Category: International EM
Keywords: meningoccocus, Neisseria meningitidis, global, infectious disease (PubMed Search)
Posted: 11/20/2013 by Andrea Tenner, MD
(Updated: 2/27/2026)
Click here to contact Andrea Tenner, MD
General Information:
Nisseria meningitidis is the common culprit in epidemic meningitis. Serogroup B is currently causing an outbreak on the Princeton campus. So what are the serogroups and why are they important?
Six main serogroups cause disease: A, B, C, Y, X, W-135.
Two quadrivalent vaccines are currently licensed in the US that cover Serogroups A, C, Y, and W-135.
Relevance to the EM Physician: The currently available vaccines in the US cover the majority of serogroups of meningococcus, however, Serogroup B (currently causing an outbreak at Princeton) is not covered, nor is Serogroup X (for travelers to Sub-Saharan Africa).
Bottom Line: Serogroups B and X are not covered by the currently available vaccines in the US and at risk populations (and physicians treating those patients) should be made aware of the gap in coverage. Investigations for a vaccine for Serogroup B (licensed in Europe and Australia, but not in the US) are currently underway.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH, FACEP
Cohn A, MacNeil JR. Chapter 3: Infectious Diseases Related to Travel: Meningitis. Centers for Disease Control Yellow Book. 2014. Accessed at: http://wwwnc.cdc.gov/travel/yellowbook/2014/chapter-3-infectious-diseases-related-to-travel/meningococcal-disease on 20 Nov 2013.
Harrison LH. The Epidemiology of Meningococcal Disease in the United States. Clin Infect Dis. 2010 March 1; 50(S2):S37.
Meningococcal Disease in Other Countries. Center for Disease Control. Accessed at: http://www.cdc.gov/meningococcal/global.html on 20 Nov 2013.
National Travel Health Network and Centre. Meningitis Fact Sheet. Accessed at: http://www.nathnac.org/pro/factsheets/meningococcal.htm on 20 Nov 2013.
Category: Critical Care
Keywords: subarachnoid hemmorhage, sah (PubMed Search)
Posted: 11/19/2013 by Feras Khan, MD
(Updated: 2/27/2026)
Click here to contact Feras Khan, MD
Ottawa Rules for Subarachnoid Hemmorhage (SAH)
Background
Design
Results
132 (6.2%) had SAH
Decision rule including any:
Had 98.5% sensitivity (95% CI, 94.6%-99.6%) and 27.5% specificity (95% CI, 25.6%-29.5%)
Adding “thunder-clap” headache and “limited neck flexion on examination” (inability to touch chin to chest or raise the head 8cm off the bed if supine) resulted in 100% (95% CI, 97.2%-100%) sensitivity.
The rule was then evaluated using a bootstrap analysis on old cohort data to validate the rule.
Conclusion/Limitations
For alert patients older than 15 y with new severe nontraumatic headache reaching maximum intensity within 1 h
Not for patients with new neurologic deficits, previous aneurysms, SAH, brain tumors, or history of recurrent headaches (≥3 episodes over the course of ≥6 mo)
Investigate if ≥1 high-risk variables present:
Age ≥40 y
Neck pain or stiffness
Witnessed loss of consciousness
Onset during exertion
Thunderclap headache (instantly peaking pain)
Limited neck flexion on examination
Category: Visual Diagnosis
Posted: 11/18/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
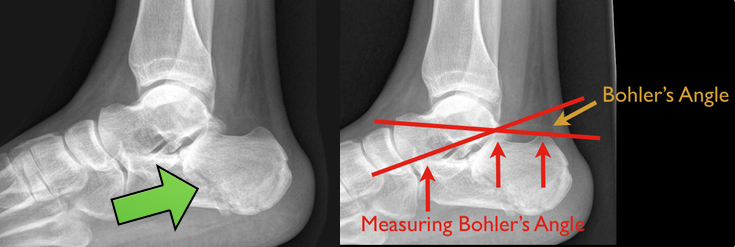
48 year-old presents after falling 15 feet following a “misunderstanding” with police. What's the diagnosis? ...and for a bonus question, why is this called a “Lover’s Fracture”?

Calcaneus fracture
Answer to Bonus Question: Historically called a “Lover’s Fracture” for “lovers” jumping out of bedroom windows (to evade suspicious spouses) who then land directly on their feet.
Calcaneus fractures
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Intra-Aortic Balloon Pump, Cardiogenic Shock (PubMed Search)
Posted: 11/15/2013 by Semhar Tewelde, MD
(Updated: 11/17/2013)
Click here to contact Semhar Tewelde, MD
Utility of Intra-Aortic Balloon Pump (IABP)
Kettner J, Sramko M, Holek M, et al. Utility of Intra-Aortic Balloon Pump Support For Ventricular Septal Rupture and Acute Mitral Regurgitation Complicating Acute Myocardial Infarction. American Journal of Cardiology. 2013 Vol 112 Issue 11 Pages 1709-1713
Category: Orthopedics
Keywords: Compartment Syndrome (PubMed Search)
Posted: 11/16/2013 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Compartment Syndrome
Compartment syndrome is classically described as having the 6 Ps:
The diagnosis of compartment syndrome can be difficult but ultimately it comes down to measuring the pressures in the area of concern. Various recommendations of the allowed pressure can be found, but in general a fasciotomy is not needed if the compartment pressure is 30 mmHg less then the diastolic pressure (The Delta 30). So if the patients diastolic pressure is 70, a fasciotomy is not need if the compartment pressure is less then 40.
Finally, if you are suspecting compartment pressure do NOT elevate the limb. Leave it in a dependent position to help improve blood flow into the limb.
Category: Pediatrics
Keywords: Intussusception, abdominal pain, fever (PubMed Search)
Posted: 11/10/2013 by Jenny Guyther, MD
(Updated: 11/16/2013)
Click here to contact Jenny Guyther, MD
Case: A 3 year 9 month female presents with fever to 39.4 C and intermittent abdominal pain worsening over 2 days. The patient had been tolerating food and had no change in her bowel habits. Based on the imaging below, what is your diagnosis and treatment?
Answer: Intussusception. This patient failed air reduction enema and was taken the OR. No bowel ischemia was found. The ilium was inside of the colon at the ileocecal valve. There was significant mesenteric lymphadenitis noticed. The patient recovered and was discharged later that day.
The x-ray above shows a soft tissue mass under the liver projection in the RUQ that can be suggestive of intussusception in the appropriate case. The second x-ray done during attempted air reduction shows air surrounding a dense area on the right side. Ultrasound, however, has become the gold standard. The ultrasound image shows the classic target sign of hyperechoic compressed loop of bowel telescoping within a hypoechoic edematous outer loop of bowel.
A few other important facts:
The median age of presentation is 32 months, with many presenting before 12 month.
Abdominal pain and/or crying was seen in 95% of cases. 66% had vomiting, 28% had fever, and 27% had bloody stools.
Causes included 29% with enlarged mesenteric lymph nodes (followed by GJ tube obstruction and meckels diverticulium)
30% have concurrent infections (URI and gastroenteritis being most common)
91% 1st time success rates with air contrast enema
*The above percentages were taken from the article referenced, which is a retrospective review done at a tertiary pediatric center.
Lochhead et al. Intussusception in children presenting to the emergency department. Clinical Pediatrics 2013 52:1029.
Category: Toxicology
Keywords: benzodiazepine, lorazepam, liver (PubMed Search)
Posted: 11/11/2013 by Bryan Hayes, PharmD
(Updated: 11/14/2013)
Click here to contact Bryan Hayes, PharmD
All benzodiazepines are metabolized by the liver. Some are just metabolized by pathways that are less dependent on global liver function.
The ‘LOT’ drugs are metabolized by conjugation, have no active metabolites, and have minimially affected half-lives even in the setting of liver disease.
L – Lorazepam
O – Oxazepam
T – Temazepam
The rest of the benzodiazepines are primarily metabolized via hepatic CYP-mediated oxidation and may have prolonged duration of effect in patients with marked liver impairment.
For a bit more detail and commentary by Dr. David Juurlink, please read my recent post on the Academic Life in Emergency Medicine blog: http://academiclifeinem.com/all-benzodiazepines-are-metabolized-by-the-liver/
Mihic SJ, Harris RA. Chapter 17. Hypnotics and Sedatives. In: Chabner BA, Knollmann BC, eds. Goodman & Gilman's The Pharmacological Basis of Therapeutics. 12nd ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=16663643. Accessed November 7, 2013.
Lee DC, Ferguson KL. Chapter 74. Sedative-Hypnotics. In: Lee DC, Ferguson KL, eds.Goldfrank's Toxicologic Emergencies. 9th ed. New York: McGraw-Hill; 2011. http://www.accesspharmacy.com/content.aspx?aID=6520459. Accessed November 7, 2013.
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Air transport, trauma, EMS (PubMed Search)
Posted: 11/13/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Helicopter EMS (HEMS) has rapidly grown over the past 30 years. HEMS is frequently used to transport trauma patients from the scene of a crash. The question is: for which trauma patients is HEMS most useful?
A recent article published in the Journal of the American Medical Association, based upon data from the National Trauma Data Bank (NTDB), looked at injured patients transported to a trauma center by helicopter versus ground ambulance. It showed that, after controlling for multiple known confounders, more severely injured patients had better outcomes when transported by helicopter than when transported by ground ambulances. Another recent article in the Journal of Trauma and Acute Care Surgery, again based upon the NTDB further showed that HEMS survival benefit seems to limited to individuals with physiologic instability.
Bottom Line:
Transport of severely injured trauma patients by helicopter versus ground from the scene of injury to a trauma center improved patient outcomes and decreased mortality. Transportation of stable, less injured patients by helicopter may actually worsen outcomes.
University of Maryland Section of Global Emergency Health
Author: Jon Mark Hirshon
Galvagno SM,Jr, Haut ER, Zafar SN, et al. Association between helicopter vs ground emergency medical services and survival for adults with major trauma. JAMA 2012;307:1602-10.
Ryb GE, Dischinger P, Cooper C, Kufera JA. Does helicopter transport improve outcomes independently of emergency medical system time? J Trauma Acute Care Surg. 2013 Jan;74(1):149-54.
Category: Critical Care
Posted: 11/12/2013 by Mike Winters, MBA, MD
(Updated: 2/27/2026)
Click here to contact Mike Winters, MBA, MD
Acalculous Cholecystitis in the Critically Ill
Rezende-Neto JB, et al. Abdominal catastrophes in the intensive care unit. Crit Care Clin 2013; 29:1017-44.
Category: Visual Diagnosis
Posted: 11/11/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
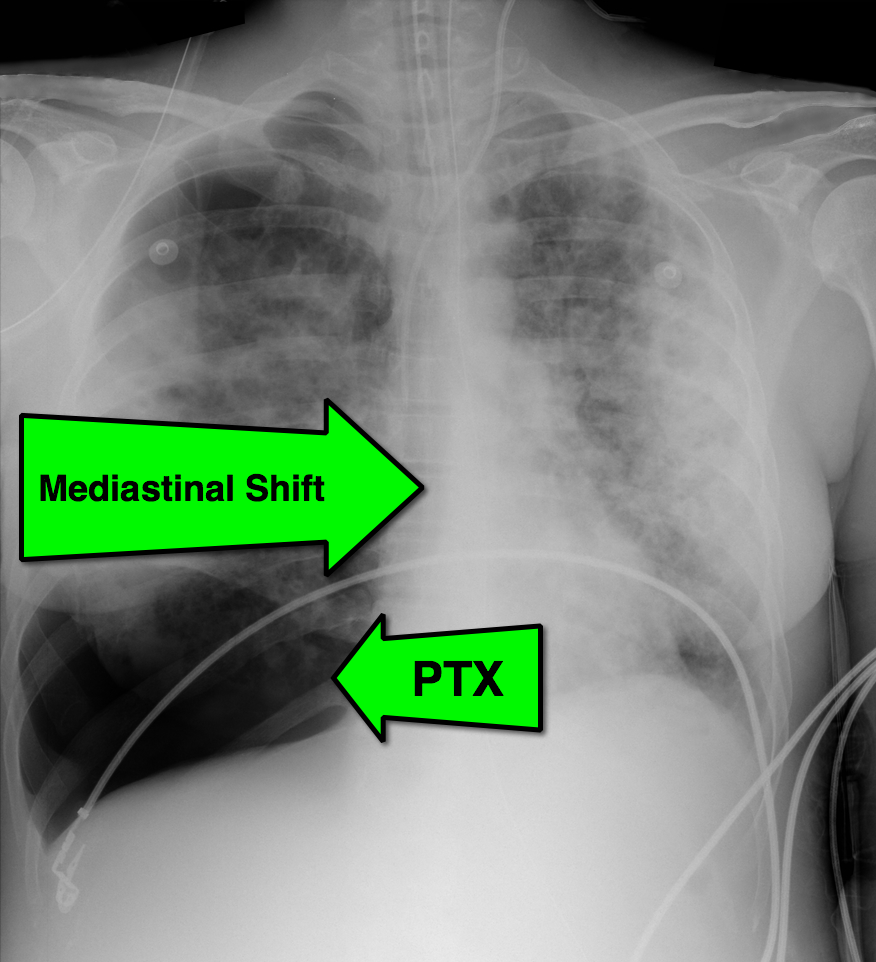
28 year-old cachectic female presents in respiratory distress and is immediately intubated on arrival to Emergency Department. What's the diagnosis and what are some potential etiologies?

Pneumothorax with mediastinal shift
Differential Diagnosis
The patient in this case had undiagnosed HIV/AIDS and presented with PTX secondary to PJP. The lifetime risk of PTX with HIV is 6% and 85% of those cases are secondary to PJP.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: AMI, LBBB, Sgarbossa criteria (PubMed Search)
Posted: 11/9/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Diagnosis of STEMI in patients with LBBB can be challenging. Guidelines that previously recommended emergent reperfusion for these patients have been reconsidered to avoid inappropriate cath lab activation and fibrinolytic therapy.
The 2013 ACC/AHA STEMI guidelines no longer consider new or presumably new LBBB a STEMI equivalent. This dramatic change may prevent inappropriate therapy for some, but fail to help identify patients with LBBB who are having STEMI's. Delayed reperfusion in this population could be fatal and is estimated to affect 5,000-10,000 patients per year in the US alone.
The Sgarbossa ECG criteria are the most validated tool to aid in the diagnosis of STEMI in the presence of LBBB. A Sgarbossa score of ≥ 3 has high specificity (>98%) and positive predictive value for acute MI and angiography-confirmed coronary occlusion. The following algorithm has been recently proposed to identify the high-risk population in which reperfusion therapy would be denied by the 2013 STEMI guidelines.
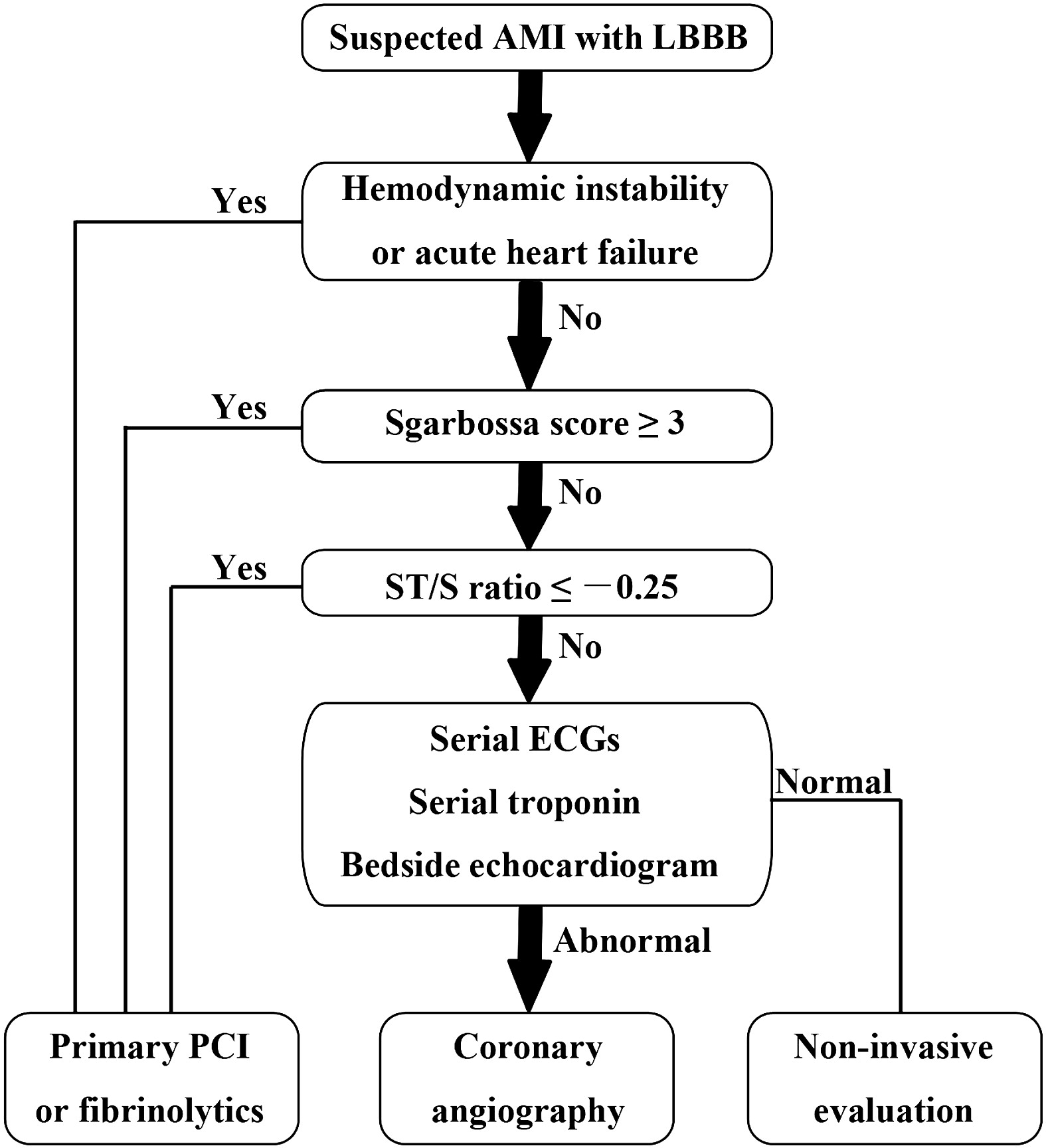
Watch this video to review Sgarbossa criteria and the modified Sgarbossa rule.
Want more emergency cardiology pearls? Follow me @alifarzadmd
The left bundle-branch block puzzle in the 2013 ST-elevation myocardial infarction guideline: From falsely declaring emergency to denying reperfusion in a high-risk population. Are the Sgarbossa Criteria ready for prime time? American Heart Journal. 2013;166(3):409–413.
Category: Orthopedics
Keywords: back pain, cauda equina (PubMed Search)
Posted: 11/4/2013 by Brian Corwell, MD
(Updated: 11/9/2013)
Click here to contact Brian Corwell, MD
Cauda equina syndrome results from compression of multiple lumbar and sacral nerve roots
Causes: Central disc herniation, spinal epidural abscess, malignancy, trauma, hematoma.
Consider this entity in those with back pain and radiculopathy at multiple spinal levels
Urinary retention occurs in >90% of patients
Saddle anesthesia occurs in 75%
Decreased rectal sphincter tone occurs in 60 to 80%
A post void residual volume <100 mL makes this entity very unlikely
Category: Pharmacology & Therapeutics
Keywords: Cephalosporin,penicillin,anaphylaxis,urticaria,cross sensitivity (PubMed Search)
Posted: 11/7/2013 by Ellen Lemkin, MD, PharmD
(Updated: 2/27/2026)
Click here to contact Ellen Lemkin, MD, PharmD
When patients with severe allergies to penicillin (urticarial, bronchospasm, anaphylaxis, angioedema) are excluded, the cross reactivity to cephalosporins is very low (approximately 0.1%)
The reaction is related to structures in the side chain, not the cyclical structure as thought in the past.
There are several cephalosporins with IDENTICAL side chains that should not be given to patients with allergies to specific penicillins, namely:
The Medical Letter on Drugs and Therapeutics • December 24, 2012 (Issue 1406) p. 101.
Category: International EM
Keywords: MERS-CoV, Viral Illness, Respiratory (PubMed Search)
Posted: 11/6/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Case Presentation:
A 56y/o man with diabetes presents with fever, cough, and diarrhea x 2 days.
V/S: T:38.7 BP:165/88 P: 105 R:24 O2 sat:91% on room air
CXR: left lower lobe infiltrate.
On further history you learn he has just returned from visiting family in Saudi Arabia 7 days ago. While there, he visited a cousin that was ill.
Clinical Question:
Should this patient be isolated for Middle Eastern Respiratory Syndrome – Corona Virus (MERS-CoV)?
Answer:
Yes, there are 150 cases to date and 64 have died. None confirmed in the US yet but 6 confirmed in Europe.
Patients who should be isolated in an airborne iso room with N95 mask use (similar to TB) are:
Patients with fever + pneumonia/ARDS AND one of the following:
Bottom Line:
In patients with febrile respiratory illness requiring hospitalization and recent travel to the Arabian Peninsula: isolate for MERS-CoV and contact the health department.
University of Maryland Section of Global Emergency Health
Author: Jenny Reifel Saltzberg
Assiri A, et al. Epidemiological, demographic, and clinical characteristics of 47 cases of Middle East respiratory syndrome coronavirus disease from Saudi Arabia: a descriptive study. Lancet Infect Dis. 2013 Sep;13(9):752-61.
Category: Critical Care
Keywords: Mechanical ventilation, Critical Care, Intubation (PubMed Search)
Posted: 10/29/2013 by John Greenwood, MD
(Updated: 11/5/2013)
Click here to contact John Greenwood, MD
Ineffective triggering is the most common type of ventilator dyssynchrony. The differential diagnosis includes:
Auto peep is the most common cause of ineffective triggering and will often occur as a patient cannot create enough inspiratory force to overcome their own intrinsic peep (PEEPi). Patients who are severely tachypnic or those with obstructive lung disease are at high risk for auto peep (not enough time to exhale).
Ineffective triggering can also occur if the patient cannot create enough of a negative inspiratory force to trigger the vent to deliver a positive pressure breath. Prolonged period of mechanical ventilation, over sedation, high cervical spine injuries, or diaphragmatic weakness are common causes.
Lastly, improper trigger sensitivities may make it difficulty for the ventilator to sense when the patient is attempting to take a spontaneous breath.
For an example of a patient with ineffective triggering, check out: http://marylandccproject.org/2013/10/28/vent-problems1/
Category: Visual Diagnosis
Posted: 11/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
This week's visual pearl reviews the structures of the heart when being viewed in a parasternal long-axis view. What do the labels correspond to in the clip below (note: "E" and "F" are valves) and do you see any obvious abnormalities?
The parasternal long-axis is obtained by scanning to the left (patient's left) of the sternum through the 2nd-5th intercostal space. Click here for a tutorial on the technique.
Answer to Bonus Question: Dilation of the RVOT
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 11/3/2013 by Semhar Tewelde, MD
(Updated: 11/16/2013)
Click here to contact Semhar Tewelde, MD
Secondary Prevention in AMI
Just as aspirin is pivotal in the treatment of acute coronary syndrome, medications such as beta-blocker, statins, and angiotensin-converting enzyme inhibitors have been proven to be essential in secondary prevention of AMI.
Patients after AMI are typically discharged on appropriate secondary prevention medications; however the prescribed doses are often far below the proven efficacy based on clinical trials.
A review of 6,748 patients from 31 hospitals enrolled in 2 U.S. registries (2003 to 2008) illustrated that only 1 in 3 patients were prescribed these medications at goal doses.
Of patients not discharged on goal doses, up-titration during follow-up occurred infrequently ~25%.
Optimal medication dosing and appropriate titration is integral to prevention of further morbidity and mortality.
Arnold S, Spertus J, Masoudi F, et al. Beyond Medication Prescription as Performace Measure: Optimal Secondary Prevention Dosing After Acute Myocardial Infarction. JACC Nov 5, 2013 Vol 62:19;1791-1801
Category: Pharmacology & Therapeutics
Keywords: contrast-induced nephropathy, n-acetylcysteine, NAC (PubMed Search)
Posted: 10/31/2013 by Bryan Hayes, PharmD
(Updated: 11/2/2013)
Click here to contact Bryan Hayes, PharmD
A recent meta-analysis has called into question whether contrast-induced AKI even occurs after an IV dye load for radiologic imaging. [1] This conclusion is most certainly up for debate.
Irrespective of that conclusion, prevention of contrast-induced nephropathy is still important. Is there any benefit to using N-acetylcysteine over normal saline in the ED? Probably not according to a new study. [2]
Conclusions
Follow me on Twitter (@PharmERToxGuy)
Category: Pediatrics
Keywords: cough, upper respiratory infection, children, honey (PubMed Search)
Posted: 11/1/2013 by Danielle Devereaux, MD
Click here to contact Danielle Devereaux, MD
How many times have you been frustrated in the peds ED when you have a child with a URI that has a significant night time cough and you feel like you have nothing to offer them for symptom control? The parent is frustrated because the child is not sleeping which means they are not sleeping and they are looking at you for help. We all know that OTC cough and cold medications are not helpful and may be harmful in children <2 yrs old and should be used with caution in children <6 yrs old. So what can you do? You can recommend a course of HONEY at night. Of course this does not apply to children < 1 yr who are at increased risk of botulism. A recent double-blind placebo-controlled trial published in Pediatrics in 2012 demonstrated reduced night time cough and subjective improved sleep quality in children age 1-5 who were given honey compared to placebo. This study supports previous less rigorous publications that found honey was an effective remedy on cough in children. Mechanism for honey's beneficial effect on cough is unknown but possibly related to close anatomic relationship between sensory nerve fibers that initiate cough and gustatory nerve fibers that taste sweetness. Of note, a recently published survey in Pediatric Emergency Care revealed that 2/3 of parents were unaware of the FDA guidelines regarding OTC cough and cold remedies in children! After you recommend HONEY for night time cough, take an extra minute and educate your parents about the potential dangers of cough and cold medicines in small children!
Cohen A, Rozen J, Kristal H, et al. Effect of honey on nocturnal cough and sleep quality: a double-blind, randomized, placebo-controlled study. Pediatrics. 2012; 130(2): 465-471.
Varney SM, et al. Pediatr Emerg Care. 2012; 28(9): 883-885
Food and Drug Administration. Using Over-The-Counter Cough and Cold Products in Children. Available at http://www.fda.gov/ForConsumers/ConsumerUpdates/ucm048515.htm
Category: Toxicology
Keywords: glycyrrhizic acid, licorice (PubMed Search)
Posted: 10/31/2013 by Fermin Barrueto
(Updated: 2/27/2026)
Click here to contact Fermin Barrueto
You have a treat bag full of candy, which one can cause hypertension, hyopkalemia, metabolic alkalosis, rhabdomyolysis, low renin activity, thrombocytopenia and hypoaldosteronism. (scroll down for answer)
Licorice syrup or licorice extract contains glycyrrhizic acid which has a mineralcorticoid-like effect and can cause of all of the effects. Don't worry, Twizzlers and other usual licorice candies do not have true licorice extract in them. It is found in herbal remedies and some "natural" candies and licorice flavored cigars. Don't pick the licorice !
