Category: Toxicology
Keywords: hydrogen peroxide (PubMed Search)
Posted: 12/22/2011 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Generally H2O2 is available OTC at a concentration of 3-9% and used as an antiseptic. Toxicity is by two methods: local irritation like a caustic and gas formation - both directly correlating with the % concentration. Some interesting findings have occurred with this ingestion including:
1) Portal vein gas seen on CT
2) Arterialization of O2 resulting in CVA
3) Encephalopathy with cortical visual impairment
4) MRI showing b/l hemispheric CVAs
Even use of 3% H2O2 for wound irrgation has caused subcutaneous emphysema and O2 emboli.
Treatment: XR/CT/MRI may detect gas, if present in RV should be placed in Tredelenburg and carefully aspirated through a central venous catheter. Anectdotal case reports have used HBO therapy when patients were critically ill.(1)
1) Mullins et al. Acute cerebral gas embolism from hydrogen peroxide ingestion successfully treated with HBO. J Toxicol Clin Toxicol 1998; 38: 111-112.
Category: Neurology
Keywords: increased intracranial pressure, opening pressure (PubMed Search)
Posted: 12/21/2011 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
--- Venous drainage obstruction (i.e. cerebral venous sinus thrombosis).
--- Endocrine (i.e. obesity, hypothyroidism, Cushing's disease, Addison's disease).
--- Medications (i.e. vitamin A, cyclosporine, lithium, lupron, oral contraceptives,
amiodorone, and antiobiotics such as tetracyclines and sulfonamides).
--- Other conditions (i.e. pregnancy, steroid withdrawal, acromegaly, polycystic ovary
syndrome, systemic lupus erythematosus, sleep apnea, HIV).
Category: Critical Care
Keywords: amiodarone, lung toxicity, ARDS, infection, critical care (PubMed Search)
Posted: 12/20/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Amiodarone-induced lung toxicity (ALT) is a serious and sometimes fatal complication of amiodarone use.
Symptoms range from mild (e.g., dyspnea with exertion) to acute respiratory distress syndrome and risk of death.
ALT is secondary to either release of toxic oxygen radials that are directly toxic to the lung or the reaction is secondary to an indirect immunologic reaction.
Risk factors for ALT: use > 2 months, dose > 400mg/day, advanced age, or pre-existing lung injury
ALT is typically a diagnosis of exclusion so suspect ALT through a detailed history; physical exam and radiology are non-specific. Lung biopsy is the only confirmatory test.
Treat ALT by discontinuing the drug, steroids, and supportive care. In rare cases where amiodarone cannot be safely discontinued (i.e., life-threatening arrhythmia), dosage should be reduced and steroids added immediately.
Generally, ALT is reversible with a good prognosis.
Mahajan, V. et al Amiodarone induced acute interstitial pneumonitis.BMJ Case Rep. 2009;2009.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Keywords: ECG, EKG, electrocardiography, electrocardiogram, rightward, axis (PubMed Search)
Posted: 12/18/2011 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
There are a handful of conditions associated with a rightward axis on the ECG: left posterior fascicular block, ventricular ectopy, lateral MI (old), pulmonary hypertension (acute or chronic), right ventricular hypertrophy, hyperkalemia, misplaced leads, and toxicity of sodium channel blocking drugs, to name a few.
When you notice that the rightward axis is NEW compared to an old ECG, and there's nothing else on the ECG that's obviously diagnostic (e.g. hyperkalemia would also show peaked Ts; ventricular tachycardia would be wide complex and fast, etc.), in emergency medicine you should always think first and foremost of the following three possibilities:
1. acute pulmonary embolus
2. toxicity of a sodium channel blocking drug
3. misplaced leads
Pay attention to axis! Using the above rule can make rightward axis very simple and useful.
AM
Category: Pediatrics
Keywords: Bayonet, fracture reduction technique, radius (PubMed Search)
Posted: 12/16/2011 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Pediatric forearm fractures:
Category: Neurology
Keywords: botulism, descending paralysis, clostridium botulinum, weakness (PubMed Search)
Posted: 12/14/2011 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Fernandez-Frackelton M. Bacteria. In: Marx J, Hockerberger R, Walls R, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. Phila: Mosby; 2009:1686-9.
Shearer p, Jagoda A. Neuromuscular Disorders. In: Marx J, Hockerberger R, Walls R, ed. Rosen's Emergency Medicine: Concepts and Clinical Practice. Phila: Mosby; 2009:1415.
Category: Critical Care
Posted: 12/13/2011 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
The Crashing Patient with PAH
Rubenfire M, Bayram M, Hector-Wood Z. Pulmonary hypertension in the critical care setting: classification, pathophysiology, diagnosis, and management. Crit Care Clin 2007;23: 801-834.
Category: Visual Diagnosis
Posted: 12/11/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
60 year old male with 6 months of weight loss and recent epistaxis. Diagnosis?
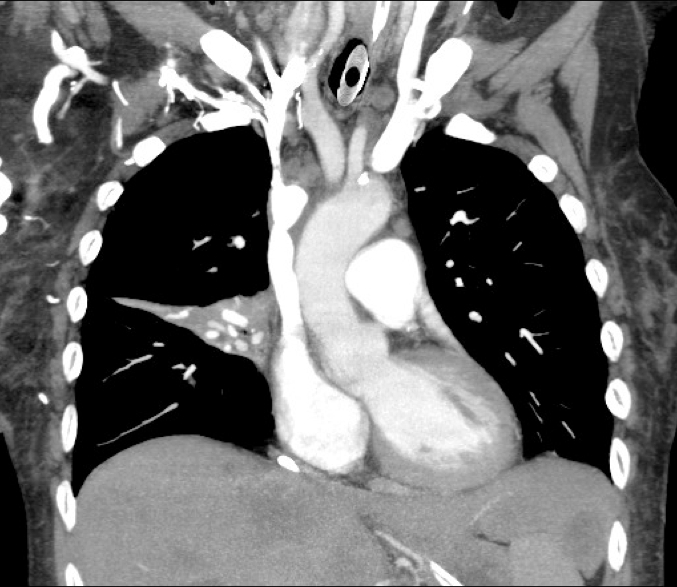
Answer: Partial obstruction of the Superior vena cava (SVC)
SVC Syndrome
SVC syndrome is caused by compression or obstruction of the superior vena cava blocking anterograde flow.
Most cases are secondary to extrinsic compression by malignancy. Other causes are secondary to thrombosis and internal obstruction (e.g., central venous catheter placement).
Symptoms present sub-acutely, worsen with bending over, and are secondary to increased venous pressure in the head and neck (e.g., epistaxis, headache, tinnitus, conjunctival injection, neck swelling, etc.).
Treatment focuses on reversing the underlying cause (e.g., radiation or chemotherapy if due a sensitive tumor) and treatment of symptoms:
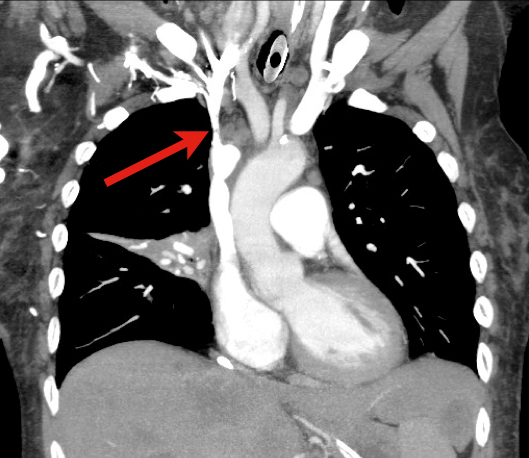
Rice TW, Rodriguez RM, Light RW. The superior vena cava syndrome: clinical characteristics and evolving etiology. Medicine (Baltimore). Jan 2006;85(1):37-42.
Nunnelee JD. Superior vena cava syndrome. J Vasc Nurs. Mar 2007;25(1):2-5; quiz 6.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Orthopedics
Keywords: fractures, child abuse, radiology (PubMed Search)
Posted: 12/10/2011 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Metaphyseal bucket handle and corner fractures are almost pathognomonic for child abuse
These injuries were originally identified by clinicians evaluating children with subdural hematomas
These injuries are typically seen in the ankles, knees, elbows and wrists
Violent twisting, shaking, or pulling across a joint creates shearing forces across the weak epiphyseal growth plate and metaphysis
This leads to
1) A thin rim of mineralized metaphyseal bone aka “bucket handle”
http://rad.usuhs.mil/rad/home/peds/bucketarrow.jpg
OR
2) Small flecks of bone from the metaphyseal corner adherent to periosteum
http://t2.gstatic.com/images?q=tbn:ANd9GcT0kZ3VR1f7MwRj7oIa6jaYVp_-f8kZ1NhSbw4kCTRGNLDJ1pKK9g
Category: Pediatrics
Posted: 12/9/2011 by Rose Chasm, MD
Click here to contact Rose Chasm, MD
NMS Pediatrics
Category: Toxicology
Keywords: warfarin, INR (PubMed Search)
Posted: 11/29/2011 by Bryan Hayes, PharmD
(Updated: 12/8/2011)
Click here to contact Bryan Hayes, PharmD
A recent study highlighted the challenges we face managing ED patients on warfarin therapy. Some key observations about how we're doing:
Literature continues to show warfarin is the most dangerous medication for our patients. Meticulous monitoring and follow up will help us potentially avoid serious interactions and adverse events.
Meeker E, et al. ED management of patients on warfarin therapy. Ann Emerg Med 2011;58:192-99.
Category: Neurology
Keywords: mictuation syncope, syncope, vagus nerve, vasovagal syncope (PubMed Search)
Posted: 12/7/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
-- occurs during or immediately following urination, often when bladder is full.
-- occurs at night or after standing from the recumbent position of a deep sleep to urinate.
-- risk factors: enlarged prostate, alpha blocker therapy, dehydration, alcohol, fatigue.
Category: Critical Care
Posted: 12/6/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Up until recently, a tight-fitting mask was one of the only ways to deliver non-invasive positive-pressure ventilation.
High-flow nasal cannulas (HFNC) have been adapted from use in neonates to adults to deliver continuous positive airway pressure (CPAP).
HFNC provides continuous, high-flow (up to 60 liters), and humidified-oxygen via nasal cannula providing positive pressure to the pharynx and hypopharynx. Patients tolerate it well and it is less claustrophobic than tight-fitting masks.
HFNC does not generate the same amount of pressure as CPAP so it may be best utilized as an intermediate step between low-flow oxygen (i.e., traditional nasal cannula) and non-invasive positive pressure ventilation with tight-fitting masks.
Check with your respiratory department if these devices are locally available.
Kernick, j. What is the evidence for the use of high flow nasal cannula oxygen in adult patients admitted to critical care units? A systematic review. Aust Crit Care. 2010 May;23(2):53-70. Epub 2010 Mar 5.
Parke, R. A preliminary randomized controlled trial to assess effectiveness of nasal high-flow oxygen in intensive care patients. Respir Care. 2011 Mar;56(3):265-70. Epub 2011 Jan 21.
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
Category: Cardiology
Posted: 12/4/2011 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Minimizing interruptions in chest compressions during CPR is critically important. As an example of the adverse consequences of interruptions, consider the following finding from Edelson (Resuscitation 2010): for every 10 seconds of hands-off time during cardiac arrest, the patient's chances of successful return of spontaneous circulation decreases by 50% due to reductions in cerebral perfusion.
Next time you are involved in a code, keep this in mind, and do EVERYTHING POSSIBLE to minimize those interruptions in chest compressions.
Category: Pediatrics
Keywords: child abuse, skeletal survey (PubMed Search)
Posted: 12/3/2011 by Vikramjit Gill, MD
Click here to contact Vikramjit Gill, MD
You just finished assessing a 6 month old in the Pediatric ED who can’t move his right leg. You suspect child abuse. You’re ready to order labs, a head CT, ophtho consult, skeletal survey and call Child Protective Services. While your doing all of this, your medical student asks you, “What exactly are you looking for on the skeletal survey?”
A skeletal survey is mandatory for cases of suspected child abuse in children under the age of 2 years. Approximately 60% of the fractures seen in abused children are younger than 18 months old.
When you are looking at a skeletal survey, carefully look for the following:
1. Multiple, healing fractures of various ages
2. Rib fractures, especially in the posterior ribs
3. Metaphyseal chip and buckle fractures
4. Spiral fractures in long bones (especially in children that can’t walk)
5. Skull fractures which are not simple and linear
6. Scapula fractures
More to come about child abuse….
References:
Category: Pharmacology & Therapeutics
Keywords: older adult, adverse drug event, ade, elderly, warfarin (PubMed Search)
Posted: 11/29/2011 by Bryan Hayes, PharmD
(Updated: 12/3/2011)
Click here to contact Bryan Hayes, PharmD
A recent article estimated 100,000 emergency hospitalizations for adverse drug events in U.S. adults 65 years of age or older each year. Nearly half of these hospitalizations were among adults ≥80 years old and two-thirds were due to unintentional overdoses.
Four medications or medication classes were implicated alone or in combination in 67% of hospitalizations:
Opioids were #5. Digoxin was #7 and resulted in the highest percentage of hospitalizations per ED visit at 80%.
Budnitz DS, et al. Emergency hospitalizations for adverse drug events in older Americans. N Engl J Med 2011;365:2002-12.
Category: Toxicology
Keywords: Insulin,beta blockers,calcium channel blockers (PubMed Search)
Posted: 12/1/2011 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
High dose insulin is recommended in treatment of beta-blocker and calcium channel blocker overdose. In a recent observational case series of cardiogenic shock, high dose insulin was evaluated for efficacy and safety.
Holger JS, Stellpfug SJ, Cole JB, Harris CR, Engebretsen KM. High-Dose Insulin: A Consecutive Case Series in Toxin-Induced Cardiogenic Shock. Clinical Toxicology Aug 2011;49(7):653-8.
Category: Neurology
Keywords: seizure, epilepsy (PubMed Search)
Posted: 11/30/2011 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Posted: 11/29/2011 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Hypotension in the PAH Patient
Rubenfire M, Bayram M, Hector-Wood Z. Pulmonary hypertension in the critical care setting: classification, pathophysiology, diagnosis, and management. Crit Care Clin 2007;23: 801-834.
Category: Visual Diagnosis
Posted: 11/27/2011 by Haney Mallemat, MD
(Updated: 11/28/2011)
Click here to contact Haney Mallemat, MD
9 year-old boy with sudden onset of unilateral facial swelling. What’s the diagnosis?

Answer: Acute Parotitis
Bonus Trivia: U.S. President Garfield died from parotitis after becoming dehydrated following abdominal surgery
Shelly J. McQuone MD, Acute Viral and Bacterial Infections of the Salivary Glands, Otolaryngologic Clinics of North America, Volume 32, Issue 5 (October 1999)
Follow me on Twitter (@criticalcarenow) or Google+ (+haney mallemat)
