Category: Visual Diagnosis
Posted: 10/7/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
25 year-old female struck in the left hand by a football. Presents with pain, visible deformity, and the Xray below. What are the next step(s) in management?

Dorsal Metacarpophalangeal (MCP) Dislocation

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: Aortic Syndrome, Aortic Dissection, Intramural hematoma, Atheromatous ulcer (PubMed Search)
Posted: 10/6/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Acute Aortic Syndromes
Classically, aortic dissection is considered the primary culprit in patients with chest pain that radiates to the back (aortic pain) or chest pain combined with ischemia (cerebral, cardiac, peripheral), syncope, or cardiac arrest. However, it should not be your only concern: the rate of aortic rupture is much higher in penetrating atheromatous ulcer (42%) and intramural hematoma (35%) than in aortic dissection (types A 7.5% and type B 4.1%).
Chest pain with concomitant ischemic symptoms and acute decompensation should prompt consideration of several etiologies under the umbrella of aortic syndromes and not limited to dissection :
Sheikh A, Ali K, Mazhar S. Acute Aortic Syndrome. Circulation 2013;128:1122-1127
Coady MA, Rizzo JA, Elefteriades JA. Pathological Variants of thoracic aortic dissection. Penetrating atherosclerotic ulcers and intramural hematomas. Cardiol Clin. 1999;17:637-657
Category: Pharmacology & Therapeutics
Keywords: cryptococcal, meningitis, amphotericin, flucytosine (PubMed Search)
Posted: 9/25/2013 by Bryan Hayes, PharmD
(Updated: 10/5/2013)
Click here to contact Bryan Hayes, PharmD
Treatment of patients with HIV/AIDS can frequently mean consideration for, and need to treat cryptoccocal meningitis.
Since 1997, studies have demonstrated that high-dose Amphotericin B combined with flucytosine has improved outcomes compared to low dose treatment or monotherapy.
A recent 2013 study reiterated this approach, showing significant decrease in deaths at 70 days post-treatment and increased rates of yeast clearance with combination therapy of Amphotericin B plus flucytosine.
Recommendation:
Antifungal treatment of cryptococcal meningitis should start with Amphotericin B at 0.7-1 mg/kg IV daily plus concurrent flucytosine 25 mg/kg orally q6 hours. Fluconazole can be substituted in place of flucytosine if it is not available or not tolerated.
Category: Pediatrics
Keywords: Omphalitis, necrotizing fasciitis, umbilical cord (PubMed Search)
Posted: 10/4/2013 by Joey Scollan, DO
Click here to contact Joey Scollan, DO
Should you be concerned about erythema around the umbilical stump?!
Yes!
Often parents will bring their neonate to the ED with concerns about the umbilical cord and it is just a simple granuloma or normal detachment. But is it omphalitis???
Omphalitis incidence is low in developed countries, but that means it’s easier, and no less catastrophic, to miss!
Omphalitis is a superficial cellulitis of the umbilical cord, but 10-16% progress to necrotizing fasciitis of the abdominal wall!!!
Always ADMIT and consider consulting surgery early in case of rapid progression…
Most often polymicrobial and should be treated with:
Should notice improvement within 12-24 hours, so if don’t or begin to observe
CONSULT SURERY for concern of necrotizing fasciitis which has a mortality rate of close to 60%!!!
Category: Pharmacology & Therapeutics
Keywords: procainamide,atrial fibrillation,prolonged QT,monomorphic VT (PubMed Search)
Posted: 10/3/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
ACLS recommendation for procainamide in tachycardic rhythms is:
Loading dose 20 mg/minute (up to 50 mg/minute for more urgent situations) until:
Maintenance infusion is 1 to 4 mg/min.
An easier method for dosing acute onset atrial fibrillation in stable patients was used in the Ottawa Aggressive Protocol, in which they administered 1 gm over 60 min, which was interrupted if BP < 100 mmHg; if corrected by a 250 ml IV bolus, the infusion was resumed. This was not used, however if the patient was to be admitted.
A strategy for treating stable monomorphic VT with procainamide used:
100 mg IV over 1-2 minutes, repeat as necessary until an endpoint of
If no slowing of the tachycardia occurred with a dose of 400 mg, the administration was ceased.
1. Steil IG, Clement CM, Perry JJ et al. Association of the Ottawa Aggressive Protocol with rapid discharge of emergency department patients with recent-onset atrial fibrillation or flutter. CJEM 2010;12(3):181-91.
2. Komura S, Chinushi M, Furushima H. et al. Efficacy of Procainamide and Lidocaine in Terminating Sustained Monomorphic Ventricular Tachycardia. Circulation May 2010 Vol 72
Category: International EM
Keywords: Malaria, Pediatrics, Quinine, Drug Reaction (PubMed Search)
Posted: 10/2/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Case Presentation:
You are working in an ED in Houston when a 2 year old girl presents with fever for one day and decreased po intake. On arrival her temp=103, HR=180, and RR=50 SaO2=100%. She was born in the US and is up to date on all of her vaccinations, but has just returned from a trip to Liberia where she was visiting her extended family and received multiple mosquito bites. Physical exam, CXR and urinalysis are otherwise unremarkable and you suspect malaria, based on her history. You start quinine IV while you are waiting for the smear when suddenly the child becomes unresponsive.
Clinical Question:
What is the next investigation you should perform?
Answer:
Rapid blood glucose!
This patient has at least 4 reasons to be hypoglycemic:
1. fasting (Kids can become hypoglycemic from fasting alone in ~24hrs)
2. infection (any infectious disease can cause it, esp in kids <3 yrs old)
3. malaria (thought to be due in part to increased consumption by parasite)
4. quinine (stimulates insulin release)
Bottom Line:
Kids can become hypoglycemic fast—check a blood glucose in all pre-pubertal sick children.
University of Maryland Section of Global Emergency Health
Author: Andi Tenner, MD, MPH
Zijlmans WCWR et al. Glucose metabolism in children: influence of age, fasting, and infectious diseases. Metabolism Clinical and Experimental. 2009. 58:1356-1365.
Category: Critical Care
Posted: 9/30/2013 by Haney Mallemat, MD
(Updated: 10/1/2013)
Click here to contact Haney Mallemat, MD
The efficacy of epinephrine during out-of hospital cardiac arrest has been questioned in recent years, especially with respect to neurologic outcomes (ref#1).
A recent study demonstrated both a survival and neurologic benefit to using epinephrine during in-hospital cardiac arrest when used in combination with vasopressin and methylprednisolone.
Researchers in Greece randomized 268 consecutive patients with in-hospital cardiac arrest to receive either epinephrine + placebo (control group; n=138) or vasopressin, epinephrine, and methylprednisolone (intervention arm; n=130)
Vasopressin (20 IU) was given with epinephrine each CPR cycle for the first 5 cycles; Epinephrine was given alone thereafter (if necessary)
Methylprednisolone (40 mg) was only given during the first CPR cycle.
If there was return of spontaneous circulation (ROSC) but the patient was in shock, 300 mg of methylprednisolone was given daily for up to 7 days.
Primary study end-points were ROSC for 20 minutes or more and survival to hospital discharge while monitoring for neurological outcome
The results were that patients in the intervention group had a statistically significant:
probability of ROSC for > 20 minutes (84% vs. 66%)
survival with good neurological outcomes (14% vs. 5%)
survival if shock was present post-ROSC (21% vs. 8%)
better hemodynamic parameters, less organ dysfunction, and better central venous saturation levels
Bottom-line: This study may present a promising new therapy for in-hospital cardiac arrest and should be strongly considered.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 9/29/2013 by Haney Mallemat, MD
(Updated: 9/30/2013)
Click here to contact Haney Mallemat, MD
65 year-old diabetic patient presents with abdominal pain. What's the abnormality on Xray?

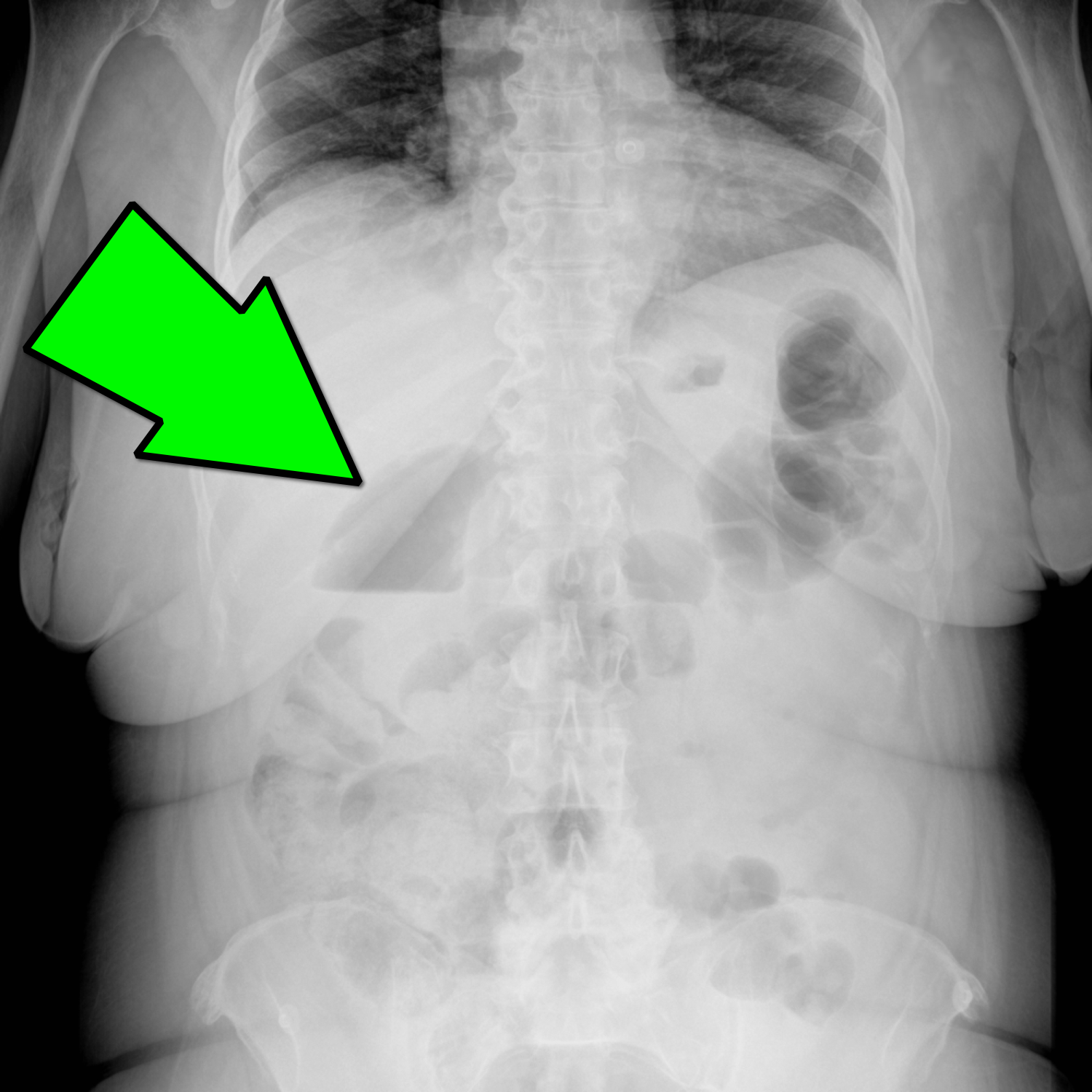
Emphysematous Cholecystitis
Emphysematous Cholecystitis
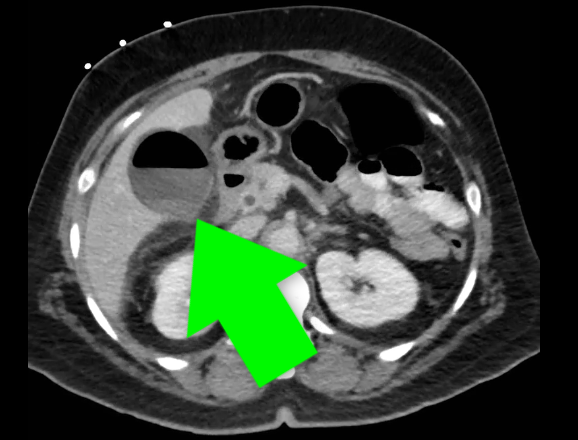
Carrascosa MF, et al. Emphysematous Cholecystitis. CMAJ.10 Jan 2012; 184(1): E81
Category: Cardiology
Posted: 9/29/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
The primary goal in management of STEMI is rapid coronary revascularization. STEMI's are occasionally complicated by ventricular fibrillation (VF) arrest. High quality chest compressions and early defibrillation will improve survival. But what can be done in cases where conventional ACLS measures fail and patients have shock-refractory VF?
Some have suggested that emergent PCI with ongoing CPR en route may be beneficial. This option may be considered in close consultation with cardiology if the arrest is thought to be driven by ongoing ischemia and infarction. However, definitive data is lacking and this has only been described in a handful of case reports.
There may also be a role for venoarterial ECMO to aid in perfusion of vital organs and limit the risk of multisystem organ failure. The ECMO circuit can also help facilitate therapeutic hypothermia after the culprit vessel(s) is revascularized and rhythm is restored.
Chances for survival are highest in younger patients, those that do not have chronic illnesses, and those who received immediate CPR after arrest.
Summary:
Consider emergent consultation for salvage PCI and ECMO in select cases of shock-refractory ventricular fibrillation associated with STEMI
Want more emergency cardiology pearls? Follow me @alifarzadmd
A recently published case report (attached) presents a fascinating case where salvage PCI and ECMO were used for shock-refractory VF. The patient survives with good neurological outcome. It highlights the multidisciplinary cooperation and resources necessary to utilize these heroic practices.
Brown DFM, Jaffer FA, Baker JN, Gurol ME. Case records of the Massachusetts General Hospital. Case 28-2013. A 52-year-old man with cardiac arrest after an acute myocardial infarction. N Engl J Med. 2013;369(11):1047–1054. doi:10.1056/NEJMcpc1304164.
Category: Orthopedics
Keywords: Stress fractures, runners (PubMed Search)
Posted: 9/28/2013 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Prior fracture represents the strongest predictor of stress fracture in both sexes
For girls: Low body mass index, (<19), late menarche (age 15 or older), previous participation in gymnastics and dance.
For boys: increased number of seasons.
Participation in basketball appears protective in boys.
This may represent a modifiable risk factor for stress fractures.
Tenforde AS, Sayres, LC, et al. Identifying sex-specific risk factors for stress fractures in Adolescent Runners. 2013
Category: International EM
Keywords: Trauma, Global, MVA (PubMed Search)
Posted: 9/25/2013 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Relevance to the EM Physician:
Although road traffic injury deaths have decreased in some high-income countries, by 2030 it is predicted that they will be the fifth leading cause of death worldwide, and the seventh leading cause of Disability Adjusted Life Years (DALY) lost.
Bottom Line:
Developing trauma and acute care capacities in low and middle-income countries is of utmost importance to mitigate the global burden of injuries.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
World Health Organization, Global status report on road safety, 2013
World Health Organization, Injuries Violence The Facts, 2010
Category: Critical Care
Keywords: Procalcitonin, Upper respiratory infections, antibiotics (PubMed Search)
Posted: 9/24/2013 by Feras Khan, MD
(Updated: 2/27/2026)
Click here to contact Feras Khan, MD
Background:
Clinical Question:
Meta-analysis:
Conclusions:
Limitations:
Bottom Line:
Clinical Outcomes Associated With Procalcitonin Algorithms to Guide Antibiotic Therapy in Respiratory Tract Infections
Philipp Schuetz, MD, MPH; Matthias Briel, MD, MSc; Beat Mueller, MD
JAMA. 2013;309(7):717-718. doi:10.1001/jama.2013.697.
http://jama.jamanetwork.com/article.aspx?articleid=1653510
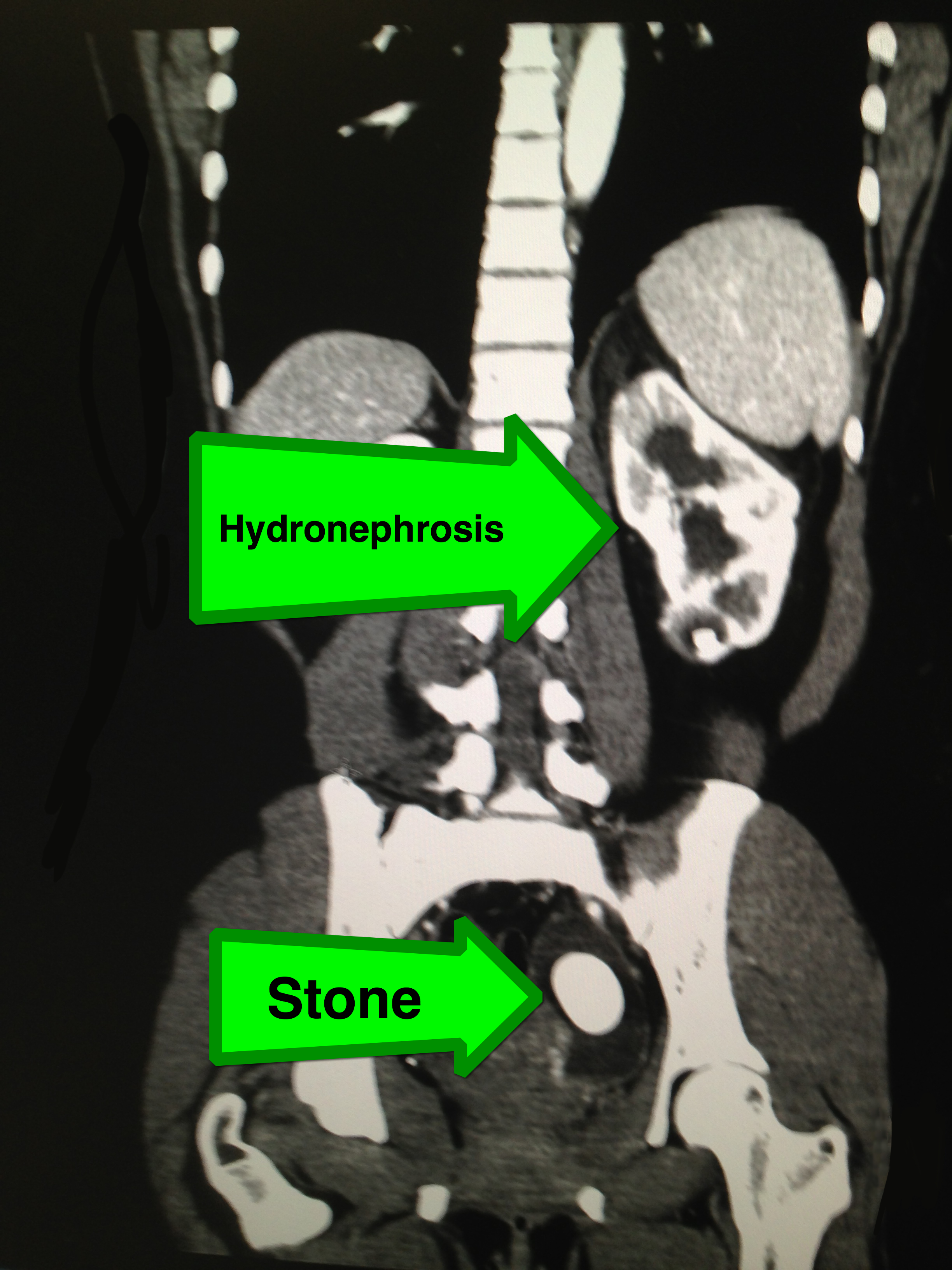
Category: Visual Diagnosis
Posted: 9/23/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
27 year-old female with no past medical history presents with sudden onset of left lower quadrant pain. What's the diagnosis?
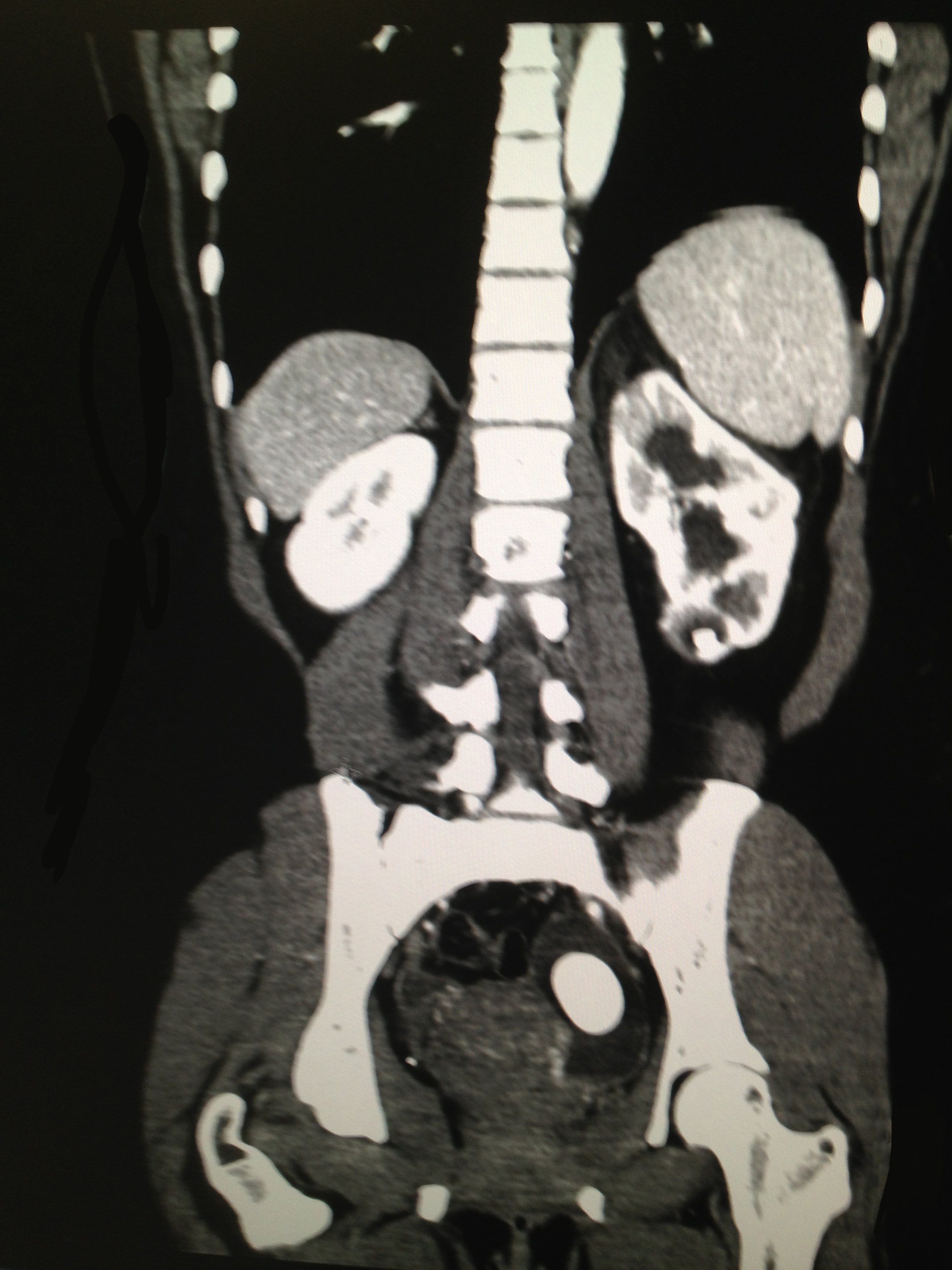
Large left-sided ureterolithiasis with hydronephrosis
Category: Cardiology
Keywords: Bundle branch block (PubMed Search)
Posted: 9/22/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Is RBBB More Indicative of Large Anteroseptal MI?
Strauss DG, Loring Z, Selvester RH, et al. Right, But Not Left, Bundle Branch Block Is Associated With Large Anteroseptal Scar. JACC. Sept 2013; 62(11): 959-967.
Category: Obstetrics & Gynecology
Keywords: Morning Sickness, Pregnancy (PubMed Search)
Posted: 9/21/2013 by Michael Bond, MD
Click here to contact Michael Bond, MD
Treatment:
Consider these therapies the next time you see a pregnant with persistent nausea and vomiting in her 1st
--Yemi
Niebyl, Jennifer MD. Nausea and Vomiting in Pregnancy. The New England Journal of Medicine. Oct 2010. 363:16.
Category: Pediatrics
Keywords: orthopedics, compartment syndrome (PubMed Search)
Posted: 9/20/2013 by Jenny Guyther, MD
(Updated: 2/27/2026)
Click here to contact Jenny Guyther, MD
We have learned how to diagnose compartment syndrome in adults, but how do you determine the early warning signs in a nonverbal or even frightened child?
Rising compartment pressures are related to increasing anxiety and agitation in children. A Boston study in 2001 showed that increasing pain medication requirements were detected 7 hours earlier than a vascular exam change. 90% of the patients with compartment syndrome in this study reported pain, but only 70% had another ‘P” (pallor, parasthesia, paralysis or pulselessness).
This has led to the proposal of the 3 “A”s for early identification of compartment syndrome in children: increasing anxiety, agitation and analgesia requirement.
Noonan and McCarthy. Compartment Syndrome in Pediatric Patients. Journal of Pediatric Orthopedics. Vol 30. No 2. March 2010.
Category: International EM
Posted: 9/18/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
General Information:
· The coming of the Affordable Care Act (ACA) is designed to shift patient care from episodic encounters to continuous community based partnerships.
· Elsewhere in the world, community health workers (CHWs) have been used effectively to improve health outcomes, reduce heath care costs and create jobs in infectious disease (TB, HIV), maternal child health and chronic disease management.
· CHWs are paid, full time lay provider members of community health systems.
o Sub-Saharan Africa is training, deploying and integrating one million CHWs into the health system via a targeted campaign.
o Brazil’s CHWs are part of family health teams that care for 110 million people.
o India employs 600,000 CHWs paid through a fee-for-service system for primary care functions.
· CHWs cost less, reduce readmissions and help address root causes of preventable chronic disease while remaining embedded in the community helping to strengthen long-term community relationships.
Relevance to the EM Physician:
As frustration with non-compliant patients mounts and the impact of the ACA looms, CHWs integrated into American communities may be just the answer we haven’t yet considered to help reduce ED overcrowding and improve our patients’ outcomes.
University of Maryland Section of Global Emergency Health
Author: Emilie J.B. Calvello, MD, MPH
Singh,P. Chokshi, D. Community Health Workers – A Local Solution to a Global Problem. NEJM. 2013, 369: 894 – 896.
Category: Critical Care
Posted: 9/17/2013 by Mike Winters, MBA, MD
(Updated: 2/27/2026)
Click here to contact Mike Winters, MBA, MD
Peri-Intubation Cardiac Arrest
Heffner AC, Swords DS, Neale MN, Jones AE. Incidence and factors associated with cardiac arrest complicating emergency airway management. Resuscitation 2013. [Epub ahead of print].
Category: Visual Diagnosis
Posted: 9/16/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
8 year-old girl presents with dysphagia and drooling, Xray is shown. What’s the diagnosis (and where is it located)?
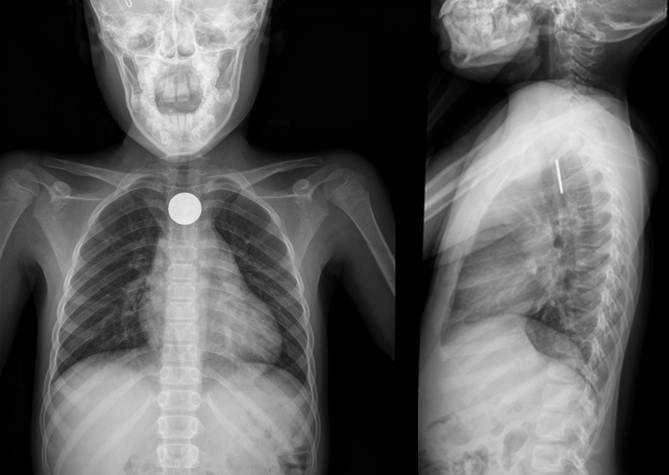
A coin located in the esophagus at the level of the cricopharyneus muscle
Foreign body (FB) pearls
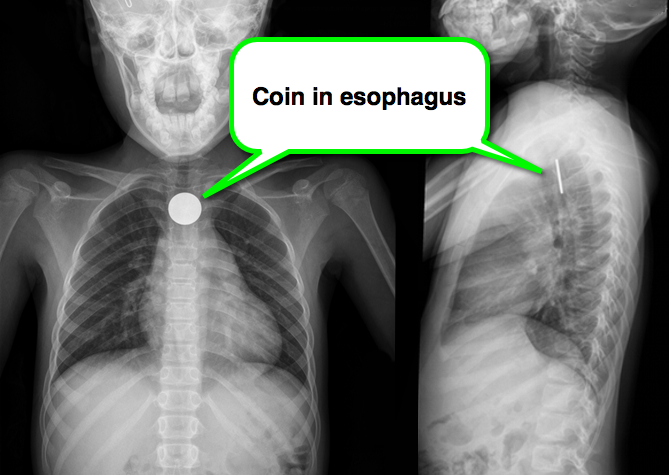
Kenton, Foreign Bodies in the Gastrointestinal Tract and Anorectal Emergencies, Emerg Med Clin N Am 29 (2011) 369–400
Category: Cardiology
Keywords: Acute Pericarditis, Colchicine (PubMed Search)
Posted: 9/15/2013 by Ali Farzad, MD
(Updated: 3/10/2014)
Click here to contact Ali Farzad, MD
Colchicine is known to be effective in treatment of recurrent pericarditis, but until recently its efficacy during the first attack of acute pericarditis has been uncertain.
A recent multicenter, double-blinded, RCT of patients with acute pericarditis found colchicine to be effective in reducing the rate of incessant or recurrent pericarditis (primary outcome), as well as the rate of hospitalization. Here are some highlights:
Bottom-line:
Colchicine is a safe and effective drug for the treatment of acute pericarditis. Consider adding colchicine to conventional therapies to reduce duration of symptoms, recurrences, and rate of hospitalization.
Imazio M, Brucato A, Cemin R, et al. A Randomized Trial of Colchicine for Acute Pericarditis. N Engl J Med. 2013 (.pdf attached)
Do you know the ECG findings of pericarditis and how to differentiate from other causes of diffuse ST-segment elevation? Check out these previous ECG videos to refresh your memory...
STEMI vs. Benign early repolarization vs. Pericarditis
