Category: Critical Care
Keywords: pericardial tampaonde, shock, tamponade, fluids, hypoperfusion (PubMed Search)
Posted: 2/13/2012 by Haney Mallemat, MD
(Updated: 2/15/2012)
Click here to contact Haney Mallemat, MD
A fluid bolus is often the first-line therapy for patients with pericardial tamponade. A fluid bolus, however, may not always improve hemodynamics.
The cardiac index of forty-nine patients with cardiac tamponade was assessed before and after a 500 cc normal saline bolus:
Bottom-line: A fluid bolus may a reasonable first choice in a hypotensive patient with tamponade, but remember that fluid boluses may not always work. Attempts at fluid resuscitation should never delay definitive treatment with pericardiocentesis.
Sagrista-Sauleda, et al. Hemodynamic effects of volume expansion in patients with cardiac tamponade. Circulation 2008; 117:1545
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Visual Diagnosis
Posted: 2/13/2012 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
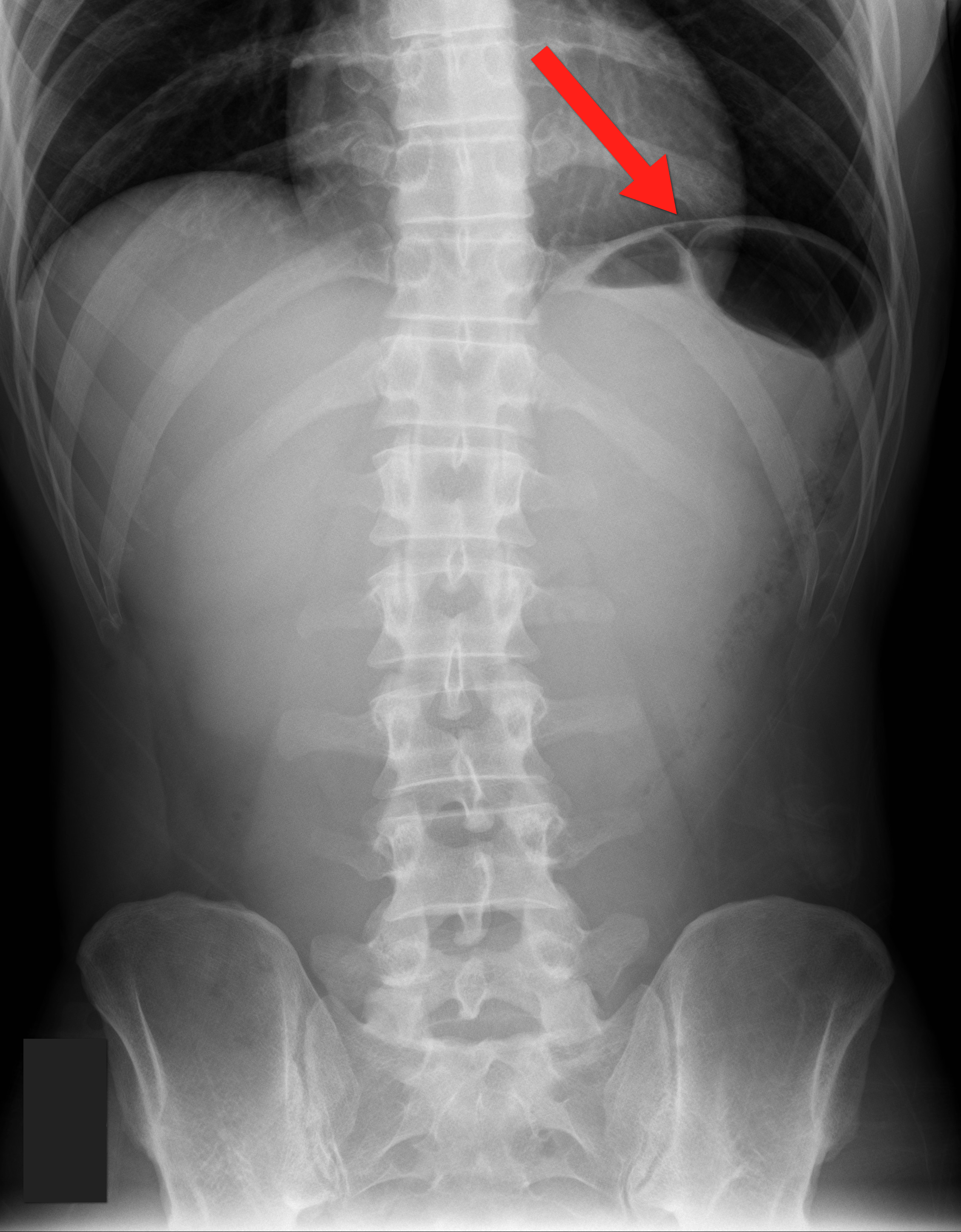
35 year old male with sudden onset of abdominal pain. Diagnosis?

Answer: Pneumoperitoneum
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: ACS, MI, painless, CAD, acute coronary syndrome (PubMed Search)
Posted: 2/12/2012 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
You might think that patients with painless MIs might have a better prognosis than patients with pain. Unfortunately, this is just not true. A recent study (1) supported prior literature indicating that the lack of pain is not a predictor of a more benign course, and in fact patients with painless MIs have a higher in-hospital and 1-year mortality. There are several other factors that may associate lack of pain with worse outcomes (e.g. painless MIs occur more often in older patients), but regardless it's important to remember that (1) many patients with MI will present without pain, and (2) the lack of "typical" symptoms should not be reassuring.
Cho JY, et a. Comparison of outcomes of patients with painless versus painful ST-segment elevation myocardial infarction undergoing percutaneous coronary intervention. Am J Cardiol 2012;109:337-343.
Category: Orthopedics
Keywords: herbal, supplements, complementary medicine (PubMed Search)
Posted: 2/11/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Common herbs and supplements used to treat pain
1) Turmeric root - used for arthritis pain. Little evidence to support its use. May slow blood clotting/enhance anticoagulant/antiplatelet effects.
2) Boswellia - used for OA and RA pain. Little evidence to support its use.May interfere with anticoagulant drugs and leukotreine inhibitors.
3) St. John's Wort - used for HA, migraine, neuralgia, muscle pain, sciatica, fibromyalgia. Little to no evidence to support its use.May interfere with numerous medications including anticoagulants, digoxin and SZ medications.
4) Glucosamine and Chondroitin - used for OA, knee pain, back pain. The glucosamine/chondroitin arthritis intervention trial found that "the dietary supplements Glucosamine and Chondroitin, taken alone or in combination are generally ineffective for OA pain of the knee." May increase the effect of Warfarin.
5) KavaKava - used for HA, muscle pain. Insufficient evidence demonstrating effectiveness for treatment of painful conditions. May cause severe liver damage and potentiate drowsiness side effects of other medications.
6) Echinacea - used for pain, migraines, arthritis. Little evidence to support its use. May exacerbate symptoms of autoimmune disorders.
7) Valerian root – used for joint and muscle pain. Insufficient evidence to support its use. May potentiate sedative side effects of barbiturates and benzos.
8) Chinese Thunder God Vine – used for arthritis. There is some evidence to suggest that this agent has anti-inflammatory properties. Long term this agent may decrease bone mineral density in women, decrease fertility in men, and may produce GI side effects.
9) Feverfew – used for muscle pain, arthritis. Some evidence to suggest that may reduce frequency of migraine headaches. No evidence for benefit in RA. May enhance effects of anticoagulants and some drugs that undergo hepatic metabolism.
10) Cat’s claw – used for herpes zoster, bone pain, arthritis. Possible benefit for OA and RA in small studies in humans but no large study has shown benefit. May interact with clotting agents, BP meds and cyclosporine.
11) Black Cohosh – used for muscle pain and arthritis. Insufficient evidence demonstrating benefit. May be associated with severe liver side effects.
12) Bromelain – used for muscle pain, arthritis, knee pain. The NIH reports that bromelain may be effective for arthritis when used in combination with trypsin and rutin. May interact with amoxicillin and other antibiotics, anticoagulants and antiplatelet drugs.
13) Devil’s claw – used for muscle pain, back pain, arthritis, migraine. The NIH reports that “taking devil’s claw alone or with NSAIDs seems to help decrease OA related pain.” May increase effects of warfarin.
Category: Pediatrics
Posted: 2/10/2012 by Rose Chasm, MD
(Updated: 2/8/2026)
Click here to contact Rose Chasm, MD
Emergency Medicine Clinics of North America
Orothopedic Emergencies
November 2010, Volume 28, Number 4
Category: Toxicology
Keywords: DRESS, anticonvulsant, eosinophilia, phenytoin, carbamazepine (PubMed Search)
Posted: 2/7/2012 by Bryan Hayes, PharmD
(Updated: 2/19/2012)
Click here to contact Bryan Hayes, PharmD
Drug rash with eosinophilia and systemic symptoms (DRESS) syndrome, previously named “anticonvulsant hypersensitivity syndrome,” is a severe adverse drug reaction which occurs in approximately 1 of every 1,000–10,000 uses of anticonvulsants.
Characterized by triad of fever, rash, and internal organ involvement.
Usually involves aromatic anticonvulsants such as phenytoin, carbamazepine, phenobarbital, primidone, lamotrigine, and possibly oxcarbazepine.
DRESS occurs most frequently within the first 2 months of therapy and is not related to dose or serum concentration.
Treatment includes prompt discontinuation of the offending agent. Patients should be admitted to the hospital and receive methylprednisolone 0.5–1 mg/kg/d divided in four doses. Other promising therapies include use of IVIG.
Follow me on Twitter (@pharmacytoxguy)
Category: Critical Care
Posted: 2/7/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
ECMO for ARDS and Refractory Hypoxemia
Brodie D, Bacchetta M. Extracorporeal membrane oxygenation for ARDS is adults. NEJM 2011;365:1905-14.
Category: Visual Diagnosis
Posted: 2/5/2012 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
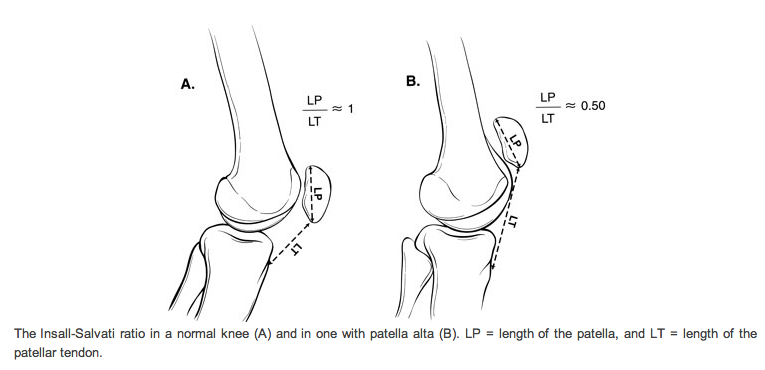
28 y.o. male felt his left knee "pop" after landing from a jump while playing basketball. Knee exam revealed limited knee extension. X-ray is shown. Diagnosis?

Answer: Patella Alta secondary to Patellar tendon rupture
References
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Pharmacology & Therapeutics
Keywords: droperidol, antiemetic, qt prolongation (PubMed Search)
Posted: 1/31/2012 by Bryan Hayes, PharmD
(Updated: 2/4/2012)
Click here to contact Bryan Hayes, PharmD
In the setting of critical drug shortages of ondansetron, prochlorperazine, and metoclopramide, consider droperidol as a viable option for the treatment of nausea and vomiting.
Although it is similar to haloperidol, it is actually FDA-approved for “prevention and/or treatment of nausea and vomiting from surgical and diagnostic procedures” (unlike haloperidol). Ironically, it is not approved for agitation, although it can be used for that indication.
Dosing for antiemesis is 1.25 to 2.5 mg IV/IM. Additional doses of 0.625 to 1.25 mg can be administered to achieve desired effect. Onset is 3-5 minutes and duration of effect is 2-4 hours. It should be administered via slow IV push over 2 minutes.
Why is it not commonly used? Black Box Warning for QTc prolongation. An ECG is a must prior to administration. Also be cautious in patients who are on other medications that can prolong the QT interval (www.qtdrugs.org).
Category: Pharmacology & Therapeutics
Keywords: ondansetron, zofran, prolonged QT, torsades, drug interactions, ciprofloxacin, antifungal, azoles (PubMed Search)
Posted: 2/2/2012 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Category: Critical Care
Posted: 1/31/2012 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
AGE occurs when gas bubbles enter arteries or veins; AGE may cause clinical symptoms even with very small volumes of air.
Air enters the circulatory system via:
· Barotrauma – Alveolar injury allows air to enter systemic bloodstream; occurs in divers following rapid ascent after breath holding, during mechanical ventilation, chest tube placement, or bronchoscopy
· Decompression sickness – Dissolved gas precipitates out of bloodstream as bubbles; typically following scuba diving without appropriate time to ascend or prolonged flying in unpressurized aircrafts
· Direct injection of air into arterial or venous circulation – Examples include accidental IV injection of air, needle biopsy of lung, or aspiration of air during central line placement
Serious clinical manifestations include:
· Neurologic changes - loss of consciousness, confusion, or focal neurological deficits
· Hemodynamic changes – hypotension, arrhythmias, cardiac ischemia, or cardiac arrest.
· Respiratory changes – obstruction of pulmonary circulation, pulmonary edema, or hypoxemia
Treatment:
· Strict attention to ABC’s using high-flow O2.
· Keep head of bed elevated to minimize/reduce cerebral edema.
· Hyperbaric Oxygen (HBO) therapy is recommended for neurological manifestations or cardiovascular instability. Good outcomes associated with shorter intervals from air embolism to HBO. Typically only 1 to 2 treatments are needed; occasionally additional treatments are necessary.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Financial & Investing
Keywords: 457b, retirement, investing (PubMed Search)
Posted: 1/29/2012 by Dan Lemkin, MS, MD
Click here to contact Dan Lemkin, MS, MD
Many physicians have the opportunity to invest in a variety of retirement funds. The most common commercial vehicle is a 401k. Academic and non-profits have access to an analogous 403b. Many physicians also have access to a 457b.
It is important to understand what it is, and most importantly how it differs from a conventional 401k or 403b. Like its' peers, it permit pre-tax contributions of a finite amount. They are offered through your employer and are bound to a specific vendor(s). These vendors provide a select number of investment choices specific to the employer contract. The maximum contribution for 2012 is $17,000.
The 457b is different from the other investment vehicles because of who and where your funds are held:
Non-governmental 457 plans have a number of restrictions that governmental ones do not. Money deferred into non-governmental 457 plans may not be rolled into any other type of tax-deferred retirement plan. It may be rolled only into another non-governmental 457 plan. Also, money deferred into non-governmental plans is not set aside in a trust for the exclusive benefit of the employee making the deferral. The Internal Revenue Code requires that money in a non-governmental 457 plan remains the property of the employer and is thus available to general creditors of the employer in legal or bankruptcy
If you work for a private entity, or a non-profit and they offer a non-governmental 457b, your personal funds are pooled with corporate resources. Your retirement contributions are at risk, should the company default and declare bankruptcy. This risk is apparently not born by GSRA 457b (Governmental agency 457b plans). A decade ago, this risk would seem insignificant. With the number of large companies and municipalities defaulting in this economic climate, prudence is warranted when considering this investment vehicle. DISCLAIMER - This pearl is not intended to provide financial advice. Please consult your HR department and / or financial advisor for additional information and advice.
Category: Orthopedics
Keywords: Hip dislocation, technique, reduction (PubMed Search)
Posted: 1/28/2012 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Our old friend Captain Morgan (the rum pirate) may now be able to assist us during a shift, not just afterwards.
http://www.inquisitr.com/wp-content/2011/08/captain-morgans-pirate-ship-satisfaction-panama.jpg
In a small case series in last months Annals of Emergency Medicine, a new reduction maneuver was described as an alternative to the traditional Aliis's maneuver.
The maneuver is named after the pirate spokesperson for the similarities in body positioning.
The patient is placed supine on a stretcher. The pelvis is fixed to a backboard with a strap. The patient's hip and knee are flexed to 90 degrees. The physician places one foot on the back board with the same knee behind the patient's knee. By holding the patient's ankle down, the patient's knee is kept in flexion. The physician then lifts his/her calf, thereby applying an upward force to the hip while gently rotating the lower leg from side to side.
http://www.youtube.com/watch?v=l07K-mO2X84
with a slight variation
http://www.youtube.com/watch?v=sGQZaqB48rw
The success rate was 12 of 13 cases. The single failure occurred in a patient with an acetabular fracture with an intra-articular fragment requiring open reduction. There were no described neurovascular complications or injuries to the knee. The technique limits the physician's risk of back strain and of falling from the stretcher.
The Captain Morgan technique for the reduction of the dislocated hip.
Hendey GW, Avila A.
Ann Emerg Med. 2011 Dec;58(6):536-40. Epub 2011 Aug 12.
Category: Pediatrics
Posted: 1/27/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Potential Causes of Neonatal Apnea and Bradycardia
• Central nervous system
Intraventricular hemorrhage, drugs maternal/fetal, seizures, hypoxic injury, herniation, neuromuscular disorders, brainstem infarction or anomalies (e.g., olivopontocerebellar atrophy), general anesthesia.
• Respiratory
Pneumonia, obstructive airway lesions, upper airway collapse, atelectasis, extreme prematurity (<1,000 g), phrenic nerve paralysis, severe hyaline membrane disease, pneumothorax, hypoxia, malformations of the chest.
• Infectious
Sepsis, meningitis (bacterial, fungal, viral), RSV
• Metabolic
Hypoglycemia, hyper/hyponatrmia, hyperammonemia, decreased organic acids, hypothermia.
• Cardiovascular
Hypotension/hypovolemia, heart failure, PDA, anemia, vagal tone.
Category: Toxicology
Keywords: paralytic, hyperkalemia, succinylcholine (PubMed Search)
Posted: 1/26/2012 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
As we go through the problems of national drug shortages it is important to remember the old drugs but to also remember why they became old and seldom used drugs. Prime example is many hospitals are beginning to develop shortages of rocuronium - the nondepolarizing paralytic that has a fast onset. This shortage has caused many to switch back to succinylcholine. The following case report should serve as reminder of how succinylcholine - due to its depolarizing nature and fasciculations - can cause a transient but significant hyperkalemia.
Levine M et al. – This case report describes a 38–year–old woman with multiple sclerosis who developed life–threatening hyperkalemia after the administration of succinylcholine during rapid sequence intubation. This case highlights the potential for iatrogenic hyperkalemia after succinylcholine in patients with neurologic diseases, including multiple sclerosis.
Category: Critical Care
Posted: 1/24/2012 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
SAH and Pulmonary Edema - Think Twice About Diuresis!
Scalfani MT, Diringer MN. Year in review 2010: Critical Care - neurocritical care. Crit Care 2011;15:237.
Category: Visual Diagnosis
Posted: 1/22/2012 by Haney Mallemat, MD
(Updated: 1/23/2012)
Click here to contact Haney Mallemat, MD
20 year old female complains of “itchy” rash to her foot x 1 week and recently the rash has spread to her other other foot and both hands (shown below). No past medical history, no fever or chills, no mucus membranes involvement, no new medications, no tick bites, no travel. She is also 16 weeks pregnant. What’s the diagnosis?
Answer: Secondary syphilis
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Geriatrics
Keywords: infection, sepsis, bacteremia, geriatrics, elderly, white blood cell count (PubMed Search)
Posted: 1/22/2012 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
The WBC count is normal in up to 45% of elderly patients with bacteremia. The most predictive factors for bacteremia in the elderly are delirium, vomiting, bandemia, and tachypnea.
Category: Orthopedics
Keywords: Flexor, Tenosynovitis (PubMed Search)
Posted: 1/21/2012 by Michael Bond, MD
Click here to contact Michael Bond, MD
Flexor Tenosynovitis
You can follow this link, http://www.youtube.com/watch?v=qf9SW0ChsCU , to see the physical exam findings of flexor tenosynovitis
Category: Pediatrics
Keywords: infectious disease, neonatal infections, umbilical disorders (PubMed Search)
Posted: 1/20/2012 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
