Category: Critical Care
Posted: 6/11/2013 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Rhabdomyolysis in the Critically Ill
Shapiro ML, Baldea A, Luchette FA. Rhabdomyolysis in the Intensive Care Unit. J Intensive Care Med 2012; 27:335-342.
Category: Visual Diagnosis
Posted: 6/10/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
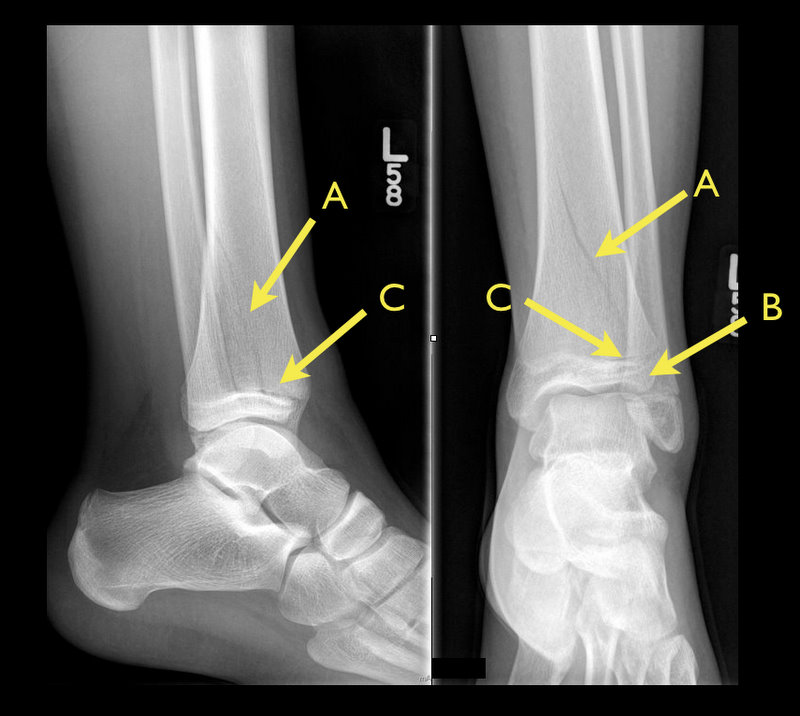
13 year-old female with ankle pain following fall down escalator. What's the diagnosis?

Answer: Tri-plane ankle fracture
Tri-plane Fractures

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 6/9/2013 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
Khoo C, Chakrabarti S, et al. Recognizing Life-Threatening Causes of Syncope. Cardiology Clinics. Volume 31, Feb, 2013
Category: Orthopedics
Keywords: Concussion, Adolscents (PubMed Search)
Posted: 6/8/2013 by Brian Corwell, MD
(Updated: 6/9/2013)
Click here to contact Brian Corwell, MD
The adolescent brain has not yet reached full maturation and is in a period of rapid development from ages 14 - 16.
Adolescents have been found to be more sensitive to the effects of concussion than adults
Concussed adolescents have deficits in attention and executive function lasting up to 2 months post injury.
Be aware that the adolescent brain will require extended recuperation time following injury
In the future, discharge instructions might need to say more than "don't get hit in the head till your headache goes away." Because of deficits in attention and executive function, physicians should consider recommendations about adolescents and jobs, school work and driving an automobile.
Effects of concussion on attention and executive function in adolescents. Howell D, Osternig L, et al. Medicine & Sceince in Sports and Exercise. June 2013
Category: Pediatrics
Posted: 6/7/2013 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Infant lumbar puncture is often difficut and may require repeated attempts. The traditional body positioning is lateral decubitus. Previous studies have examined the saftey of having the patient in a sitting position, and neonatal studies have suggested that the subarachnoid space increases in size as the patient is moved to the seated position. A study by Lo et al published last month looked to see if the same held true in infants.
50 healthy infants less then 4 months old had the subarachnoid space measured by ultrasound between L3-L4 in 3 positions: lateral decubitus, 45 degree tilt and sitting upright.
This study found that the size of the subarachnoid space did not differ significantly between the 3 positions. Authors postulated that a reason for increase sitting LP success rate that had been reported in anestesia literature with tilt position could be due to other factors such as increased CSF pressure, intraspinous space widening or improved landmark identification.
Sitting or Tilt Position for Infant Lumbar Puncture Does Not Increase Ultrasound Measurements of Lumbar Subarachnoid Space Width. Pediatr Emer Care 2013;29: 588-591.
Category: Toxicology
Keywords: Opioid, methadone, pain management, tolerance, analgesia (PubMed Search)
Posted: 6/6/2013 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Gussow, L. Toxicology Rounds. When Opioids Increase Pain. Emergency Medicine News Feb 2013. 35(2):6.
Category: International EM
Keywords: global, health, accountability, sovereignty (PubMed Search)
Posted: 6/5/2013 by Andrea Tenner, MD
(Updated: 2/8/2026)
Click here to contact Andrea Tenner, MD
General Information:
-The global health world is faced with an unprecedented challenge of a trio of threats:
1. Infections, undernutrition, reproductive health issues
2. Rising global burden of non-communicable diseases and risk factors
3. Challenges arising from globalization (climate change and trade politics)
-Definitions of global health are variable and can emphasize anything from types of health problems, populations of interest, geographic area or a specific mission. This makes governance and analysis difficult.
-During the past decade there has been an explosion of more than 175 initiatives, funds, agencies, and donors. Health is increasingly influenced by decisions made in other global policymaking areas.
-The major governance challenges for global health are:
1. Defining national sovereignty in the context of deepening health interdependence
2. Maximizing cross-sector interdependence
3. Developing clear mechanisms of accountability for non-state actors
Relevance to the US physician:
The Global Health System and its governance affects our ability to work effectively within the US and how we structure efforts to expand the reach of timely, effective emergency care worldwide.
Bottom Line:
The Global Health System has become more complex. Any development of Emergency Care Systems must take into account the complexity of actors in the field of global health.
The University of Maryland Section of Global Emergency Health
Author: Emilie J. B. Calvello, MD, MPH
An interactive graphic can be found at: http://www.nejm.org/doi/full/10.1056/NEJMra1109339?query=featured_home
Frenk, J. and Moon, S. Governance Challenges in Global Health. NEJM 2013; 368: 936 – 42.
Category: Critical Care
Posted: 6/4/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Therapeutic hypothermia (TH) following out-of-hospital cardiac arrest (OHCA) has increasingly been utilized since it was first described. TH following in-hospital cardiac arrest (IHCA), on the other hand, is not as commonplace or consistent despite a recommendation by the American Heart Association (AHA).
A recent prospective multi-center cohort-study demonstrated that of 67,498 patients with return of spontaneous circulation (ROSC) following IHCA only 2.0% of patients had TH initiated; of those 44.3% did not even achieve the target temperature (32-34 Celsius).
The factors found to be most associated with instituting TH were:
Bottom-line: Hospitals should consider instituting and adhering to local TH protocols for in-house cardiac arrests.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 6/3/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Ever wonder how to place a pigtail catheter?
Check out this video to learn how, click here
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 6/2/2013 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Category: Pharmacology & Therapeutics
Keywords: cellulitis, cephalexin, sulfamethoxazole/trimethoprim, Bactrim, streptococcus (PubMed Search)
Posted: 5/20/2013 by Bryan Hayes, PharmD
(Updated: 5/31/2013)
Click here to contact Bryan Hayes, PharmD
Background
In the current era of community-acquired MRSA (CA-MRSA), most of our outpatient treatment options for cellulitis aim to cover MRSA. Choices include sulfamethoxazole/trimethoprim (SMZ-TMP), doxycycline, linezolid, and clindamycin (depending on local susceptibility patterns).
A New Study
Take Home Clinical Points
Pallin DJ, et al. Clinical Trial: Comparative Effectiveness of Cephalexin Plus Trimethoprim-Sulfamethoxazole Versus Cephalexin Alone for Treatment of Uncomplicated Cellulitis: A Randomized Controlled Trial. Clinical Infectious Diseases 2013;56(12):1754-62. [PMID 23457080]
Follow me on Twitter (@PharmERToxGuy)
Category: Toxicology
Keywords: quetiapine, olanzapine, risperidone (PubMed Search)
Posted: 5/30/2013 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Hyperglycemia in the setting of antipsychotic use has been reported mostly with olanzapine (Zyprexa) but does occur with other antipsychotics. A recent study from the NYC medical examiner's office details 17 deaths of DKA due to antipsychotics and found that (from highest to lowest incidence) quetiapine > olanzapine > risperidone were the atypical antipsychotics found with these deaths.
Remember hyperglycemia occurs with patients on antipsychotics and can lead to hyperglycemia hyperosmolar coma or DKA. Both can be lethal.
Fatal Diabetic Ketoacidosis and Antipsychotic Medication.
Ely SF, Neitzel AR, Gill JR.
J Forensic Sci. 2012 Dec 27. doi: 10.1111/1556-4029.12044.
Category: International EM
Posted: 5/30/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Background Information:
Each year, an estimated 50 million travelers from Western countries visit tropical regions all over the world.
Given the potentially serious consequences for the patients and, their close contacts and healthcare workers it is important that life threatening tropical diseases are swiftly diagnosed.
Pertinent Study Design and Conclusions:
- Descriptive analysis of acute and potentially life threatening tropical diseases among 82,825 ill western travelers reported to GeoSentinel from June of 1996 to August of 2011.
- Of these travelers, 3,655 (4.4%) patients had an acute and potentially life threatening disease.
- The four most common conditions being falciparum malaria (76.9%), typhoid fever (11.7%), paratyphoid fever (6.4%), and leptospirosis (2.4%).
Bottom Line:
Western physicians seeing febrile and recently returned travelers from the tropics need to consider a wide profile of potentially life threatening tropical illnesses, with a specific focus on the most likely diseases described in this case series.
University of Maryland Section of Global Emergency Health
Author: Walid Hammad, MB ChB
Jensenius M, Han PV, Schlagenhauf P, Schwartz E, Parola P, Castelli F, von Sonnenburg F, Loutan L, Leder K, Freedman DO; GeoSentinel Surveillance Network. Acute and potentially life-threatening tropical diseases in western travelers—a GeoSentinel multicenter study, 1996-2011. Am J Trop Med Hyg. 2013 Feb; 88(2):397-404
Category: Critical Care
Posted: 5/28/2013 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
End-expiratory Occlusion Test
Monnet X, Teboul JL. Assessment of volume responsiveness during mechanical ventilation: recent advances. Critical Care 2013; 17:217.
Category: Visual Diagnosis
Posted: 5/27/2013 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
9 month-old presents with wheezing and the CXR is shown below. What's the diagnosis?
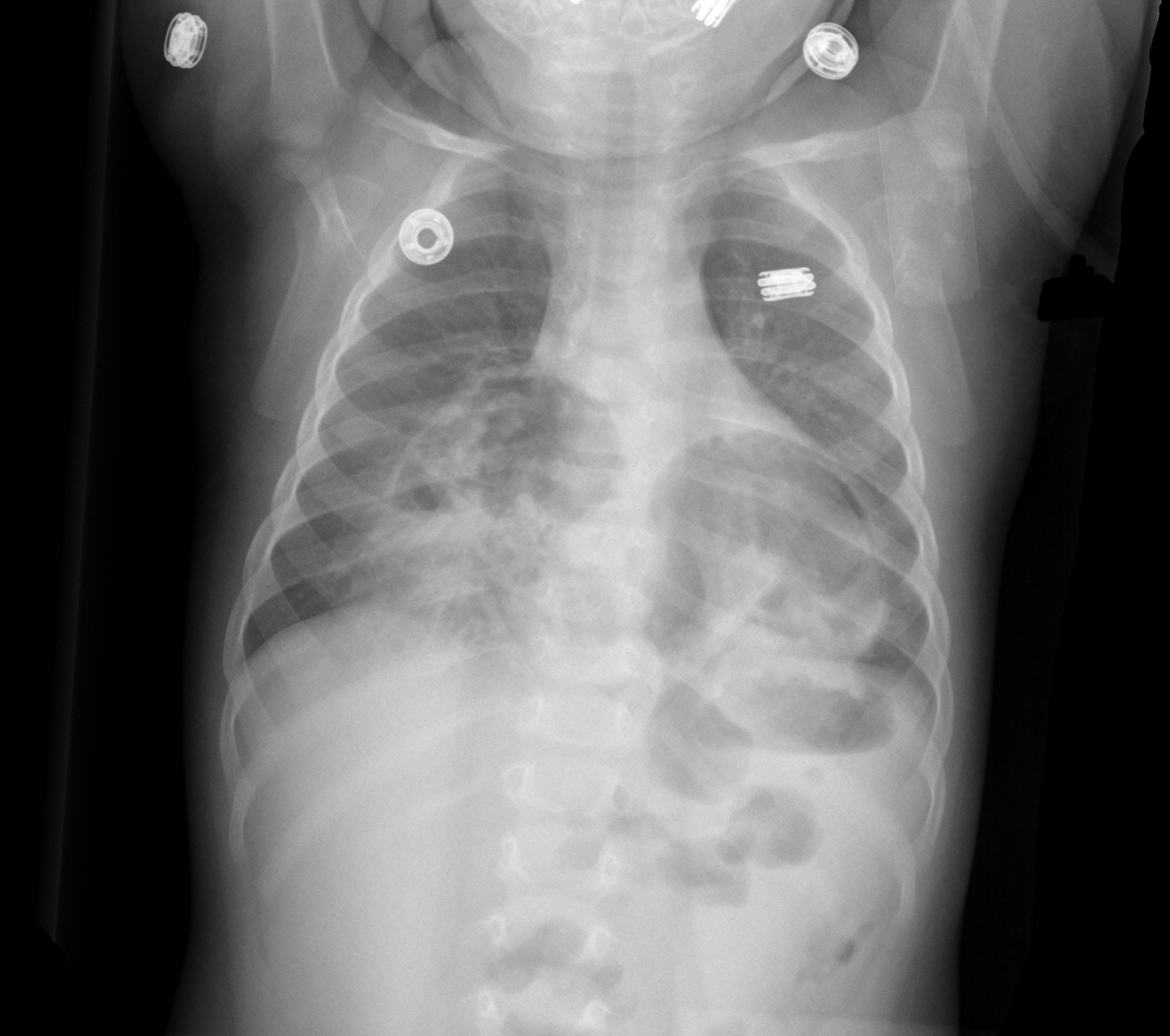
Congenital anterior diaphragmatic defects with herniated bowel.
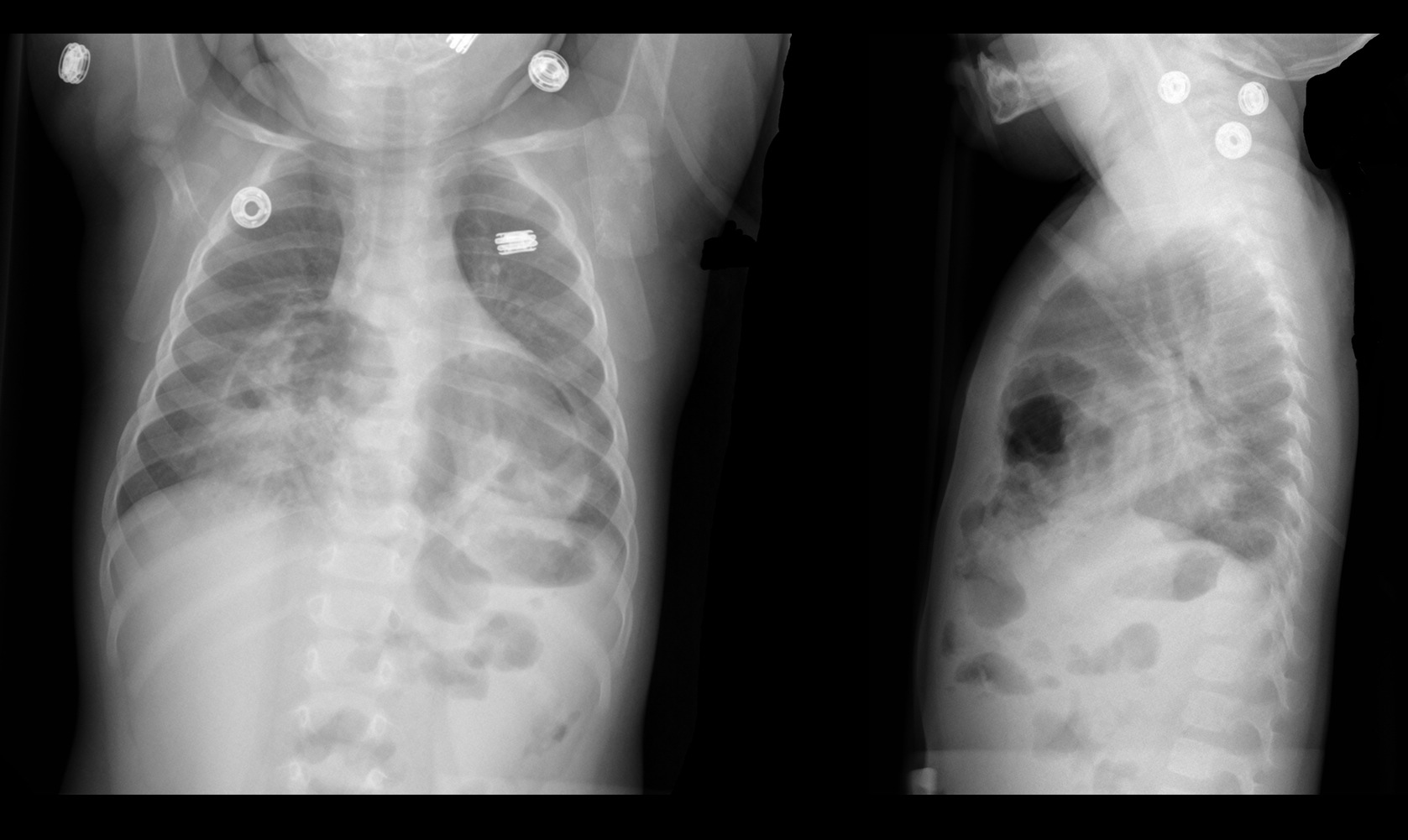
Follow me on Twiter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 5/26/2013 by Semhar Tewelde, MD
(Updated: 2/8/2026)
Click here to contact Semhar Tewelde, MD
Reynolds H. Myocardial infarction without obstructive coronary artery disease. Curr Opin Cardiol 2012, 27:655–660
Category: Orthopedics
Keywords: Frozen shoulder, adhesive capsulitis (PubMed Search)
Posted: 5/25/2013 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Adhesive capsulitis aka frozen shoulder
idiopathic loss of BOTH active and passive motion (this is a significant reduction of at least 50%)
Motion is stiff and painful especially at the extremes
Occurs due to thickening and contracture of the shoulder capsule
Affects patients between the ages of 40 and 60
Diabetes is the most common risk factor
Imaging is normal and only helpful to rule out other entities such as osteophytes, loose bodies etc.
Treatment includes NSAIDs, moist heat and physical therapy.
Patients should expect a recovery period of 1-2 years!
Category: Pediatrics
Posted: 4/26/2013 by Mimi Lu, MD
(Updated: 5/24/2013)
Click here to contact Mimi Lu, MD
Ultrasound findings of appendicitis
Ultrasound images:
http://www.youtube.com/watch?v=d9jKM6x52nk
http://sonocloud.org/watch_video.php?v=MWHM3D7KD25H
http://sonocloud.org/watch_video.php?v=54862AYWGHGA
Category: Toxicology
Keywords: intralipid, arrest, lipid (PubMed Search)
Posted: 5/23/2013 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
Utilizing 20% lipid emulsion at a dose of 1.5 mL/kg (100 mL Bolus) IV with repeat in 15 minutes in no response is being recommended in patients hemodynamic instabiity due to poisoning.
Probably more effective in lipophilic drugs is a current theory for the mechanism of action - the "lipid sink". The idea is that the lipids envelope the drug pulling it off its receptors or sequestering it in the intravascular space. A recent paper has added another mechanism - direct inotropic and lusiptropic effects.(1)
Also, if you think the therapy is experimental, think again. Another recent paper surveyed Poison Control Centers and found 30/45 Poison Centers in the US have a defined protocol for utilization of lipid emulsion therapy. The PCCs are recommending it more.(2)
What was once considered just a purely experimental therapy only used at the very end of code is becoming more mainstream. Comfort with its safety profile and anectodotal effiicacy continues to mount.
1. Fettiplace MR, Ripper R, Lis K, Lin B, Lang J, Zider B, Wang J,
Rubinstein I, Weinberg G. Rapid Cardiotonic Effects of Lipid Emulsion
Infusion. Crit Care Med. 2013 Mar 25. [Epub ahead of print]
2. Christian MR, Pallasch EM, Wahl M, Mycyk MB. Lipid Rescue 911: Are
Poison Centers Recommending Intravenous Fat Emulsion Therapy for
Severe Poisoning? J Med Toxicol. 2013 May 10. [Epub ahead of print]
Category: International EM
Posted: 5/22/2013 by Walid Hammad, MD, MBChB
Click here to contact Walid Hammad, MD, MBChB
Clinical Presentation:
- A 40-year-old Hispanic man was admitted to the hospital after being found unconscious. He had a 2-day history of disorientation that manifested itself as his being unable to recognize family members.
- Upon admission he regained consciousness, becoming alert and oriented, but developed urinary retention and was unable to move or feel his lower extremities.
- Spinal MRI (with and without gadolinium) showed the spinal cord to be abnormally diffuse, with swelling and edema in the cervicothoracic region.
Diagnosis:
- After an extensive work up for lymphoma and CNS infection, he was discovered to have toxoplasmosis and was found to be HIV positive, which was previously undiagnosed.
Discussion:
- Approximately 10% of patients with AIDS present with some neurological deficit as their initial complaint, and up to 80% will have CNS involvement during the course of their disease.
- Myelitis is a known complication of AIDS and is occasionally the initial complaint.
The incidence of myelopathy may be as high as 20%, with 50% of the cases reported post-mortem
- Toxoplasmosis is the most common cause of cerebral mass lesions in patients with AIDS
Occurring in 3–10% of patients in the United States and in up to 50% of AIDS patients in Europe, Latin America, and Africa
Bottom Line:
New neurological deficit in any patient should raise suspicion of HIV infection
Most patients with AIDS that present with evolving myelopathy, characterized by extremity weakness, sensory involvement, spinal cord enlargement, enhancing lesions in brain or spinal cord CT or MRI, have toxoplasmic myelitis
University of Maryland Section of Global Emergency Health
Author: Terrence Mulligan DO, MPH
"Spinal cord toxoplasmosis as an unusual presentation of AIDS: case report and review of the literature", Int J Emerg Med (2010) 3:439–442
