Category: Pediatrics
Keywords: Bronchiolitis, RSV (PubMed Search)
Posted: 9/10/2010 by Adam Friedlander, MD
Click here to contact Adam Friedlander, MD
As RSV season approaches, remember these key points in managing bronchiolitis:
Category: Toxicology
Keywords: cyanide, lactate (PubMed Search)
Posted: 9/9/2010 by Bryan Hayes, PharmD
(Updated: 2/8/2026)
Click here to contact Bryan Hayes, PharmD
In the setting of acute cyanide poisoning, it is virtually impossible to obtain a timely cyanide level to help assess toxicity. However, there are two diagnostic tests that can help confirm your diagnosis.
Remember cyanide halts cellular respiration meaning the cells cannot utilize oxygen. Therefore, the venous PO2 should be about the same as the arterial PO2. The cells then switch to anaerobic metabolism, thereby producing lactate.
Category: Neurology
Keywords: median nerve block, nerve blok, median nerve (PubMed Search)
Posted: 9/8/2010 by Aisha Liferidge, MD
Click here to contact Aisha Liferidge, MD
How to Perform a Median Nerve Block
Category: Critical Care
Posted: 9/7/2010 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Pulmonary Contusion and Ventilator Management
Kiraly L, Schreiber M. Management of the crushed chest. Crit Care Med 2010; 38(S):S469-S477.
Category: Cardiology
Keywords: cocaine, myocardial infarction, atherosclerosis (PubMed Search)
Posted: 9/5/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
Acute use of cocaine increases risk of acute MI due to tachydysrhythmias, vasospasm, and increased platelet aggregation. There is a 24-fold increased risk of MI in the first hour after use of cocaine. 6% of patients presenting with cocaine-chest pain rule in for acute MI.
[Weber, Acad Emerg Med 2000]
Category: Orthopedics
Keywords: Elbow, radiographs (PubMed Search)
Posted: 9/4/2010 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Radiologic evaluation of the elbow (Part 2)
Helpful clues in the evaluation of elbow trauma:
Category: Toxicology
Keywords: Epinephrine, epi-pen, digital block, finger, ischemia (PubMed Search)
Posted: 9/2/2010 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
A recent study examined the effects of accidental digital epinephrine injection from auto-injectors. 127 cases with complete follow-up had the following effects:
Pharmacologic vasodilators were used in 23%. Four patients had possible digital ischemia. All patients had complete resolution of symptoms, most within 2 hours. No patient was admitted, received hand surgery consultation, or had surgical care.
Although this speaks for the safety of digital anesthesia using epinephrine, it underscores the importance of providing education to patients who are prescribed epinephrine auto-injectors.
Muck AE, Bebarta VS, Borys DJ, MOrgan DL. Six Years of Epinephrine Digital Injections: Absence of Significanct Local or Systemic Effects. Ann Em Med Sept 2010;56(3);270-4.
Singer AJ. Accidental Digital Self-Injection of Epinephrine: Debunking the Myth. Sept 2010;56(3):275-7.
Category: Neurology
Keywords: ulnar nerve block, ulnar nerve, nerve block (PubMed Search)
Posted: 9/1/2010 by Aisha Liferidge, MD
(Updated: 2/8/2026)
Click here to contact Aisha Liferidge, MD
Category: Critical Care
Keywords: SIADH, CSW, syndrome of inappropriate adh, cerebral salt wasting, hyponatremia, neurosurgery (PubMed Search)
Posted: 8/30/2010 by Haney Mallemat, MD
(Updated: 2/8/2026)
Click here to contact Haney Mallemat, MD
Hyponatremia plagues many neurosurgical patients due to the syndrome of inappropriate secretion of ADH (SIADH) or the cerebral salt wasting syndrome (CSW). Both diseases may appear similar (hyponatremia, increased urine osmolarity, increased urine sodium, normal adrenal, renal and thyroid function), but there is one BIG difference. Patients with SIADH are euvolemic or hypervolemic (excess ADH causes fluid retention) whereas patients with CSW are fluid depleted (impaired renal handling of sodium and water). To differentiate, look for signs of hypovolemia: orthostatics, dry mucus membranes, hemoconcentration, pre-renal azotemia, and/or hemodynamics (IVC collapse anyone?).
Bottom line: Distinguish SIADH from CSW because the treatments are exact opposites:
SIADH: Fluid restrict
CSW: Give water and salt (i.e., 0.9% saline)
Cerebral salt wasting syndrome: a review. Harrigan MR
Neurosurgery. 1996 Jan;38(1):152-60.
Category: Vascular
Keywords: Hypertension (PubMed Search)
Posted: 8/30/2010 by Rob Rogers, MD
(Updated: 2/8/2026)
Click here to contact Rob Rogers, MD
Hypertensive Encephalopathy (HE) is a clinical diagnosis and can look like many other disease entities.
HE refers to a relatively rapidly evolving syndrome of severe hypertension in association with severe headache, nausea, and vomiting, visual disturbances, convulsions, altered mental status and, in advanced cases, stupor and coma.
The key is the presence of severe hypertension. Remember, though, that 160/105 mm Hg may be high for an individual patient. Most patients with the syndrome will have diastolic pressures well in excess of 120-130 mm Hg. The only way you will know if the diagnosis is correct is to treat the BP (carefully control), work up other etiologies, and see of symptoms improve with BP control.
Beware the patient with severe HTN and seizure. Seizure may be the first, and only, symptom of hypertensive encephalopathy.
Category: Cardiology
Keywords: SVT, atrial fibrillation, WPW, antidromic, orthodromic (PubMed Search)
Posted: 8/29/2010 by Amal Mattu, MD
(Updated: 2/8/2026)
Click here to contact Amal Mattu, MD
Some confusion exists regarding proper distinction and treatment between the different tachydysrhythmias associated with WPW. Here's the scoop:
1. orthodromic SVT: narrow regular tachycardia, looks just like a routine SVT, treat just like any other SVT (AV nodal blockers work fine)
2. antidromic SVT: wide regular tachycardia, looks just like VTach, treat like VTach (amiodarone, procainamide, shock; lidocaine won't work, though won't harm either)
3. atrial fibrillation: very different!! irregularly irregular, morphologies of the QRS complexes vary between narrow and wide, some areas may have rates as high as 250-300/min, MUST avoid all AV nodal blockers (which includes adenosine, CCBs, BBs, digoxin, amiodarone); treat with procainamide or sedation+cardioversion
Category: Orthopedics
Keywords: Adhesive Capsulitis (PubMed Search)
Posted: 8/28/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Adhesive Capsulitis -- Frozen Shoulder
Category: Pediatrics
Posted: 8/18/2010 by Rose Chasm, MD
(Updated: 2/8/2026)
Click here to contact Rose Chasm, MD
MedStudy Pediatrics Board Review, Book 4, 1st edit
Category: Toxicology
Keywords: caustic (PubMed Search)
Posted: 8/26/2010 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
In a previous pearl we were discussing the need to perform EGD for any suicidal patient with a history of ingestion of a caustic to grade injury and assess chance of perforation and/or stricture formation. Suicidal patients are intentionally ingesting the caustic and can thus justify the risk/benefit ratio more easily than the pediatric unintentional ingestion. The concerned parent will bring the child in with a possible ingestion of a caustic. The container could be simply in the same room, spilled on the child and never be ingested. Even if ingested, the amount is less if the child tastes the caustic and will reflexively cause spitting. The literature is scant in regards to this type of patient but seems to point to this general algorithm:
Child displays 2 or more of the following symptoms there is enough evidence from case series that there will be a clinically signficant lesion found on EGD.
Vomiting, Drooling, Stridor, Presence of Oropharyngeal Burns
That being said, many clinicians would elect for EGD and assessment of airway with stridor alone. Do not be fooled into thinking if you see no oral lesions that there is no way the child ingested the caustic. Each case series showed a lack of correlation of physical exam findings to EGD findings.
Gaudrealt, 1983
Crain, 1984
Previtera, 1990
Category: Neurology
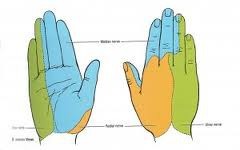
Keywords: hand examination, sensory function, median nerve, ulnar nerve, radial nerve (PubMed Search)
Posted: 8/25/2010 by Aisha Liferidge, MD
(Updated: 8/28/2014)
Click here to contact Aisha Liferidge, MD
-- ulnar nerve >>> supplies palmar surface and dorsal tips of little finger and medial half of ring finger, including
adjacent parts of hand.
-- median nerve >>> supplies palmar and dorsal aspects of thumb, index finger, middle finger, and lateral half
of ring finger, including adjacent parts of hand.
-- radial nerve >>> supplies most of dorsal surface of hand.
Category: Critical Care
Posted: 8/24/2010 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Hemostatic Therapy for ICH - Updated Guidelines
Morgenstern LB, et al. Guidelines for the management of spontaneous intracerebral hemorrhage. Stroke 2010;41:00-00.
Category: Vascular
Keywords: Aortic Dissection (PubMed Search)
Posted: 8/23/2010 by Rob Rogers, MD
(Updated: 2/8/2026)
Click here to contact Rob Rogers, MD
Beta Blockade in Treating Acute Aortic Dissection
Medical therapy for acute aortic dissection is aimed at decreasing shear stress within the aorta. Although there are many agents to choose from when treating hypertension in patients with acute aortic disease, all regimens should include a beta blocker (like esmolol) unless contraindicated. Initiation of a beta blocker before another antihypertensive agent is added is crucial as this will prevent reflex tachycardia associated with vasodilators and other afterload reducers. Reflex tachycardia may worsen the dissection.
Category: Cardiology
Keywords: hypercalcemia, hypocalcemia, electrocardiography (PubMed Search)
Posted: 8/22/2010 by Amal Mattu, MD
Click here to contact Amal Mattu, MD
typical ECG findings associated with hypercalcemia: short QT (e.g. QTc < 400 msec), ST-segment depression
typical ECG findings associated with hypocalcemia: prolonged QT
note that hyperkalemia is often associated with hypocalcemia, and as a result hyperkalemic patients often have a prolonged QT, but it's not the hyperkalemia that prolongs the QT, it's the hypocalcemia
Category: Orthopedics
Keywords: Rotator Cuff Tears, Chronic, Acute (PubMed Search)
Posted: 8/21/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Rotator Cuff Tears:
Four muscles make up the rotator cuff (SITS) which control internal and external rotation of the shoulder and abduct the shoulder.
Tears can be due to acute injuries (falls, heavy lifting, forceful abduction), though the majority (>90%) of rotator cuff tears are chronic in nature and due to subacromial impingement and decreased blood supply to the tendons.
Most patients can be treated with sling immobilization, NSAIDs and referral to sports medicine or orthopaedic surgeons. Elderly patients should be referred quickly as prolonged immobilization can lead to a frozen shoulder.
Category: Toxicology
Keywords: sulfonylureas,hypoglycemia (PubMed Search)
Posted: 8/19/2010 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
We will all get the patient presenting with low blood glucose on a regular basis. In general, barring any underlying infection, those who are insulin dependent can be corrected with IV dextrose and/or food and be discharged. Those on a sulfonylurea may experience repeated hypoglycemic episodes and require admission - perhaps even treatment with the antidote: octreotide.
Below is the duration of action and half-life of the sulfonylureas which illustrates the need for admission:
Duration of action is the physiologic effect whereas the half-life is the pharmacokinetics of elimination of the drug. Often these two numbers are different for drugs. Do not let the half-life fool you into thinking it is safe to discharge a hypoglycemic patient on a sulfonylurea.
