minimal active metabolites | | |
| Oxycodone | Minimal active metabolites | | |
| Fentanyl | No active metabolites | | |
| Methadone | Active metabolites are inactive | | |
Dean M. Opioids in renal failure and dialysis patients. J Pain Symptom Mange 2004;28:497-504.
Category: Pediatrics
Posted: 7/3/2020 by Cathya Olivas Michels, MD
Click here to contact Cathya Olivas Michels, MD
Every year, numerous children die of non-exertional heatstroke after being left in motor vehicles in the United States. Per data obtained from the national nonprofit KidsAndCars.org, the average number of pediatric vehicular heatstroke deaths is 39 per year since 1990. In 2018, this number peaked at 54 pediatric deaths. Prior studies show that the interior temperature of a closed vehicle rises quickly within minutes of closing the doors and windows. This rapid change occurs even on days with cooler ambient temperatures (20s °C/70s °F): the interior temperature of a car may still reach 117F within an hour.
Children, particularly infants and toddlers, are at increased risk for heat illness due to several physiologic and developmental factors:
- Unable to escape hot environments or to self-hydrate
- Lack mature thermoregulatory systems
o Have lower rate of sweat production than adults
- Have higher basal metabolic rates than adults
- Have higher body surface area:mass ratio --> absorb heat faster in hot environments
Bottom line: ED providers can be instrumental in giving anticipatory guidance on vehicular heatstroke in children during the warmer seasons:
- Educate caregivers to “Look before you Lock”
- Suggest that the caregiver place a valuable object (phone, employee badge, handbag) in the back seat when traveling with a child
- Remind caregiver of the dangers of intentionally leaving a child in the car for any reason, even during cooler spring/summer days.
A recent retrospective cohort study (Hammett et al.) of 554 pediatric victims (aged <14 years) who died of heatstroke in a motor vehicle was conducted using KidsAndCars.org data. This study is the largest to date to describe this US subset of pediatric fatalities.
Results:
- Nearly half of the cases occurred when the ambient temperature was >90°F. However, 10% cases occurred when the ambient temperature was < 80°F.
- Most incident cases (~40%) occurred in home parking areas > nonresidential parking areas> daycare centers parking.
- The mean victim age was 16.4 months. Most (99%) victims were less than 5 years of age.
- Male children were more common victims (54% cases) than female children.
- Most victims (78%) were left unknowingly in vehicles by their caregivers. For those victims left intentionally in vehicles, caregivers’ reasons for leaving the child in the vehicle were the caregivers’ need to attend work or school or desire to allow the child to keep sleeping.
- A single caregiver was most commonly responsible for leaving the child in the vehicle (89% cases), with the victim’s mother being the most often responsible.
https://www.kidsandcars.org/wp-content/uploads/2020/01/Heatstroke-fact-sheet.pdf
Hammett, D. L., Kennedy, T. M., Selbst, S. M., Rollins, A. & Fennell, J. E. Pediatric Heatstroke Fatalities Caused by Being Left in Motor Vehicles. Pediatric Emergency Care, (2020).
Category: Critical Care
Keywords: Neutrophils, Lymphocytes, NLR, ANC, ALC, Sepsis, COVID (PubMed Search)
Posted: 6/30/2020 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
As has been previously noted, the white blood cell count is "the last refuge of the intellectually destitute." However, within a CBC (especially if a differential is obtained), there is information that can sometimes be of value. One measure, which was noted before COVID but has come under increasing attention in the current pandemic, is the Neutrophil-To-Lypmhocyte Ratio (NLR). Because physiologic stress typically causes the Absolute Neutrophil Count (ANC) to increase and the Absolute Lymphocyte Count (ALC) to decrease, the ratio of the two values (NLR = ANC/ALC) should increase when the body is under stress. Similar to the WBC however, it should be noted that ANY source of physiologic stress can cause abnormalities of the NLR, and thus this is not limited strictly to infectious etiologies.
With that caveat in mind, the NLR can sometimes be a clue to the degree of physiologic stress the patient is under. As lymphopenia is a frequent finding in COVID, the NLR has come under particular interest in the setting of COVID and appears to have prognostic value in COVID+ patients.
It should be kept in mind that inflammatory stressors (e.g. sepsis) are likely to disproportionately raise the NLR relative to noninflammatory stressors (e.g. pulmonary embolism), so a septic patient with an NLR of 10 might not be all that ill, whereas a PE patient with an NLR of 10 may be sicker. As with any single lab, and particularly one so nonspecific, there are no hard and fast cutoffs, and the NLR has to be interpreted in the context of other clinical data (it is very much possible to have a high NLR and not be that sick, or to have a low NLR and be sick... this is only one datapoint and does have pitfalls associated with it). As a rough guide however, a Pulmcrit post by Josh Farkas from 2019 suggested the following interpretation of the NLR:
1-3: Normal
6-9: Mild stress (e.g. uncomplicated appendicitis)
9-18: Moderate stress, may be associated with critical illness
>18: Severe stress, commonly associated with critical illness
The post (see references below) provides an excellent overview of NLR, further information on the uses and pitfalls of NLR, and several additional sources on the subject. It's a very worthwhile read.
Bottom Line: The Neutrophil-To-Lymphocyte Ratio (NLR = ANC/ALC) is one indicator of the degree of physiologic stress, and may be used in conjuction with other clues to determine how sick your patient is.
Category: Toxicology
Keywords: Carbon monoxide poisoning, PE, DVT (PubMed Search)
Posted: 6/25/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Carbon monoxide is an odorless gas that can cause neurologic and cardiovascular toxicity. It is produce by combustion of organic materials/fuel such as natural gas (furnace, gas stove, water heater, space heater) or gasoline. DVT/PE has been reported among victims of CO poisoning.
A recently published article investigated the risk of DVT/PE after CO poisoning.
Results
22,699 patients with CO poisoning were identified between 2004 and 2015
30 days after CO poisoning
90 days after CO poisoning
No significant increase in risk > 90 days.
Conclusion
Cho Y et al. Risk of venous thromboembolism after carbon monoxide poisoning: a nationwide population-based study. Ann of Emerg Med. 2020;75:587-596.
Category: Critical Care
Keywords: ICH, stroke, hemorrhagic, platelet, DDAVP, desmopressin (PubMed Search)
Posted: 6/23/2020 by Robert Brown, MD
Click here to contact Robert Brown, MD
Mortality is high in intracranial hemorrhage, and even higher for anti-platelet associated ICH (AP-ICH). The Platelet Transfusion Versus Standard Care After Acute Stroke Due to Spontaneous Cerebral Hemorrhage Associated with Antiplatelet Therapy (PATCH) trial was shocking: it demonstrated platelet transfusion was associated with worse outcomes, excluding those patients who were planned to go to surgery in the next 24 hours. SCCM and the Neurocritical Care Society recommend AGAINST platelet transfusion in non-operative ICH, but encourage a dose of DDAVP.
But who knows who will go to surgery? If you've been giving platelets and DDAVP to non-operative AP-ICH, you're not alone. So in the July Issue of Crit Care Medicine, the authors of the PATCH trial published a retrospective study of 140 patients, excluding those who immediately had surgery. In this group in which a quarter eventually had decompressive craniectomy and a fifth had an external ventricular drain placed, half received platelets and DDAVP instead of DDAVP alone.
The result? Still no benefit to platelet transfusion (despite the inclusion of patients who went on to have surgery). We all WANT to give platelets to AP-ICH, but there is NO evidence of BENEFIT and we may cause HARM. A test of platelet function (like the TEG) should be performed at the very least to select for patients with actual platelet dysfunction, and transfusion should be limited to patients going to surgery.
Mengel A, Stefanou M, Hadaschik K, et al. Early Administration of Desmopressin and Platelet Transfusion for Reducing Hematoma Expansion in Patients With Acute Antiplatelet Therapy Associated Intracerebral Hemorrhage. Crit Care Med 2020; 48:1009-1017
Baharoglu M, Cordonnier C, Al-Shahi R, et al. Platelet transfusion versus standard care after acute stroke due to spontaneous cerebral haemorrhage associated with antiplatelet therapy (PATCH): A randomised, open-label, phase 3 trial. Lancet 2016; 387:2605-2613
Frontera J, Lewin J, Rabinstein A, et al. Guideline for reversal of antithrombotics in intracranial hemorrhage: A statement for healthcare professionals from the Neurocritical Care Society and Society of Critical Care Medicine. Neurocrit Care 2016; 24:6-46
Category: Infectious Disease
Keywords: HIV, Medications (PubMed Search)
Posted: 6/20/2020 by Michael Bond, MD
(Updated: 6/21/2020)
Click here to contact Michael Bond, MD
Category: Pediatrics
Keywords: weight loss, not eating, small, FTT (PubMed Search)
Posted: 6/19/2020 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Calleo V, Surujdeo R and Thabet A. Emergency Department Management of Patients with Failure to Thrive. EB Medicine. March 2020.
Category: Critical Care
Posted: 6/16/2020 by Mike Winters, MBA, MD
(Updated: 2/9/2026)
Click here to contact Mike Winters, MBA, MD
Analgesics & Sedatives in the Critically Ill Obese Patient
Erstad BL, Barletta JF. Drug dosing in the critically ill obese patient - a focus on sedation, analgesia, and delirium. Crit Care. 2020; 24:315.
Category: Orthopedics
Keywords: Sickle cell trait, exertional death (PubMed Search)
Posted: 6/13/2020 by Brian Corwell, MD
(Updated: 2/9/2026)
Click here to contact Brian Corwell, MD
Sickle cell trait (SCT) is common and often overlooked clinically
-7.3% African Americans
-0.7% Hispanics
-0.3% Caucasians
SCT is a leading cause of exertional death in athletes who play football
The exact mechanism is unknown but likely involves a combination of high intensity exercise, dehydration, heat strain and inadequate opportunity for cardiovascular recovery leading to microvascular erythrocyte sickling.
This leads to hypoxia, cell death, hyperkalemia, and death from arrhythmia.
Presentation often involves rhabdomyolysis and exertional collapse.
In August of 2010 the NCAA enacted legislation requiring documentation of SCT status of all Division 1 athletes (2012 for Division 2 and 2014 for Division 3)
They also mandated education, counseling and issued guidelines for proper conditioning
Sudden death in athletes with SCT was first observed in military recruits in 1970.
Death in African American military recruits was 28 times more likely in those with SCT than in those without.
A 2012 study of football athletes found the risk of exertional death to be 37 times higher in athletes with SCT than in those without.
Despite game/competition situations being more intense, deaths occur almost exclusively during practice and conditioning drills.
Following the 2010 legislation, there has been a 89% decrease in death from SCT in NCAA D1 football.
Workout plans need to account for heat/humidity, the athletes level of conditioning and allow for adequate rest, recovery, hydration. SCT screening is only part of the solution.
Buchanan et al., 2020. Sudden Death Associated With Sickle Cell Trait Before and After Mandatory Screening. Sports Health.
Category: Toxicology
Keywords: hydroxychloroquine toxicity, overdose (PubMed Search)
Posted: 6/11/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
A 27 year-old man with history of rheumatoid arthritis presents to the emergency department after ingestion of hydroxychloroquine (20 tablets of 200 mg/tablet). He complains of nausea/vomiting. He appears lethargic. What is the anticipated hydroxychloroquine toxicity and management?
VS: Temp: afebrile, BP: 95/55 mmHg, RR: 23 breaths/min, O2 saturation: 99%
ECG:
Signs and symptoms of hydroxychloroquine toxicity includes:
Patient’s initial ECG showed: QRS: 134 msec; QTc 710 msec. There is also a terminal R wave in aVR. no prior ECG was available.
He experienced intermittent non-sustained V tach.
K was 2.0 mmol/L. other laboratories were normal
Management/course:
ED/Hospital day 1:
Hospital day 2:
Summary
Chai PR et al. Intentional hydroxychloroquine overdose treated with high-dose diazepam: an increasing concern in the COVID-19 pandemic. J Med Toxicol. 2020 PMID: 32514696; PMCID: PMC7278768; DOI: 10.1007/s13181-020-00790-8
Category: Neurology
Keywords: pregnancy, postpartum, migraine, RCVS, CVT, Bell's Palsy, facial palsy (PubMed Search)
Posted: 6/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Pregnancy is associated with an increased risk for RCVS, CVT, and Bell’s Palsy. Pregnancy also affects the frequency of migraines due to hormonal fluctuations.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: Covid-19, hydroxychloroquine, prophylaxis (PubMed Search)
Posted: 6/9/2020 by Quincy Tran, MD, PhD
(Updated: 2/9/2026)
Click here to contact Quincy Tran, MD, PhD
Patient
· A North America multicenter study involving 821 asymptomatic patients who had exposure to Covid-19-positive patients. The study was double-blind, placebo-controlled randomized trial.
Intervention
· Within 4 days of exposure, participants were randomized to receive hydroxychloroquine. Dose of hydroxychloroquine was 800 mg once then 600 mg in 6-8 hours then 600 mg daily for 4 more days.
· There were 414 patients in this arm. Median age 41 years [IQR 33-51]
Comparison:
· Placebo treatment. There were 407 patients in this arm. Median age 40years [IQR 32-50]
Outcome:
· Incidence of either laboratory-confirmed Covid-19 or Covid-19 symptoms within 14 days.
Results:
· 49 (11.8%) patients with treatment had Covid-19 findings (positive tests or symptoms)
· 58 (14.3%) patients with placebo had Covid-19 findings (p=0.35).
· The absolute difference was -2.4%. The number need to treat (NNT) to prevent one infection is 42 patients. Number needed to harm is 50 patients.
· Symptoms were fatigue (49.5%), cough (44.9%), sore throat (40.2%) myalgia (37.4%), fever (34.6%), anosmia (23.4%), shortness of breath (18.7%).
Conclusion:
Hydroxychloroquine prophylaxis did not prevent post-exposure Covid-19 infection.
A Randomized Trial of Hydroxychloroquine as Postexposure Prophylaxis for Covid-19.
Boulware DR, Pullen MF, Bangdiwala AS, Pastick KA, Lofgren SM, Okafor EC, Skipper CP, Nascene AA, Nicol MR, Abassi M, Engen NW, Cheng MP, LaBar D, Lother SA, MacKenzie LJ, Drobot G, Marten N, Zarychanski R, Kelly LE, Schwartz IS, McDonald EG, Rajasingham R, Lee TC, Hullsiek KH.
N Engl J Med. 2020 Jun 3. doi: 10.1056/NEJMoa2016638. Online ahead of print.
PMID: 32492293
Category: Pharmacology & Therapeutics
Keywords: Metronidazole, Disulfiram-like Reaction (PubMed Search)
Posted: 6/6/2020 by Wesley Oliver
Click here to contact Wesley Oliver
While taking metronidazole it is advised that patients avoid ethanol use for at least 3 days after therapy due to the possibility of a disulfiram-like reaction. The disulfiram-like reaction presents as abdominal cramps, nausea, vomiting, headaches, and/or flushing and can cause extreme discomfort for patients. A recent case report describes a case of a disulfiram-like reaction in a patient receiving metronidazole and an oral prednisone solution that contained 30% alcohol. This case highlights an important point. Not only should we counsel patients about avoiding alcoholic beverages for at least 3 days after metronidazole therapy, but they should also avoid all alcohol-containing products, such as oral solutions and mouthwash.
Category: Critical Care
Posted: 6/4/2020 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Clinical Question: Will resuscitation guided by dynamic assessments of fluid responsiveness in patients with septic shock improve patient outcomes?
Methodology:
Design: Randomized, unblinded clinical trial among adults with sepsis-associated hypotension comparing PLR-guided SV responsiveness as a guide for fluid management (intervention) versus “usual care” at 13 hospitals in the United States and the United Kingdom (randomization was in a 2:1 allocation of SV-guided to usual care).
Inclusion criteria:
-patients presenting to the ED with sepsis or septic shock and anticipated ICU admission.
-refractory hypotension (MAP ≤ 65mmHg after receiving ≥ 1L and < 3L of fluid)
Exclusion criteria:
-infusion of > 3L of IV fluid prior to randomization
-hemodynamic instability due to active hemorrhage
-pregnancy or being incarcerated
-indication for immediate surgery
-acute CVA, acute coronary syndrome, acute pulmonary edema, status asthmaticus, major cardiac arrhythmia, drug overdose, injury from burn or trauma, status epilepticus
-inability or contraindication to passive leg raising
Intervention (in ICU):
-PLRs were performed prior to any treatment of hypoperfusion with either fluid bolus or vasopressors for the first 72 hours after ICU admission or until ICU discharge (whichever occurred first)
-If patient was FR (increase in SV ≥10%) a 500 ml crystalloid fluid bolus was given with repeat PLRs after every fluid bolus
-If the patient was non-FR, initiation or up-titration of vasopressors was prompted with repeat PLRs after significant escalation (an increase of 1 mcg/kg/min norepinephrine)
Results:
-83 patients in Intervention arm, 41 in Usual Care arm
-Both arms received a similar volume of resuscitation fluid prior to enrollment (2.4 ± 0.6 L Intervention vs. 2.2 ± 0.7L Usual Care)
-Positive fluid balance at 72 hours or ICU discharge, was significantly less in the Intervention arm (-1.37L favoring Intervention, 0.65 ± 2.85L Median: 0.53L Intervention vs. 2.02 ± 3.44L Median: 1.22L Usual Care, p=0.02).
-Fewer patients required RRT (5.1% vs 17.5%, p=0.04) or MV in Intervention arm compared to Usual Care (17.7% vs 34.1%, p=0.04)
-ICU length of stay was similar in the two arms
-There was no difference in overall 30-day mortality (6.3% difference, Intervention: 15.7% vs. Usual Care: 22.0%, 95% CI -21.2%, 8.6%)
Implications:
Although this is a smaller, unblinded (also funded by maker of SV monitoring device) study, Douglas et al. demonstrate that limiting fluid administration using dynamic assessments of fluid responsiveness to guide resuscitation in patients in septic shock is likely safe. In fact, this may actually decrease the need for renal replacement therapy and mechanical ventilation amongst this patient population. At the very least, this study adds to the body of literature showing the harms of excessive fluid administration and positive fluid balance.
Bottom line:
If possible, use dynamic assessments of fluid responsiveness in patients with septic shock to guide interventions, particularly for further resuscitation beyond initial fluid resuscitation (~2 liters in this study).
Douglas IS, Alapat PM, Corl KA, et al. Fluid Response Evaluation in Sepsis Hypotension and Shock: A Randomized Clinical Trial. Chest. 2020
Category: Toxicology
Keywords: Riot control agent, Mace, pepper spray, tear gas (PubMed Search)
Posted: 6/4/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Over the past several days, riot control agents have been used against the protest participants (related to Mr. George Floyd’s death). There are 3 widely used riot control “lacrimating” agents:
These agents (irritants) primarily affect the eye, skin, and respiratory tract.
| Organ | Effect | Management |
| Eyes | · Lacrimination · Blepharospasm · Conjunctiva irritation/conjunctivitis · Periorbital edema · Corneal abrasions | · Copious H20/saline irrigation with Morgan Lensor Nasal Cannula jury-rig · Slit lamp exam for corneal abrasions |
| Skin | · Burning sensation · Blister · Contact dermatitis · 2nd degree burns (mace) | · Wash with soap and water · Wound care |
| Airway/respiratory tract | · Respiratory tract irritation · Rhinorrhea · Laryngospasm · Bronchospasm · Chemical pneumonitis | · B2-agonists for bronchospasm · Steroids if worsening underlying reactive airway disease · CXR to evaluate for possible pneumonitis · Supplementary oxygen as needed |
Mangement:
