Category: Neurology
Keywords: cerebral venous thrombosis, CVT, prothrombotic, headache (PubMed Search)
Posted: 9/10/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: The incidence of CVT is increasing with rate of increase higher in males and older females. Consider CVT beyond traditional risk factors.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: resuscitation, ultrasound, VExUS, venous congestion (PubMed Search)
Posted: 9/8/2020 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
While the invasive monitoring of central venous pressure (CVP) in the critically ill septic patient has gone the way of also transfusing them to a hemoglobin of 10 mg/dL, it remains that an elevated CVP is associated with higher mortality1,2 and renal failure.2,3
Extrapolating from existing data looking at hepatic vein, portal vein, and renal vein pulsatility as measures of systemic venous hypertension and congestion,4,5,6 Beaubien-Souligny et al. developed the venous excess ultrasound (VExUS) grading system incorporating assessment of all 3, plus the IVC, using US to stage severity of venous congestion in post-cardiac surgery patients.7 They evaluated several variations, determining that the VExUS-C grading system was most predictive of subsequent renal dysfunction.
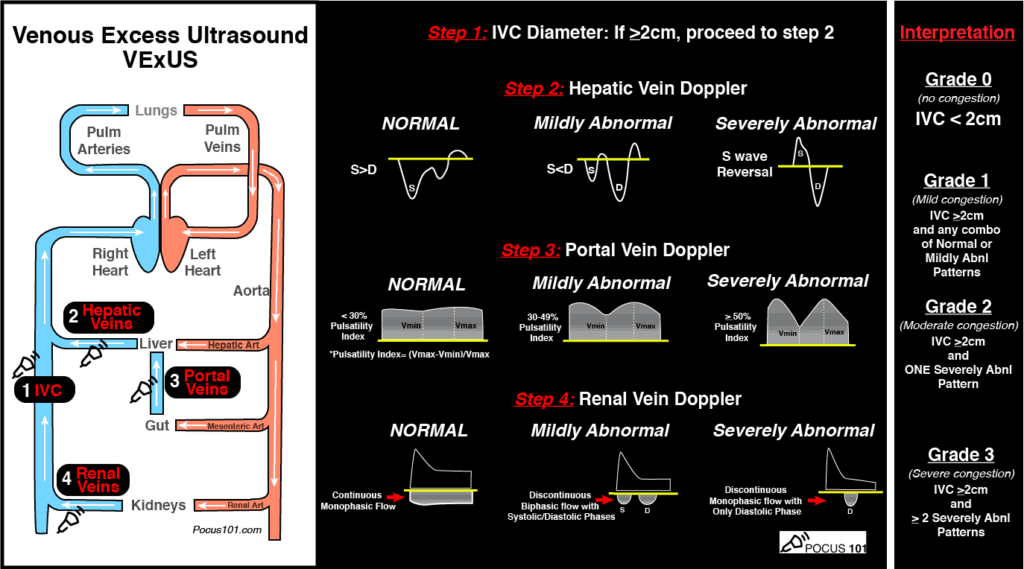
(Image from www.pocus101.com)
High Points
VExUS Grade 3 (severe) venous congestion:
Caveats
Clinical Uses
A great how-to can be found here:
https://www.pocus101.com/vexus-ultrasound-score-fluid-overload-and-venous-congestion-assessment/
1. Li DK, Wang XT, Liu DW. Association between elevated central venous pressure and outcomes in critically ill patients. Ann Intensive Care. 2017;7(1):83. doi:10.1186/s13613-017-0306-1
2. Chen KP, Cavender S, Lee J, et al. Peripheral Edema, Central Venous Pressure, and Risk of AKI in Critical Illness. Clin J Am Soc Nephrol. 2016;11(4):602-608.
3. Chen CY, Zhou Y, Wang P, Qi EY, Gu WJ. Elevated central venous pressure is associated with increased mortality and acute kidney injury in critically ill patients: a meta-analysis. Crit Care. 2020;24(1):80. doi:10.1186/s13054-020-2770-5
4. Iida N, Seo Y, Sai S, et al. Clinical Implications of Intrarenal Hemodynamic Evaluation by Doppler Ultrasonography in Heart Failure. JACC Heart Fail. 2016;4(8):674-682. doi:10.1016/j.jchf.2016.03.016
5. Ikeda Y, Ishii S, Yazaki M, et al. Portal congestion and intestinal edema in hospitalized patients with heart failure. Heart Vessels. 2018;33(7):740-751. doi:10.1007/s00380-018-1117-5.
6. Beaubien-Souligny W, Benkreira A, Robillard P, et al. Alterations in Portal Vein Flow and Intrarenal Venous Flow Are Associated With Acute Kidney Injury After Cardiac Surgery: A Prospective Observational Cohort Study. J Am Heart Assoc. 2018;7(19):e009961. doi:10.1161/JAHA.118.009961
7. Beaubien-Souligny W, Rola P, Haycock K, et al. Quantifying systemic congestion with Point-Of-Care ultrasound: development of the venous excess ultrasound grading system. Ultrasound J. 2020;12(1):16. doi:10.1186/s13089-020-00163-w
Category: Pharmacology & Therapeutics
Keywords: esmolol, cardiac arrest, ventricular tachycardia, ventricular fibrillation (PubMed Search)
Posted: 9/5/2020 by Ashley Martinelli
(Updated: 2/8/2026)
Click here to contact Ashley Martinelli
| | Beta-blockade N=22 | Control N= 44 | OR/CI |
| Temporary ROSC, n (%) | 19 (86.4) | 14 (31.8) | OR 14.46, 95% CI 3.63-57.57 |
| Sustained ROSC, n (%) | 13 (59.1) | 10 (22.7) | OR 5.76, 95% CI 1.79-18.52 |
| Survival with neurological function, n (%) | 6 (27.3) | 4 (9.1) | OR 4.42; 95% CI 1.05-18.56 |
Category: Pediatrics
Keywords: button battery, pediatrics, esophageal injuries (PubMed Search)
Posted: 9/4/2020 by Prianka Kandhal, MD
Click here to contact Prianka Kandhal, MD
Ingestion of a button battery is a can't-miss diagnosis with a very high risk for causing severe esophageal injury. There are about 3000 button battery ingestions per year, and this is increasing because electronics are becoming more and more prevalent.
Severe damage to the esophagus occurs within 2 hours. On your lateral view, the end with narrowing is the negative end, which triggers a hydrolysis reaction that results in an alkaline caustic injury and, ultimately, liquefactive necrosis.
Children can present with nonspecific symptoms and if the ingestion was not witnessed, they are at high risk for delays in diagnosis. Additionally, in the community setting, there can be further delays in definitive treatment (endoscopic removal) due to difficulty in calling teams in or transporting to other facilities.
Anfang et al. looked into ways to mitigate damage to esophageal tissue. They did an in vitro study on porcine esophageal tissue, measuring the pH with different substances applied. They tried apple juice, orange juice, gatorade, powerade, pure honey, pure maple syrup, and carafate. They then repeated the study in vivo on piglets with button batteries left in the esophagus and ultimately did gross and histological examination of the esophageal tissue.
Honey and carafate demonstrated protective effects both in vitro and in vivo. They neutralized pH changes, decreased full-thickness esophageal injury, and decreased outward extension of injury into deep muscle.
Take Home Point: If a child is found to have a button battery in the esophagus, while definitive management is still emergent endoscopic removal, early and frequent ingestion of honey (outside of the hospital) and Carafate (in the hospital) may help reduce the damage done to the tissue in the interim. The authors recommend 10ml every 10 minutes.
Anfang RR, Jatana KR, Linn RL, et al. pH-Neutralizing Esophageal Irrigations as a Novel Mitigation Strategy for Button Battery Injury. The Laryngoscope. 2019; 129:49-57.
Category: Critical Care
Keywords: Renal Replacement Therapy (PubMed Search)
Posted: 9/1/2020 by Kim Boswell, MD
(Updated: 2/8/2026)
Click here to contact Kim Boswell, MD
STARRT-AKITrial
The Standard versus Accelerated initiation of Renal Replacement Therapy in Acute Kidney Injury
The development of acute kidney injury (AKI) in the critical care setting portends a greater morbidity and mortality for patients. Additionally, it places the patient at high risk of complications and requires a greater use of resources. Several studies in the past have examined if the timing of initiation of renal replacement therapy (RRT) would result in a mortality benefit, but have failed to demonstrate consistent outcomes.
The STARRT-AKI trial was a multinational, randomized controlled trial designed to determine if early initiation of RRT in critically ill adult patients with AKI lowered the risk of 90-day mortality. The Kidney Disease Improving Global Outcomes (KDIGO) classification was used to define AKI and over 2900 patients were randomly assigned to two groups over a 4 year period. Exclusion criteria included: recent RRT, a renal transplant within the preceding year, advanced CKD, an overdose necessitating RRT, or a strong suspicion of obstruction or autoimmune/vascular cause of their AKI.
Groups:
Outcomes/Results:
Take home points:
Timing of Initiation of Renal-Replacement Therapy in Acute Kidney Injury. STARRT-AKI Investigators; Canadian Critical Care Trials Group, the Australian and New Zealand Intensive Care Society Clinical Trials Group, the United Kingdom Critical Care Research Group, the Canadian Nephrology Trials Network, and the Irish Critical Care Trials Group, Bagshaw SM, Wald R, Adhikari NKJ, et al. N Engl J Med. 2020 Jul 16;383(3):240-251.
Category: Neurology
Keywords: trigeminal neuralgia, TN, tic douloureux, neuropathic facial pain (PubMed Search)
Posted: 8/26/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
Bottom Line: New onset trigeminal neuralgia needs workup for its etiology. Carbamazepine and oxcarbazepine can be effective for symptom management though continuous or long-lasting pain exacerbations are difficult to treat.
Follow me on Twitter @EM_NCC
Category: Critical Care
Posted: 8/25/2020 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Ketamine In the Critically Ill Patient
Hurth KP, et al. The reemergence of ketamine for treatment in critically ill adults. Crit Care Med. 2020; 48:899-911.
Category: Orthopedics
Keywords: Elbow, fracture, ultrasound (PubMed Search)
Posted: 8/12/2020 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Diagnostic performance of Ultrasonography for detection of pediatric elbow fracture
Elbow fractures account for approximately 15% of pediatric fractures
Fat pads are traditionally taught as a marker of fracture
In a cadaveric study:
Elbow effusions of 1-3 mL could be identified with ultrasound
Elbow effusions of 5-10 mL could be identified with plain film
Pediatric plain films are sometimes challenging to obtain and interpret compared to adults
-More likely to be uncooperative in obtaining required views
-Non-ossified epiphyses
Ultrasound may be used to detect
-Cortical disruption and irregularity
-Growth plate widening
-Hematoma interposed between fracture fragments
-Elevated posterior fat pad
Absence of elbow fracture was indicated by
-Lack of cortical disruption
-Absence of posterior fat pad sign
Meta-analysis of 10 articles totaling 519 patients using ultrasonography to detect elbow fractures
Sensitivity 96%
Specificity 89%
False negative rate 3.7%
For comparison, plain radiographs
Interpreted by peds EM physicians (87.5% sensitive and 100% specific)
Interpreted by radiology (96% sensitive, 100% specific)
Consider using ultrasound as a noninvasive, radiation-free modality for accurate diagnosis of pediatric elbow fractures.
Lee SH, Yun SJ. Diagnostic Performance of Ultrasonography for Detection of Pediatric Elbow Fracture: A Meta-analysis. Ann Emerg Med. 2019;74(4):493-502.
Category: Pediatrics
Keywords: Female GU, abdominal pain, missed period (PubMed Search)
Posted: 8/21/2020 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Definition: Congenital anomaly where the hymen is completely obstructing the vaginal opening
Demographic: Incidence 0.05-0.1% of females
History: Most are asymptomatic and diagnosed on physical exam or incidentally when there is lack of menarche. Symptoms in adolescents can include: Abdominal pain (50%), urinary retention (20%), abnormal menstruation (14%), dysuria (10%), frequency, renal failure, UTI and back pain.
Physical exam: bulging, blueish hymenal membrane
Complications: Late detection can lead to infections, fertility problems, endometriosis, hydronephrosis, and rarely renal failure
ED treatment: If abdominal pain is significant or there is urinary obstruction, a urinary foley can be placed. GYN should be consulted.
Definitive treatment: Hymenectomy, hymenotomy, carbon dioxide laser treatments or foley insertion through the hymen (done by a specialist).
Lee K, Hong J, Jung H et al. Imperforate Hymen: A Comprehensive Systematic Review. J Clin Med 2019; 8(56): 1-14.
Category: Toxicology
Keywords: baclofen overdose, hemodialysis, renal elimination (PubMed Search)
Posted: 8/20/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Baclofen is a presynaptic GABA-B receptor agonist in the spinal cord that is primarily used for muscle spasms/spasticity. In large overdose, baclofen can produce CNS depression, respiratory depression, bradycardia/hypotension, hypothermia, seizure and coma.
Baclofen is primarily eliminated by the kidney. In patients with end-stage kidney disease/acute kidney failure, hemodialysis (HD) has been used to enhance baclofen clearance. However, it is unclear if there is a benefit of using HD in patients with normal kidney function.
In a recently published case report, HD was implemented in an attempt to shorten the anticipated prolonged ICU course.
Case: 14 year old (51 kg) woman ingested 60 tablets of baclofen (20 mg tablets)
Her symptoms were:
Baclofen level: 882 ng/mL (therapeutic range: 80 – 400 ng/mL)
Baclofen clearance from hemodialysis vs. urine
Patient’s mental status improved on hospital day 6 and was extubated. She was discharged to psychiatry on hospital day 14.
Conclusion:
Lee VR et al. Removal of baclofen with hemodialysis is negligible compared to intact kidney excretion in a pediatric overdose: a case report. Clin Toxicol. 2020
Category: Critical Care
Keywords: COVID-19, ARDS, Pneumonia, Steroids (PubMed Search)
Posted: 8/17/2020 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Another week, another COVID-19 study...
On August 12th, the Metcovid study was e-published ahead of print in Clinical Infectious Diseases. This was another study looking at steroids in COVID-19 pneumonia, this time performed in Brazil. Metcovid was a parallel, double-blind, randomized, placebo-controlled phase IIb clinical trial which enrolled 416 patients at a single academic center for the evaluation of methylprednisolone (MP; 0.5 mg/kg BID x 5 days) vs placebo. As with all COVID studies, Metcovid has some significant limitations, and some equivocal findings. However, Metcovid was largely in line with RECOVERY and other trials looking at steroids in COVID-19, which lends it some face validity. Metcovid found no significant difference in the primary outcome (mortality at day 28), but did find a difference in mortality in patients over 60 years old (a post-hoc analysis). Metcovid was probably underpowered (sample size was based on a 50% reduction in mortality), and did have a very small trend towards reduced mortality in the MP group (37.1% vs 38.2%, p=0.629).
Bottom Line:
Category: Toxicology
Keywords: nitrous oxide abuse, neurologic findings, physical exam (PubMed Search)
Posted: 8/13/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
What physical exam findings are associated with nitrous oxide abuse?
Nitrous oxide (NO) inhalation abuse, also called “whip-its” or “whippets”, inactivates vitamin B12 and create a vitamin B12 deficiency state. Chronic abuse of nitrous oxide can result in neurologic deficits/findings affecting the posterior/dorsal column of the spinal cord.
Physical exam findings:
Category: Neurology
Keywords: cerebrospinal fluid, rhinorrhea, otorrhea, halo, double ring, beta-2 transferrin (PubMed Search)
Posted: 8/12/2020 by WanTsu Wendy Chang, MD
(Updated: 2/8/2026)
Click here to contact WanTsu Wendy Chang, MD
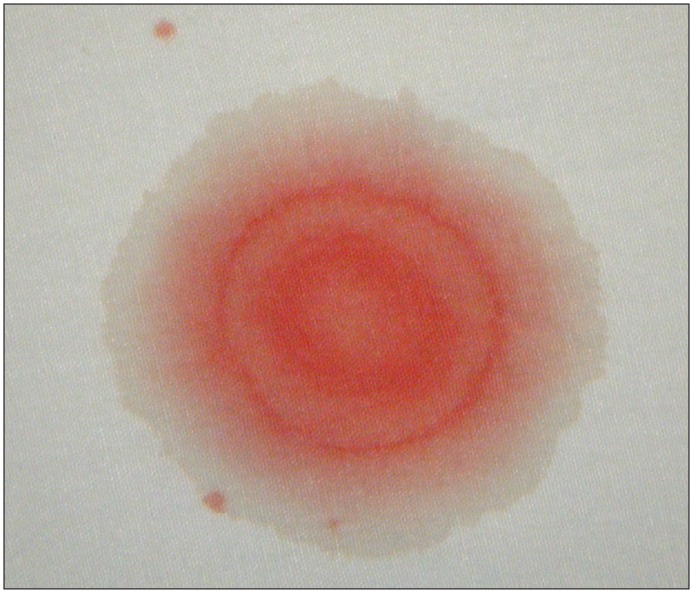
Bottom Line: Beta-2 transferrin is more accurate than the halo sign to identify CSF containing fluid.
Follow me on Twitter @EM_NCC
Category: Orthopedics
Keywords: Peripheral neuropathy, median nerve (PubMed Search)
Posted: 8/8/2020 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Pronator Teres Syndrome
A compressive neuropathy of the median nerve in the region of the elbow
The median nerve passes through the cubital fossa and passes between the superficial and deep heads of the pronator teres muscle.
Rare compared to other compressive neuropathies such as carpal tunnel syndrome.
More common in women and in fifth decade of life
May be seen with weight lifters, arm wrestlers, rowers, tennis, archery, professional cyclists, dentists, fiddlers, pianists, harpists
Also associated with well-developed forearm muscles
History:
Forearm pain – unlike carpal tunnel
Paresthesias in median distribution
No night symptoms – unlike carpal tunnel
Physical exam:
Sensory loss in medial nerve distribution.
Involves the thenar eminence!
Unlike carpal tunnel syndrome which doesn’t involve sensory loss in thenar eminence.
Pain may be made worse with resisted forearm pronation
Compression/Tinel’s sign over pronator mass reproduces symptoms
Treatment:
Splinting which limits pronation and NSAIDs
Steroid injection
Surgical nerve decompression is non operative treatment fails after greater than 6 months (rare)
Category: Critical Care
Keywords: gastrointestinal bleeding, TXA (PubMed Search)
Posted: 7/30/2020 by Lindsay Ritter, MD
(Updated: 8/4/2020)
Click here to contact Lindsay Ritter, MD
Prior to this study, a Cochrane review and meta-analysis of TXA for upper GI bleeds with 7 trials (1654 patients), showed a large reduction in mortality with TXA (RR 0.61, 95% CI 0.42-0.98, p=0.01)
Design:
-Randomized, international, multicentre, placebo-controlled trial at 164 hospitals in 15 countries Juy 2013-2019
->16/18 years old with upper or lower GI bleeding
-1 g TXA IV over 10 minutes followed by maintenance dose 3 g TXA over 24 hours
Results:
-Main outcome death due to bleeding within 5 days
-4% (222/5994) died in TXA group vs 4% (226/5981) placebo risk ratio RR 0.99, 95% CI 0.82-1.18
-Arterial thromboembolic events MI/CVA similar in both groups (0.7% vs 0.8%)
-Venous thromboembolic events PE/DVT higher in TXA group (0.8% vs 0.4%)
Pitfalls:
-Initially calculated all cause mortality until realization that over half deaths were due to non-bleeding causes, changed to death related to bleeding, allowing study appropriate power to detect difference
-Majority of patients had UGIB/variceal bleeding due to liver disease, over 75% deaths in those with liver disease
-Only 16% patients randomized in <3 hours, most >8 hours (CRASH-2 trial found benefit TXA in trauma patients only <3 hrs to administration)
Takeaway:
-TXA should not be used in the management of GI bleeds
-Increased venous thromboembolic events associated with TXA administration for GI bleeds
HALT-IT Trial Collaborators. Effects of a high-dose 24-h infusion of tranexamic acid on death and thromboembolic events in patients with acute gastrointestinal bleeding (HALT-IT): an international randomised, double-blind, placebo-controlled trial. Lancet. 2020;395(10241):1927-1936. doi:10.1016/S0140-6736(20)30848-5
Gluud LL, Klingenberg SL, Langholz E. Tranexamic acid for upper gastrointestinal bleeding. Cochrane Database Syst Rev. 2012;1
Category: Pharmacology & Therapeutics
Keywords: Cirrhosis, Pain, Acetaminophen, NSAID, Opioid (PubMed Search)
Posted: 8/1/2020 by Wesley Oliver
(Updated: 2/8/2026)
Click here to contact Wesley Oliver
The liver performs an essential role in the metabolism and clearance of many drugs. Liver damage due to cirrhosis can decrease first-pass metabolism of oral medications and increase free-drug concentrations of protein-bound medications due to decreased albumin production. In the absence of cirrhosis, patients with chronic hepatitis or hepatic cancer may only have a small decrease in drug clearance. Hepatic dose adjustments are not as prevalent or readily available as renal dose adjustments, which can create difficulty in finding the balance between pain relief and adverse effects.
The most common medications used for pain control in the emergency department are acetaminophen, NSAIDs, and opioids.
Acetaminophen
It is sometimes misconceived that acetaminophen should never be used in patients with cirrhosis due to the common knowledge that acetaminophen overdoses can cause hepatotoxicity. Alcoholics may have an increased risk of hepatotoxicity due to induction of CYP2E1 and decreased glutathione stores. However, acetaminophen is safe in patients with cirrhosis when used at appropriate doses. Limit the total daily dose of acetaminophen to 2 g daily in patients with cirrhosis and avoid acetaminophen in patients that are actively drinking. Also, educate patients that over-the-counter (OTC) and prescription medications may contain acetaminophen.
NSAIDs
In patients with cirrhosis, NSAIDs have increased bioavailability due to decreased CYP metabolism and decreased protein binding. In addition, prostaglandin inhibition can precipitate renal failure and sodium retention, worsening ascites and increasing the risk of hepatorenal syndrome, and increase the risk of gastrointestinal bleeding. Thrombocytopenia from NSAID use can further increase the risk of bleeding. Thus, avoid NSAID use in patients with cirrhosis. Topical NSAIDs can be considered.
Opioids
Opioid metabolism is altered in patients with cirrhosis and can contribute to complications with cirrhosis, such as precipitating encephalopathy. Generally, the bioavailability is increased and half-life is extended; thus, lower doses of immediate-release (IR) formulations at extended dosing intervals should be utilized. Common opioids for acute pain control in the emergency department are fentanyl, hydrocodone/oxycodone, hydromorphone, and morphine.
Take Home Points
| Drug/Class | Preferred Agent | Considerations |
| Acetaminophen | Max daily dose 2 g/day | Avoid if actively drinking. Be cautious if patient also taking OTC or combination products. |
| NSAIDs | None; Avoid | Topical NSAIDs may be considered. |
| Opioids | Hydromorphone, Fentanyl | Start with IR products at lower doses and extended intervals. |
1. Rakoski M, Goayl P, Spencer-Safier M, Weissman J, Mohr G, Volk M. Pain management in patients with cirrhosis. Clinical Liver Disease. 2018;11:135-140.
2. Wehrer M. Pain management considerations in cirrhosis. US Pharm. 2015;40:HS5-HS11.
Category: Critical Care
Keywords: albumin, crystalloids, sepsis (PubMed Search)
Posted: 7/25/2020 by Quincy Tran, MD, PhD
(Updated: 7/28/2020)
Click here to contact Quincy Tran, MD, PhD
Patient
Single Center, double-blinded, randomized trial.
Patients with cancer and septic shock
Intervention
4% albumin + lactate ringer bolus in 10 minutes
180 patients
Comparison:
Lactate ringer bolus in 10 minutes
180 patients
Outcome:
Primary: Any mortality within 7 days of randomization.
Secondary: Mortality within 28 days, renal replacement therapy (RRT)
Results:
7-day mortality: 46 (25%) for LR + albumin vs. 40 (22%) for LR only
28-day mortality: 96 (53%) for LR + albumin vs. 83 (46%) for LR only
RRT: 16 (9%) for LR + albumin vs. 12 (7) for LR only
Conclusion:
Adding albumin for early resuscitation to crystalloids did not improve mortality in cancer patients with septic shock.
Lactated Ringer's Versus 4% Albumin on Lactated Ringer's in Early Sepsis Therapy in Cancer Patients: A Pilot Single-Center Randomized Trial.
Crit. Care Med. 2019 Oct;47(10):e798-e805.
Category: Pediatrics
Keywords: MVC, neck injury, neurological injury (PubMed Search)
Posted: 7/24/2020 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
There is no well validated clinical decision rule similar to NEXUS or the Canadian Cervical Spine rule in children for clearing the cervical spine. Clinical clearance versus imaging first is a complicated decision. Certain risk factors may predispose children to injury and should be taken into account when deciding about clinical clearance versus imaging (XR).
High Risk Criteria for Cervical Spine Injury in Pediatrics
| Mechanism
| High risk MVC Intrusion > 12 inches at the occupant site Intrusion > 18 inches at any site Partial or complete ejection Death in the same passenger compartment Vehicle telemetry consistent with high speed Fall > 10 feet Nonaccidental trauma Diving injury |
| History
| Down’s Syndrome 22.q11.2 deletion Klippel-Fiel syndrome |
| Physical Exam
| Altered mental status Intoxication Hypotension Focal neurological exam Neck pain Torticollis |
Gopinathan N, Viswanathan V, Crawford A. Cervical Spine Evaluation in Pediatric Trauma: A Review and an Update of Current Concepts. Indian J Orthop 2018;52(5):489-500.
Leonard J, Browne L and Ahmed F et al. Cervical Spine Injury Risk Factors in Children with Blunt Trauma. Pediatrics 2019;144 (1):e20183221.
Kliegman R, Stanton B, St Geme J et al. Nelson Textbook of Pediatrics. 20th edition Vol 1 and 2. 2016. Elsevier. P 549-550, 3299-3300, 3352.
Category: Toxicology
Keywords: tianeptine, clinical characteristics, poison center (PubMed Search)
Posted: 7/23/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Tianeptine is an antidepressant with mu-opioid receptor agonism. It is available in several European countries for therapeutic use, but not available in the US.
There has been an increase in tianeptine exposure in the US since August 2019. Recently a retrospective observation study was done to characterize the clinical features associated with tianeptine exposure.
Result
| Intoxication (n=11) | Withdrawal (n=27) |
| Symptoms · Lethargy: 7 (63%) · Agitation: 3 (27%) · Tachycardia: 3 (27%) · GI distress: 2 (18%) · Myoclonic/hallucination: 2 (18) | Symptoms · Anxiety: 12 (44%) · GI distress: 3 (33%) · Hypertension: 8 (30%) · Agitation: 8 (30%) · Tachycardia: 7 (26%) |
| Treatment · Naloxone: 3 (27%) · Benzodiazepines: 2 (18%) · Antipsychotics: 2 (18%) · Antimuscarinic: 1 (9%)
| Treatment · Benzodiazepine: 10 (37%) · Opioids: 6 (22%) · Alpha-2-agonist: 5 (19%) · Antipsychotics: 5 (19%) · Antimuscarinic: 5 (19%) |
| Disposition · ICU: 6 (55%) · Non-ICU: 2 (18%) · Discharged home: 2 (18%)
| Disposition · ICU: 4 (15%) · Non-ICU: 7 (26%) · Psych: 1 (4%) · Discharged home: 10 (37%) |
Conclusion
Rushton W et al. Characteristics of tianeptine effects reported to a poison control center: a growing threat to pubic health. Clin Toxicol (Phila) 2020. DOI: 10.1080/15563650.2020.1781151
Category: Critical Care
Posted: 7/21/2020 by Caleb Chan, MD
(Updated: 2/8/2026)
Click here to contact Caleb Chan, MD
Design
-Two-center prospective observational study with 157 patients admitted to the ICU for pneumonia and being treated with HFNC
-ROX (Respiratory rate-OXygenation) index = ratio of SpO2/FIO2 to RR
Results:
-ROX index ≥4.88 at 12 hours after HFNC onset with a sensitivity of 70.1%, a specificity of 72.4%, PPV of 89.4%, NPV of 42%, LR+ of 2.54, and LR- of 0.41 in predicting treatment failure
Validation study: Roca, 2019
-results similar, but ROX index ≥4.88 at 12 hour with LR+ of only 1.82
-also found that a ROX index of <3.85 at 12 hours had a sensitivity of 23.5%, specificity of 98.4%, PPV of 88.9, NPV 69.9, LR+ of 14.47, and LR- 0.78
Pitfalls:
-decision to intubate was not made based on ROX index
-criteria for intubation was also part of the ROX index
-NIV was not part of their treatment algorithm
-created and validated prior to current COVID-19 pandemic
Takeaways:
- The ROX index can be a tool to help predict whether a patient with pneumonia on HFNC may need mechanical ventilation or higher level of care
- May be most helpful with patients with pneumonia on HFNC boarding in the ED
- At 12 hours of HFNC, ROX index of >4.88 suggests patient likely to succeed with HFNC vs. <3.85 which suggests likely need for mechanical ventilation
Roca O, Messika J, Caralt B, et al. Predicting success of high-flow nasal cannula in pneumonia patients with hypoxemic respiratory failure: The utility of the ROX index. J Crit Care. 2016;35:200-5.
Roca O, Caralt B, Messika J, et al. An Index Combining Respiratory Rate and Oxygenation to Predict Outcome of Nasal High-Flow Therapy. Am J Respir Crit Care Med. 2019;199(11):1368-1376.
