Category: Pediatrics
Posted: 12/13/2013 by Rose Chasm, MD
(Updated: 2/27/2026)
Click here to contact Rose Chasm, MD
Wang CJ, et al. Quality-of-care indicators for children with sickle cell disease. Pediatrics. 2011;128:484.
Berini JC, et al. Fatal hemolysis induced by Ceftriaxone in a child with sickle cell anemia. 1995;126:813.
Category: Toxicology
Keywords: acetaminophen, Rumack-Matthew nomogram (PubMed Search)
Posted: 12/7/2013 by Bryan Hayes, PharmD
(Updated: 12/12/2013)
Click here to contact Bryan Hayes, PharmD
Can acetaminophen concentrations < 100 mcg/mL obtained between 1-4 hours after acute ingestion accurately predict a nontoxic 4-hour concentration? NO!
Despite a high negative predictive value, a new study found there are still cases with toxic concentrations after 4 hours despite earlier levels < 100 mcg/mL.
The Rumack-Matthew nomogram is to be utilized starting at 4 hours after an acute acetaminophen ingestion. Unless the concentration is zero, a second level must be drawn at 4 hours if an earlier one is positive.
Froberg BA, et al. Negative predictive value of Acetaminophen concentrations within four hours of ingestion. Acad Emerg Med 2013;20(10):1072-5. [PMID 24127715]
Rhyee SH. Early serum acetaminophen levels: how soon is too soon? Acad Emerg Med 2013;20(10):1070-1. [PMID 24127714]
Follow me on Twitter (@PharmERToxGuy)
Category: International EM
Keywords: Chikungunya, Virus, International, (PubMed Search)
Posted: 12/11/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Clinical Presentation:
Diagnosis
Treatment
Bottom line:
Chikungunya virus can cause symptoms similar to dengue fever but is not as deadly. This week the first cases of CHIKV were reported in the Caribbean. Consider this in travelers returning from endemic areas.
Distinguishing features:
University of Maryland Section for Global Emergency Health
Author: Andi Tenner, MD, MPH, FACEP
http://www.cdc.gov/chikungunya/pdfs/CHIKV_Clinicians.pdf
http://www.thedailyherald.com/index.php?option=com_content&view=article&id=44572
Category: Critical Care
Posted: 12/10/2013 by Mike Winters, MBA, MD
(Updated: 2/27/2026)
Click here to contact Mike Winters, MBA, MD
The Concentrated Overview of Resuscitative Efforts (CORE) Scan
Wu TS. The CORE Scan. Crit Care Clin 2014; 30:151-75.
Category: Visual Diagnosis
Posted: 12/9/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
37 year-old male presents with cough and a fever. What's the diagnosis and name three risk factors assiciated with disease?
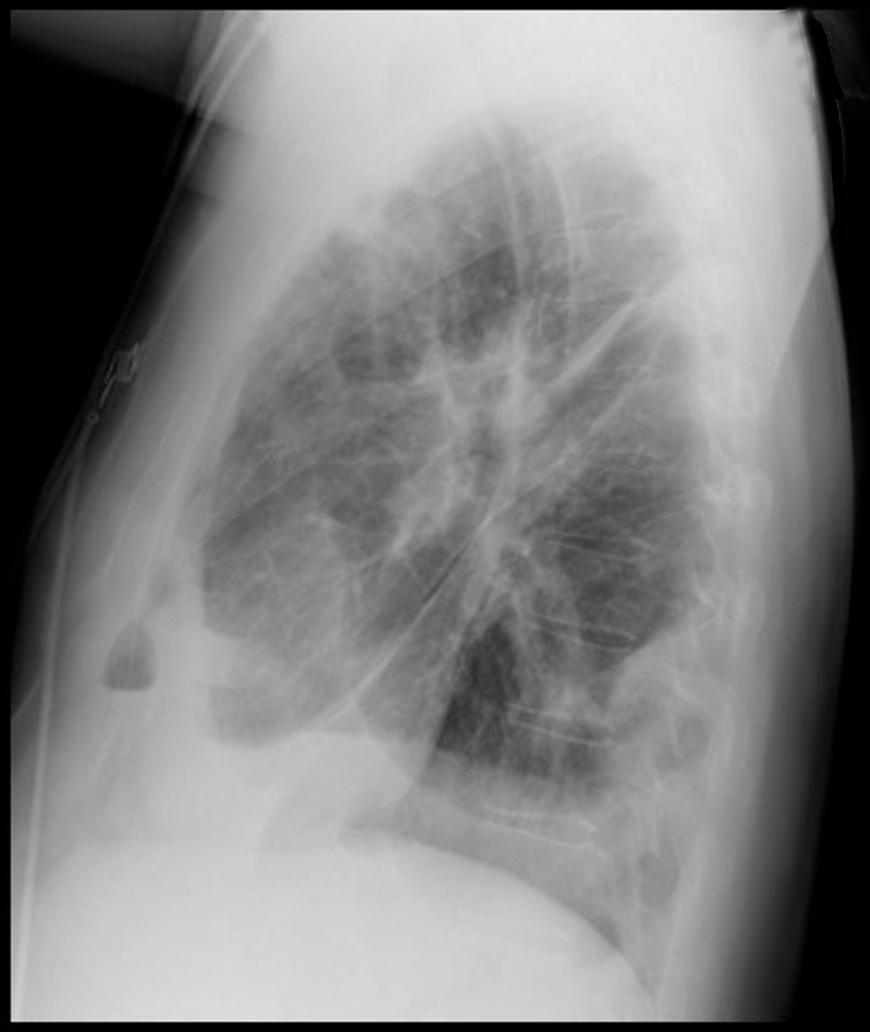
Answer: Lung Abscesses
Lung Abscess
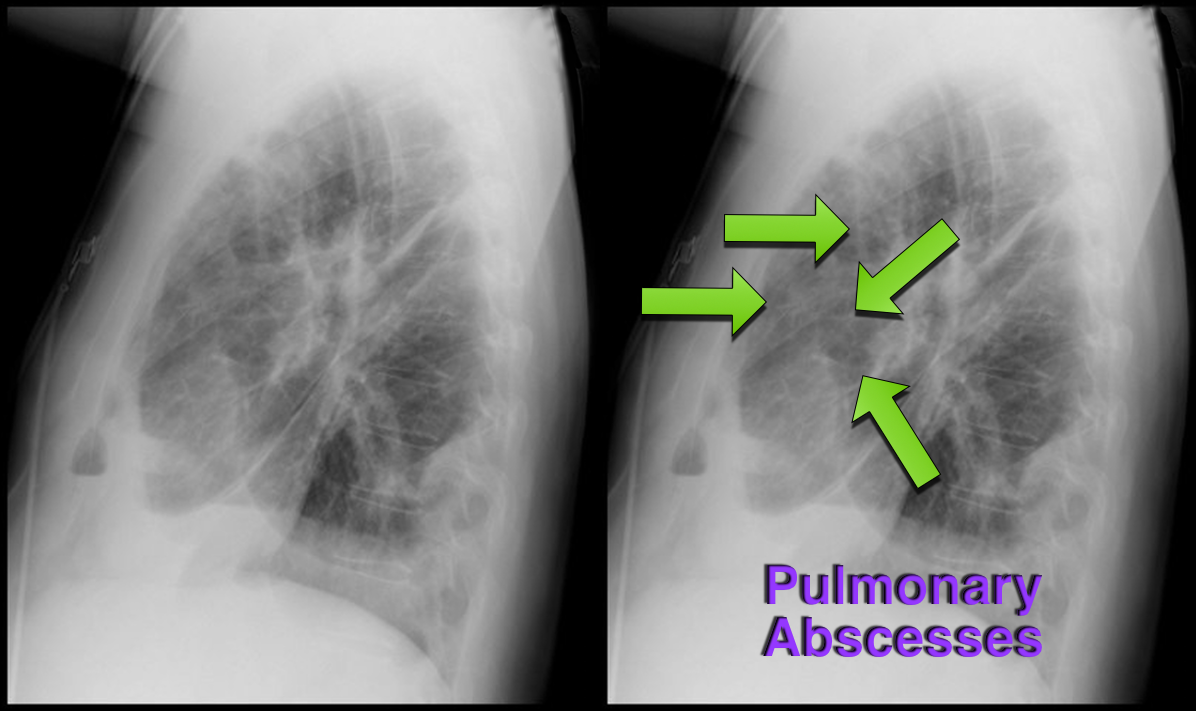
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: ACS, Chest Pain, HEART score (PubMed Search)
Posted: 12/8/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Bottom-line: The HEART score can help to objectively risk stratify ED patients with chest pain into low, intermediate, and high risk groups. Using the HEART score can also facilitate more efficient and effective communication with colleagues.
Want more emergency cardiology pearls? Follow me @alifarzadmd
Backus BE, Six AJ, Kelder JC, et al. A prospective validation of the HEART score for chest pain patients at the emergency department. International Journal of Cardiology. 2013;168(3):2153–2158.
Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. 2008;16(6):191–196.
Category: Pharmacology & Therapeutics
Keywords: healthcare-associated pneumonia, HCAP, atypical, macrolide, fluoroquinolone (PubMed Search)
Posted: 12/2/2013 by Bryan Hayes, PharmD
(Updated: 12/7/2013)
Click here to contact Bryan Hayes, PharmD
In a potentially ground breaking study of healthcare-associated pneumonia (HCAP) patients, atypical pathogens were identified in 10% of cases!
Application to clinical practice: Add atypical coverage with a macrolide or respiratory fluoroquinolone for HCAP patients who have been in the community for any length of time.
The study also identified HCAP patients who may not require 3 'big gun' broad-spectrum antibiotics. This is a practice changing article for ED providers. For more analysis of the study, please note the bonus reading links below.
Bonus reading:
Dr. Emily Heil (@emilylheil) analyzes the full study in more depth at Academic Life in Emergency Medicine: http://academiclifeinem.com/new-treatment-strategy-not-so-sick-health-care-associated-pneumonia/
Dr. Ryan Radecki (@emlitofnote) critiques the study at Emergency Medicine Literature of Note: http://www.emlitofnote.com/2013/10/down-titrating-antibiotics-for-hcap.html
Maruyama T, et al. A new strategy for healthcare-associated pneumonia: a 2-year prospective mulitcenter cohort study using risk factors for multidrug-resistant pathogens to select initial empiric therapy. Clin Infect Dis 2013;57(10):1373-83. [PMID 23999080]
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: oral anticoagulant,edoxaban,atrial fibrillation,stroke,Xa (PubMed Search)
Posted: 12/5/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
It has linear, predictable pharmacokinetics, achieves maximal concentration within 1-2 hours, is 50% renally excreted, and has a half life is 9-11 hours.
Edoxaban was evaluated in a recent trial comparing warfarin in patients with atrial fibrillation.
The primary end point or first stroke or systemic pulmonary embolic event occurred in 1.5% with warfarin, compared with 1.18% in the high dose edoxaban (HR 0.79; 97.5% CI 0.63-0.99, P<0.001). In the intention to treat there were trends favoring high dose edoxaban and unfavorable trends with the lower dose.
The principal safety end point of major bleeding occurred in 3.43% with warfarin versus 2.75% with high dose edoxaban (HR 0.86; 95% CI 0.71-0.91, P<0.001).
Bottom line: Both high dose (60 mg) and low dose (30 mg) edoxaban were non-inferior to warfarin with prevention of stroke or systemic emboli, and were associated with significantly lower rates of bleeding and death from cardiovascular causes.
Currently it is approved for use in Japan.
Edoxaban versus Warfarin in Patients with Atrial Fibrillation. Giuliano, RP et al. NEJM Nov 28, 2013; 369(22):2093-2104.
Category: International EM
Keywords: Vaccine, Meningitis, Neisseria meningitidis, Outbreak (PubMed Search)
Posted: 12/4/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Fever and headache or rash in those with close contacts from the affected universities should be considered for rapid, empiric meningococcal treatment.
CDC Health Alert Network, Nov. 27, 2013 http://emergency.cdc.gov/HAN/han00357.asp
Category: Critical Care
Keywords: Mechanical Ventilation, autoPEEP, PEEP, obstructive lung disease, critical care (PubMed Search)
Posted: 12/2/2013 by John Greenwood, MD
(Updated: 12/3/2013)
Click here to contact John Greenwood, MD
Vent Management: Finding the AutoPEEP!
OK, so we all know not to, "...Fall asleep on Auto-PEEP" thanks to Dr. Mallemat's pearl that can be seen here. But now the question is, how do you know if your patient is air-trapping?
There are 3 ways you can look for evidence of Auto-PEEP on the ventilator:
Blanch L, Bernabé F, Lucangelo U. Measurement of air trapping, intrinsic positive end-expiratory pressure, and dynamic hyperinflation in mechanically ventilated patients. Respir Care. 2005;50(1):110-23.
Category: Visual Diagnosis
Posted: 12/2/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Which view of the heart is this and can you name the structures from A-G?
1. Subcostal or Subxiphoid view; this view is obtained by placing the probe under the ribs with the patient supine. The liver is used as an acoutic window to image the heart.
2. Name the items labeled A-G:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Cardiac Transplant (PubMed Search)
Posted: 12/1/2013 by Semhar Tewelde, MD
(Updated: 8/28/2014)
Click here to contact Semhar Tewelde, MD
ECG Following Cardiac Transplant
Chou's Electrocardiography in Clinical Practice: Adult and Pediatric 6th Edition
Category: Orthopedics
Keywords: Posterior, Dislocation, Shoulder (PubMed Search)
Posted: 11/30/2013 by Michael Bond, MD
(Updated: 2/27/2026)
Click here to contact Michael Bond, MD
Posterior Shoulder Dislocations

(A posterior shoulder dislocation will show the humeral head displayed superiorly in the image away from the clavicle which is the inferior most bone)
Some things to look for on the AP view that will suggest a posterior shoulder dislocation:
Life in the Fast Lane as a great discussion of posterior shoulder dislocations at http://lifeinthefastlane.com/posterior-shoulder-dislocation/
Best way to make the diagnosis --- suspect it and get an axillary view.
Category: International EM
Keywords: Pediatric, Trauma, Ultrasound, Abdomen, International (PubMed Search)
Posted: 11/27/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Bottom Line: In a stable pediatric abdominal trauma victim, combined FAST and LFT results are an effective screening tool to evaluate for intra-abdominal injury.
Kenefake et al, Pediatric Emergency Medicine Nuances in Pediatric Truama. Emergency Medicine Clinics of North America, August 2013, 31;3:627-652
Krug E. Injury: a leading cause of the global burden of disease. Geneva: World Health Organization; 1999 (WHO/HSC/PVI/99.11).
Retzlaff et al, Is sonography reliable for the diagnosis of pediatric blunt abdominal trauma. J of Ped Surg 2010; 45: 912-915
Sola et al, Pediatric FAST and Elevated Liver Transaminases: An Effective Screening Tool in Blunt Abdominal Truama. J of Surgical Research 2009; 157;1: 103-107
Category: Critical Care
Posted: 11/26/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
The management of alcohol withdrawal syndrome (AWS) includes supportive care focusing on the ABC’s and administration of benzodiazepines (BDZ).
While BDZ are effective in the treatment of AWS, some patients may require very high doses of BDZ to control symptoms (tachycardia, hypertension, diaphoresis, etc.); unfortunately, high-doses of BDZ may lead to suppression of the respiratory drive and endotracheal intubation.
Dexmedetomidine (DEX) is a sedative agent that is an intravenous alpha2-agonist (it's like clonidine); it reduces sympathetic outflow from the central nervous system and it may help treat withdrawal syndromes. The major benefit of DEX is that it does not suppress the respiratory drive, thus intubation is not required.
Smaller trials and case series have shown that patients with AWS who were treated with BDZ in addition to DEX had better symptom control, lower overall BDZ doses, and less respiratory depression/intubation.
Bottom-line: While more trials are needed, consider adding DEX for patients with AWS who require high-doses of BDZ.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 11/25/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
What view of the heart is this and can you name everything from A-G?
1. Apical-four chamber view; this view is obtained by placing the probe in the 4-5th intercostal space at the anterior axillary-line. The patient can be placed in left lateral decubitus to improve imaging.
2. Name the items labeled A-G:
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Therapeutic Hypothermia, ROSC, Cardiac Arrest, Resuscitation (PubMed Search)
Posted: 11/23/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Want more emergency cardiology pearls? Follow me @alifarzadmd
Category: Orthopedics
Keywords: bronchospasm, asthma, exercise-induced laryngeal obstruction (PubMed Search)
Posted: 11/23/2013 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Unexplained respiratory symptoms during exercise are often incorrectly considered secondary to exercise induced asthma/bronchospasm.
An important diagnosis on the differential should be exercise-induced laryngeal obstruction (EILO).
Of 91 athletes referred for asthma workup, 35% had EILO.
The presence of inspiratory symptoms did not differentiate athletes with and without EILO.
61% of athletes with EILO used regular asthma medication at referral.
Category: Pediatrics
Keywords: trauma, cardiac arrest, return of spontaneous circulation (PubMed Search)
Posted: 11/22/2013 by Mimi Lu, MD
Click here to contact Mimi Lu, MD
Category: Toxicology
Keywords: rivaroxaban, dabigatran (PubMed Search)
Posted: 11/21/2013 by Fermin Barrueto
(Updated: 2/27/2026)
Click here to contact Fermin Barrueto
Reversal of the new anticoagulants rivaroxaban (Xarelto) and dabigatran (Pradaxa) has been challenging particularly in the ED setting with no definitive reversal agent. Intracerebral hemorrhage or critical GI bleed management becomes challenging and worsens mortality.
There is growing literature that states activated prothrombin complex concentrate or non-activated PCC may reverse these new anticoagulants. A volunteer study (1) showed its efficacy and concensus workgroups are now recommending aPCC as first line therapy(2). The search goes on for a reliable reversal agent for these new anticoagulants which were suppose to solve more problems instead of create new ones.
1) Eerenberg ES, Kamphuisen PW, Sijpkens MK, Meijers JC, Buller HR, Levi M. Reversal of rivaroxaban and dabigatran by prothrombin complex concentrate: a randomized, placebo-controlled, crossover study in healthy subjects. Circulation. 2011 Oct 4;124(14):1573-9. 2) Pernod G, Albaladejo P, Godier A, Samama CM, Susen S, Gruel Y, Blais N, Fontana P, Cohen A, Llau JV, Rosencher N, Schved JF, de Maistre E, Samama MM, Mismetti P, Sié P; Working Group on Perioperative Haemostasis. Management of major bleeding complications and emergency surgery in patients on long-term treatment with direct oral anticoagulants, thrombin or factor-Xa inhibitors: proposals of the working group on perioperative haemostasis (GIHP) - March 2013. Arch Cardiovasc Dis. 2013 Jun-Jul;106(6-7):382-93.
