Category: Orthopedics
Keywords: Concussion Incidence, epidemiology, (PubMed Search)
Posted: 10/26/2019 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
A recent epidemiology study in Pediatrics looked at concussions in 20 high school sports during the 2013–2014 to 2017–2018 school years.
For every athlete, one practice or competition was counted as one exposure.
Overall, 9542 concussions were reported for an overall rate of 4.17 per 10 000 athletic exposures (AEs).
Football continues to have the highest incidence with a concussion rate of 10.40 per 10 000 AEs.
As in previous studies, rates in competition (33.19 to 39.07 per 10 000 AEs) are increasing and higher than rates in practice which are lower and decreasing over the study period (5.47 to 4.44 per 10 000 AEs).
This may reflect better reporting or increasing injury rate
In all 20 sports, recurrent concussion rates decreased from 0.47 to 0.28 per 10 000 AEs.
Confirming prior studies, among sex-comparable sports, concussion rates were higher in girls than in boys (3.35 vs 1.51 per 10 000 AEs).
Also, among sex-comparable sports, girls had larger proportions of concussions that were recurrent than boys (9.3% vs 6.4%).
This study may reflect effective implementation of strategies to reduce concussion incidence such as mandatory removal from play and more stringent requirements associated with return to play.
Concussion Incidence and Trends in 20 High School Sports, Kerr et al., 2019, Pediatrics.
Category: Pediatrics
Keywords: lactated ringer, LR, normal saline, NS (PubMed Search)
Posted: 10/25/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Bottom line: Balance fluid resuscitation with LR was not associated with improved outcomes compared to NS and pediatric sepsis. Selective LR use necessitates a prospective trial to definitively determine comparative effects among crystalloids.
1. Weiss SL, Keele L, Balanmuth F, Vendetti N, Ross R, Fitzgerald JC, Gerber JS. Crystalloid Fluid Choice and Clinical Outcomes in Pediatric Sepsis: A Matched Retrospective Cohort Study. J Pdatr.207 Mar:182:304-310.
2. Balamuth F, Kittick M, McBride P, Woodford AL, Vestal N, Casper TC, Metheney M, Smith K, Atkin NJ, Baren JM, Dean JM, Kuppermann N, Weiss SL. Pragmatic Pediatric Trial of Balanced versus Normal Saline Fluid in Sepsis: The PRoMPT BOLUS Randomized Controlled Trial Pilot Feasibility Study. Acad Emerg Med. 2019 Jun 10
Category: Toxicology
Keywords: VA-ECMO, drug-induced cardiogenic shock (PubMed Search)
Posted: 10/24/2019 by Hong Kim, MD
Click here to contact Hong Kim, MD
Patients with drug-induced cardiogenic shock [DIC] (e.g. overdose of CCB/BB, membrane stabilizing agents, etc.) are often managed with medical interventions such as vasopressors, bicarbonate infusion, high-dose insulin, lipid emulsion therapy. A fraction of these patients may be refractory to the standard medical therapy. VA-ECMO (venoarterial extracorporeal membrane oxygenation) has been utilized in such situation; yet clinical experience of using VA-ECMO in DIC is limited.
A recent retrospective study of the Extracorporeal Life Support Organization’s ECMO registry showed
Conclusion
Clinical utility of venoarterial-extracorporeal membrane oxygenation (VA-ECMO) in patients with drug-induced cardiogenic shock: a retrospective study of the Extracorporeal Life Support Organizations’ ECMO case registry
Category: Neurology
Keywords: Cryptococcus neoformans, cryptococcosis, meningoencephalitis (PubMed Search)
Posted: 10/23/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: Consider cryptococcal meningitis even in immunocompetent patients.
Category: Airway Management
Keywords: PE, tachypnea, Critical Care, ED Disposition (PubMed Search)
Posted: 10/21/2019 by Robert Brown, MD
Click here to contact Robert Brown, MD
ICU admission rates for all acute PEs vary wildly across the country (<5% to ~80%).
To predict which hemodynamically stable, normotensive PE patients should be admitted to the ICU, a single-center retrospective analysis of 7 years’ data sought to describe the reasons why normotensive patients with PE required vasopressors within 48 hours of admission to the ICU. The authors studied 293 patients admitted to the ICU at Beth Israel Deaconess in Boston and found only 8 patients (2.7%) who decompensated within the first 2 days. Of MANY variables studied, only respiratory rate was significantly different between those who decompensated and those who did not (mean RR 29 with range 26-32 in the decompensated group vs mean 21 with range 17-24).
Bottom Line: cost control experts may lean on you to admit fewer PE patients to the ICU. There is no perfectly reliable way to predict which normotensive patient with a PE will decompensate. The PESI score has been validated but even the low risk cohort had 1.6% mortality at 3 days. The BOVA score has been validated but its endpoint of mortality at 30 days is less useful for planning admission. Tachypnea should concern you.
Admon A, Seymour C, Gershengorn H, et al. Hospital-level variation in ICU admission and critical care procedures for patients hospitalized for pulmonary embolism. Chest 2014; 146(6):1452-1461
Patel H, Shih J, Gardner R, et al. Hemodynamic decompensation in normotensive patients admitted to the ICU with pulmonary embolism. Journal of Critical Care 2019; 54:105-109
Category: Pediatrics
Keywords: sedation, autism spectrum disorder (PubMed Search)
Posted: 10/18/2019 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Brown et al. Procedural sedation in children with autism spectrum disorders in the emergency department. Am J Emerg Med. 2019 Aug;37(8):1404-1408.
Category: Critical Care
Posted: 10/15/2019 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
The Critically Ill Geriatric Patient with Sepsis
Khoujah D, et al. Resuscitating the critically ill geriatric emergency department patient. Emerg Med Clin N Am. 2019; 569-81.
Category: Orthopedics
Keywords: Playing surface, concussion (PubMed Search)
Posted: 10/12/2019 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Synthetic turf playing surfaces have been growing in popularity over the last decade and seem to have become a new standard.
Due to the need for durable fields that can accommodate multiple teams/activities, in addition to the high cost of maintaining grass and the need to conserve water, many parks and schools have switched from grass to turf. Turf is advertised as maintenance free but ….this is not the case.
Locally, at M&T Bank Stadium, groundskeepers drive a LitterKat turf sweeper across the field for 4 hours 2-3 times a week to ensure that the synthetic rubber is cleaned and distributed evenly. The field is also repainted every 4 games because the paint may become hard. The cost of this level of maintenance is beyond what many parks and local high schools can afford.
A recent study examined high school concussion data at almost 2000 high schools with over 14,000 recorded concussions. Researchers concluded that more concussions occurred in games than practices. Interestingly, they also found that playing surface was significantly associated with concussion. Almost 90% of all injuries occurred on turf-based surfaces. Turf outweighed all other mechanisms of injury, including helmet-to-helmet hits and grass playing surface. Between 10 and 15.5% of concussions occur from helmet to ground contact. In the NFL, this mechanism accounts for about 1 in 7 concussions.
Attempting to limit total exposure time in practice and games on turf surfaces may be beneficial until more study is needed.
Category: Toxicology
Keywords: suicide attempt, adolescent, young adults, epidemiological trend (PubMed Search)
Posted: 10/10/2019 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
The rate of suicide attempt has been increasing over the past decade. A recently published article investigated the temporal trend of suicide attempts in adolescent/young adult population (10 – 25 years old) from 2000 to 2018.
Methods
Results
Top 5 substance involved in suicide attempt
Agents associated with serious medical outcome (after 2011)
Conclusion
Spiller HA et al. Suicide attempts by self-poisoning in the United States among 10-25 year olds from 2000 to 2018: substances used, temporal changes and demographics. Clin Toxicol (Phila) 2019. Oct 6:1-12. doi: 10.1080/15563650.2019.1665182. [Epub ahead of print]
Category: Critical Care
Keywords: cardiac arrest, hypothermia, nonshockable rhythm (PubMed Search)
Posted: 10/8/2019 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Rationale: Data regarding temperature management in patients suffered from cardiac arrest with nonshockable rhythm was inconclusive.
Objective: whether moderate hypothermia at 33C, compared with normothermia at 37C would improve neurologic outcome in patients with coma after cardiac arrest with nonshockable rhythm.
Outcome: survival with favorable 90-day neurologic outcome (Cerebral Performance Category scale 1-2/5)
SummaryThere was higher percentage of patients achieving CPC 1-2 in the hypothermia group (10.2%) vs normothermia group (5.7%, Hazard Ratio 4.5, 95% CI 0.1-8.9, p=0.04)
This randomized multicenter trial involved 581 patients with cardiac arrest and nonshockable rhythm. Hypothermia group included 284 patients vs. 297 in the normothermia group. Median GCS at enrollment = 3.
Majority of patients was cooled with the use of a basic external cooling device: 37% for hypothermia and 50.8% for normothermia group.
There was higher percentage of patients achieving CPC 1-2 in the hypothermia group (10.2%) vs normothermia group (5.7%, Hazard Ratio 4.5, 95% CI 0.1-8.9, p=0.04)
Limitation:
A. The study used strict enrollment criteria:
B. normothermia group had higher proportion of patients with temperature at 38C.
C. Hypothermia group underwent temperature management of 56 hours vs. 48 hours for normothermia patients.
Take home points:
In a selected group of patients with cardiac arrest and nonshockable rhythm, moderate hypothermia at 33C may improve neurologic outcome.
Lascarrou JB, Merdji H, Le Gouge A, Colin G, Grillet G, Girardie P, Coupez E, Dequin PF, Cariou A, Boulain T, Brule N, Frat JP, Asfar P, Pichon N, Landais M, Plantefeve G, Quenot JP, Chakarian JC, Sirodot M, Legriel S, Letheulle J, Thevenin D, Desachy A, Delahaye A, Botoc V, Vimeux S, Martino F, Giraudeau B, Reignier J; CRICS-TRIGGERSEP Group.
Targeted Temperature Management for Cardiac Arrest with Nonshockable Rhythm.
N Engl J Med. 2019 Oct 2. doi: 10.1056/NEJMoa1906661. [Epub ahead of print]
Category: Toxicology
Keywords: e-cigarrette liquid exposure, National Poison Data System (PubMed Search)
Posted: 10/3/2019 by Hong Kim, MD
Click here to contact Hong Kim, MD
E-cigarette (vaping) use has become increasingly popular over the past 10 years, especially among adolescents. Intentional exposure (i.e. ingestion in self harm) of nicotine (e-cigarette liquid) can be life threatening where it can produce mixture of stimulatory (early), cholinergic toxicity and muscle paralysis/respiratory failure by blocking the neuromuscular junction. However, the severity of clinical toxicity in unintentional exposure can vary widely depending on the dose/route/circumstance of their exposure.
A recently published study investigated the characteristics of e-cigarette liquid exposure between Jan 1, 2010 to Dec 31, 2018 using the National Poison Data System
Result
Top 4 clinical/demographic characteristics are listed below.
Age group:
Route of exposure
Level of care:
Clinical effects - overall
In <5 years group
Conclusion
Category: Critical Care
Posted: 10/1/2019 by Caleb Chan, MD
(Updated: 2/7/2026)
Click here to contact Caleb Chan, MD
Blood Transfusion Thresholds in Specific Populations
Sepsis - 7 g/dL
Acute Coronary Syndrome - no current specific recommendations pending further studies
Stable Cardiovascular Disease - 8 g/dL
Gastrointestinal Bleeds
Acute Neurologic Injury - Traumatic Brain Injury - 7 g/dL
Postpartum Hemorrhage - 1:1:1 ratio strategy
Cable CA, Razavi SA, Roback JD, Murphy DJ. RBC Transfusion Strategies in the ICU: A Concise Review. Crit Care Med. 2019; epub ahead of print.
Category: Orthopedics
Keywords: Tenosynovitis, wrist pain (PubMed Search)
Posted: 9/28/2019 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Intersection Syndrome
De Quervain’s is a common tenosynovitis is involving the the 1st dorsal compartment of the wrist/forearm.
Intersection syndrome is a tenosynovitis that occurs at the intersection of the 1st and 2nd dorsal compartments.
Pathology located at crossing point of the 1st compartment structures (APL and EBP) with the radial wrist extensors (ECRB and ECRL)
Occurs most commonly from repetitive wrist extension and is common in rowers, weight lifters, and in those playing racquet sports.
Occurs about 4 to 6cm proximal to the radiocarpal joint VERSUS De Quervain’s which occurs near the level of the radial styloid.
Pain worse with resisted wrist and thumb extension
Radiographs not required
Splint and start NSAIDs
Recalcitrant cases can be referred for corticosteroid injection
https://stemcelldoc.files.wordpress.com/2012/09/intersection-syndrome-referral-pain-pattern1.jpg
Category: Neurology
Keywords: ACEP, SAH, imaging, nonopioid, CTA, LP (PubMed Search)
Posted: 9/25/2019 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Godwin SA, Cherkas DS, Panagos PD, et al. Clinical policy: critical issues in the evaluation and management of adult patients presenting to the emergency department with acute headache. Ann Emerg Med 2019;74(4):e41-74.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: VAPI, acute respiratory failure, vaping, e-cigarettes, e-hookah, juul, pulmonary disease, acute lung diease, ARDS (PubMed Search)
Posted: 9/23/2019 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
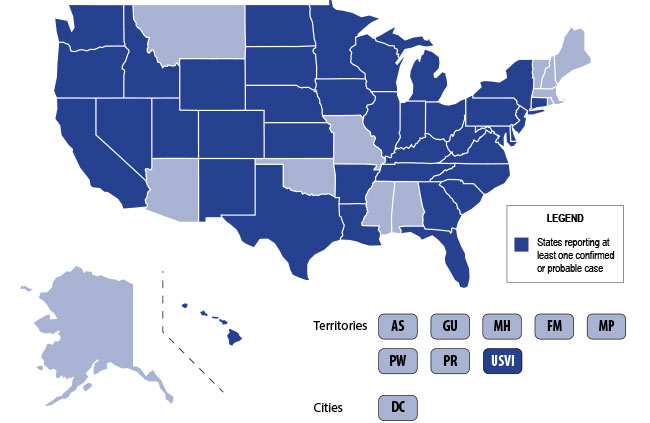
The U.S. is currently experiencing an epidemic of a severe lung disease termed Vaping-Associated Pulmonary Illness (VAPI), with over 500 cases and 7 deaths across 38 states and 1 U.S. territory since July 2019.
The clinical presentation of VAPI varies --
Diagnostics --
Treatment is supportive +/- steroids --
Bottom Line: Include vaping-associated pulmonary illness in your differential for patients presenting with acute lung disease.
Background: The use of electronic nicotine delivery systems, also known as e-cigarettes or vape pens, has risen precipitously since their introduction in 2006. They heat a liquid that can contain nicotine, THC/CBD, flavors and/or other additives, producing an aersol that is inhaled by users.
They have been marketed as a way to quit smoking, and as being safer than cigarettes. The U.S. is, however, currently experiencing an epidemic of a severe lung disesae termed Vaping-Associated Pulmonary Illness, with over 500 cases and 7 deaths across 38 states and 1 U.S. territory.
Per data obtained by the CDC:
CDC Emergency Preparedness & Response: "Severe Pulmonary Disease Associated with Using E-Cigarette Products" https://emergency.cdc.gov/han/han00421.asp
Category: Pediatrics
Keywords: Orthopedics, compartment syndrome (PubMed Search)
Posted: 9/20/2019 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
- Tibial tubercle avulsion fractures are rare and pediatrics, accounting for less than 3% of all epiphyseal injuries in children ages 11-17 years.
- The typical mechanism is a sudden forceful quadriceps contraction. Patients present with sudden pain after sprinting or jumping with pain, bruising, deformity or swelling over the tibial tubercle and with a decrease ability to extend the leg.
- 10 to 20% of cases result in anterior compartment syndrome related to the rupture of the anterior tibial recurrent artery.
- Although directly measured intra-compartmental pressures can facilitate the diagnosis of compartment syndrome, interpretation of these values can be challenging with healthy children having higher average lower leg compartment pressures than adults. Treatment of subsequent compartment syndrome is often based on a high index of suspicion.
Yue et al. Bilateral tibial tubercle avulsion fractures: Pediatric orthopedic injury at high risk for compartment syndrome. The American Journal of Emergency Medicine. Available online May 2019.
Category: Toxicology
Keywords: capsaicin, cannabinoid hyperemesis syndrome, marijuna use. (PubMed Search)
Posted: 9/19/2019 by Hong Kim, MD
Click here to contact Hong Kim, MD
Cannabinoid hyperemesis syndrome [CHS] (i.e. cyclic/recurrent nausea, vomiting and abdominal pain) is associated with long-term and frequent use of marijuana. Patients with CHS often report temporary relief of symptoms with hot water/shower exposure. Emergency room providers may encounter a growing number of patients with CHS with increasing legalization of marijuana-containing products.
Topical capsaicin has been gaining interest as a potential adjunct to the conventional management of patients with CHS (e.g. antiemetics, opioids, benzodiazepines and antipsychotics).
A small retrospective study was performed involving 43 patients who had multiple visits, and were treated with and without capsaicin. The primary outcome was the ED length of stay (LOS).
Results
Conclusion
Wagner S et al. Efficacy and safety of topical capsaicin for cannabinoid hyperemesis syndrome in the emergency department. Clin Toxicol (Phila) 2019. Sep 4:1-5. doi: 10.1080/15563650.2019.1660783. [Epub ahead of print]
Category: Critical Care
Keywords: Pregnant, difficult airway (PubMed Search)
Posted: 9/17/2019 by Kim Boswell, MD
Click here to contact Kim Boswell, MD
Most non-OB physicians experience some fear or anxiety over taking care of the average pregnant patient. There are two patients to consider when caring for these women. Critical illness adds another layer of complexity to an already challenging patient population. Due to the normal physiologic changes that occur during pregnancy there are specific and important factors to be aware of when considering and preparing for intubation.
Djabatey EA, Barclay PM. Difficult and failed intubationin 3430 obstetric general anesthesics. Anaesthesia 2009;64: 1168.
Izci B, Vennelle M, Liston WA, et al. Sleep-disordered breathing and upper airway size in pregnancy and post part. Our Respir J 2006; 27:321.
Lebowitz PW, Shay H, Straker T, et al. Shoulder and head elevation improves laryngoscope view for tracheal intubation in non obese as well as obese individuals. J Clin Anesth 2012; 24:104.
Category: Orthopedics
Keywords: foot fracture, radiology (PubMed Search)
Posted: 9/14/2019 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Imaging of Lisfranc Injuries
Tarsometatarsal fracture-dislocation
Anatomy
3 Columns of the midfoot, divided by the tarsometatarsal joints
The Lisfranc ligament
- Extends from the 2nd MT to the medial cuneiform
- Critical to structure and stabilization of the 2nd MT and the midfoot arch
Imaging
Plain films: AP/lateral/oblique
Consider weight bearing view with contralateral comparison if high suspicion
CT: Can be useful to confirm abnormal plain films
MRI: not done in ED but can be used to diagnose pure ligament injuries
Below is a review of the lines of the foot which will ensure not missing this diagnosis. May be helpful to review with sample imaging.
Plain films findings: https://prod-images.static.radiopaedia.org/images/49189279/86408d5bae08ab80ae9ef377337ab7_big_gallery.jpeg
On AP view:
On Lateral view:
On the Oblique view:
Remember that the lateral margin of the 5th MT can project lateral to the cuboid (up to 3 mm)
Lines drawn on 2 view foot for review
https://radiopaedia.org/cases/lisfranc-ligament-normal-alignment
Orthobullets.org
Category: Pediatrics
Keywords: UTIcalc, SBI, serious bacterial infection, febrile infant, urinary tract infection (PubMed Search)
Posted: 9/13/2019 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Question: In febrile children younger than 2 years, what combination of clinical and laboratory variables best predicts the probability of a urinary tract infection?
Given that urinary tract infections (UTI) are the most common source of serious or invasive bacterial infections in young febrile infants, early identification and treatment has the potential to reduce poor outcomes. Wouldn't it be great if there was an easy way to identify patients at highest risk?
Researchers from the Children’s Hospital of Pittsburgh formulated a calculator (UTICalc) that first estimates the probability of urinary tract infection (UTI) based on clinical variables and then updates that probability based on laboratory results.
Bottom line:
The UTICalc calculator can be used to guide to tailor testing and treatment in children with suspected urinary tract infection with the hope of improving outcomes for children with UTI by reducing the number of treatment delays.
Go ahead and give it a click!! https://uticalc.pitt.edu/
Shaikh N, Hoberman A, Hum SW, Alberty A, Muniz G, Kurs-Lasky M, Landsittel D, Shope T. Development and Validation of a Calculator for Estimating the Probability of Urinary Tract Infection in Young Febrile Children. JAMA Pediatr. 2018 Jun 1;172(6):550-556.
