Category: Orthopedics
Keywords: hip fracture, transfusion, analgesia (PubMed Search)
Posted: 6/22/2024 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Hip Fractures
Femoral neck and intertrochanteric fractures occur most commonly among patients aged 65 and over
Major risk factors for hip fractures include osteoporosis and falls.
Patients with a low body mass index (BMI <22) appear to be at higher risk
Isolated trochanteric fractures occur more often in young active adults
In-hospital mortality rates are approximately 5% (range 1-10%)
In addition to making the diagnosis and consulting orthopedic surgery, ED providers must remember to provide adequate analgesia as elderly patients are often under medicated.
-Up to 72% receive no prehospital analgesia.
Extracapsular fractures cause more pain than intracapsular fractures due to the greater degree of periosteal trauma.
Poor pain control predisposes hip fracture patients to delirium
Retrospective studies indicate that patients at higher risk for significant bleeding have at least 2 of the following risk factors:
Age over 75 years, initial Hgb below 12 g/dL and peri trochanteric fracture location.
Category: Pediatrics
Keywords: fever, temperature, infection (PubMed Search)
Posted: 6/21/2024 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Teaching has circulated that a temperature of 40 degrees Celsius or above (hyperpyrexia), was associated with a greater incidence of serious bacterial infection. However, this teaching originated in a time prior to the availability of childhood vaccinations. In fact, the largest retrospective study to support this used data from 1966-1974.
2565 WELL APPEARING patients between the ages of 61 days and their 18th birthday who presented to a single tertiary care pediatric emergency department with the chief complaint of fever were included. The prevalence of serious bacterial infection was compared to the presence of hyperpyrexia, age, chronic conditions, gender and vaccination status.
Serious bacterial infections (SBIs) included: deep space infections, appendicitis, pneumonia, mastoiditis, lymphadenitis, acute bacterial rhinosinusitis, urinary tract infection, pyelonephritis, cholecystitis, tubo-ovarian abscess, septic arthritis, osteomyelitis, bacteremia or bacterial meningitis.
There was NO statistically significant association between hyperpyrexia and SBIs. Older age and make sex were associated with a higher risk of SBIs.
Bottom line: In well appearing children 61 days and older, having a temperature >/= to 40 degrees was not associated with serious bacterial infections.
Rachad S, Nickel D, Berry F, et al. Risk of serious bacterial infections in pediatric patients with hyperpyrexia. J Am Coll Emerg Physicians Open. 2024;5(2):e13135. Published 2024 Mar 13. doi:10.1002/emp2.13135
Category: Trauma
Keywords: troponin fall geriatric trauma (PubMed Search)
Posted: 6/20/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
A prospective European study of patients over age 65 presenting with a ground level fall obtained troponin levels to ascertain if myocardial infarction was a cause of the ground level fall. Troponin levels were elevated in a majority of patients however only 0.5% were defined as having a myocardial infarction. Of the 3% who died within 1 year, troponin was found to be higher than those that survived the one-year study period. The authors concluded “Our data do not support the opinion that falls may be a common presenting feature of MI. We discourage routine troponin testing in this population. However, hs-cTnT and hs-cTnI were both found to have prognostic properties for mortality prediction up to 1?year.”
Diagnostic and prognostic value of cardiac troponins in emergency department patients presenting after a fall: A prospective, multicenter study
Tanguy Espejo, Lukas Terhalle, Alexandra Malinovska MD, Henk B. Riedel MD, Laura Arntz MD, Livia Hafner, Karen Delport-Lehnen MD, Joanna Zuppinger MD,
First published: 26 March 2024
Academic Emergency Medicine
Category: EMS
Keywords: intubation, timing, trauma arrest, prehospital (PubMed Search)
Posted: 6/19/2024 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Several studies have shown that patients who require a resuscitative thoracotomy (RT) have a higher odds of survival if they are transported by police or in private vehicles. This study examined 195 patients who required RT to see if prehospital intubation and out of hospital time (OOHT) affected ROSC rates.
There was no association between OOHT and ROSC and no association of OOHT and survival. The mean OOHT for this study was only 25 minutes which is faster than other studies.
The odds of ROSC were lower in patients who had ANY intubation attempts prior to arrival.
Bottom line: BLS airway management (or supraglottic placement) may be more beneficial for the trauma arrest patient in the prehospital setting.
Radulovic N, Hillier M, Nisenbaum R, Turner L, Nolan B. The impact of out-of-hospital time and prehospital intubation on return of spontaneous circulation following resuscitative thoracotomy in traumatic cardiac arrest. Prehosp Emerg Care. 2023 Nov 28:1-14. doi: 10.1080/10903127.2023.2285390. Epub ahead of print. PMID: 38015060.
Category: Critical Care
Keywords: RSI, intubation, magnesium (PubMed Search)
Posted: 6/18/2024 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Magnesium is known to relax smooth muscles. Interestingly, there is also some literature using it as part of Rapid Sequence Intubation (RSI) pre-treatment in general, in hopes that this or other mechanisms might allow it to improve intubating conditions. Zouche et al recently published an RCT looking at giving IV magnesium as part of RSI pretreatment in cases where neuromuscular blockade (NMB) is not going to be given (e.g. scenarios where it is contraindicated). IV Magnesium Sulfate, 50 mg/kg in 100 mL of saline given 15 minutes before induction, significantly improved intubating conditions in those getting sedation but not NMB (95% vs 39%).
In 2013, Park et al did an RCT giving magnesium to all RSIs, even with the use of rocuronium in those patients, arguing that magnesium is also known to potentiate the effects of non-depolarizing NMB agents. They also found better intubating conditions in the magnesium patients.
In both trials, magnesium was associated with lower heart rates and less hypertension in the peri-intubation and immediate post-intubation periods (of note: high dose magnesium is known to be associated with lower blood pressures, and can induce overt hypotension). Neither study was really powered for more important measures like first pass success, mortality, or important side effects like peri-intubation hypotension.
Bottom Line: These are two small trials, and while more abundant literature should probably be obtained before we change our practice, one could consider giving magnesium sulfate, 50 mg/kg in 100 mL saline, prior to intubation in an attempt to improve intubating conditions. In my opinion, this is probably worth considering in the rare circumstance that your patient has a true contraindication to neuromuscular blockade, but I probably wouldn't start doing this in standard RSI where you're going to be giving NMB until more literature confirms the safety of this approach. Also, I would avoid this in situations where the patient is already hypotensive or at high risk of peri-intubation hypotension. This may be worth considering in the very rare patient you're not necessarily going to give NMB to right away (maybe awake fiberoptic intubations?) who are also very low risk for hypotension.
Imen Zouche, Wassim Guermazi, Faiza Grati, Mohamed Omrane, Salma Ketata, Hichem Cheikhrouhou, Intravenous magnesium sulfate improves orotracheal intubation conditions: A randomized clinical trial, Trends in Anaesthesia and Critical Care, Volume 57, 2024, 101371, ISSN 2210-8440, https://doi.org/10.1016/j.tacc.2024.101371 (https://www.sciencedirect.com/science/article/pii/S221084402400042X)
Park SJ, Cho YJ, Oh JH, Hwang JW, Do SH, Na HS. Pretreatment of magnesium sulphate improves intubating conditions of rapid sequence tracheal intubation using alfentanil, propofol, and rocuronium - a randomized trial. Korean J Anesthesiol. 2013 Sep;65(3):221-7. doi: 10.4097/kjae.2013.65.3.221. Epub 2013 Sep 25. PMID: 24101956; PMCID: PMC3790033.
Category: Critical Care
Keywords: ICU, delirium, antipsychotic (PubMed Search)
Posted: 6/18/2024 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
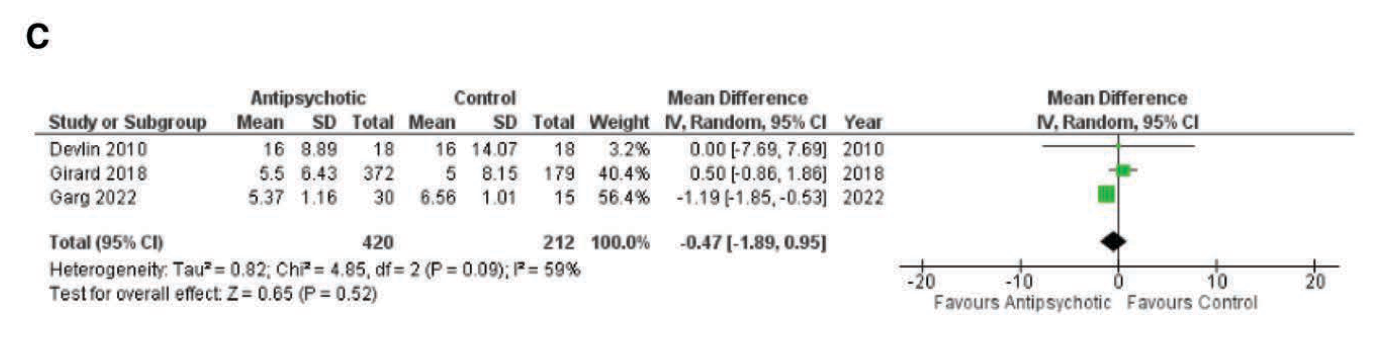
Title: Antipsychotics in the Treatment of Delirium in Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials.
We all do it. When our patients in the ICU develop delirium, we would give them an antipsychotic, commonly quetiapine (Brand name Seroquel), and all is good. However, results from this most recent meta-analysis may suggest otherwise.
Settings: This is a meta-analysis from 5 Randomized Control Trials. Intervention was antipsychotic vs. placebo or just standard of care.
Participants: The 5 trials included A total of 1750 participants. All trials used Confusion Assessment Method for the ICU or Intensive Care Delirium Screening Checklist to measure delirium.
Outcome measurement: Delirium – and Coma-Free days
Study Results:
The use of any antipsychotic (typical or atypical) did not result in a statistically significant difference in delirium- and coma-free days among patients with ICU delirium (Mean Difference of 0.9 day; 95% CI -0.32 to 2.12).
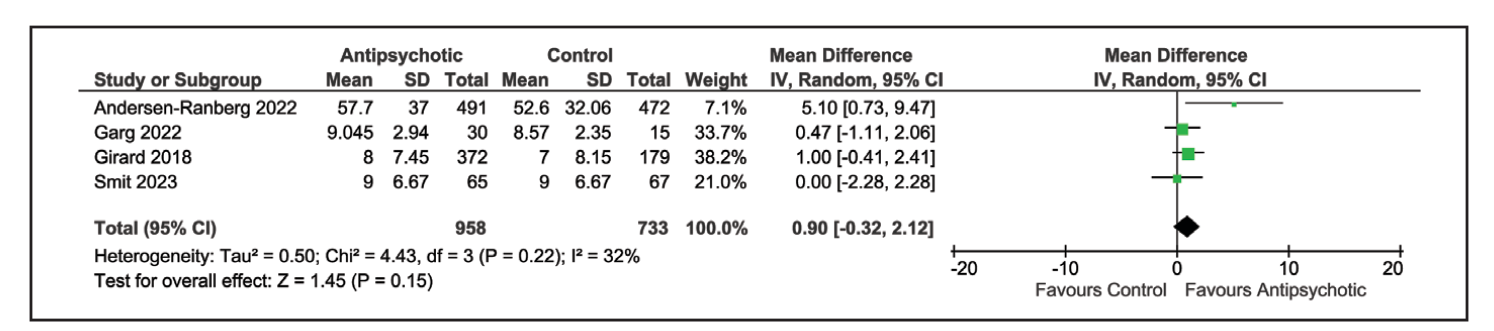
Similarly, atypical antipsychotic medication also did not result in difference of delirium- and coma-free days: Mean difference of 0.56 day; 95% CI -0.85 to 1.97).
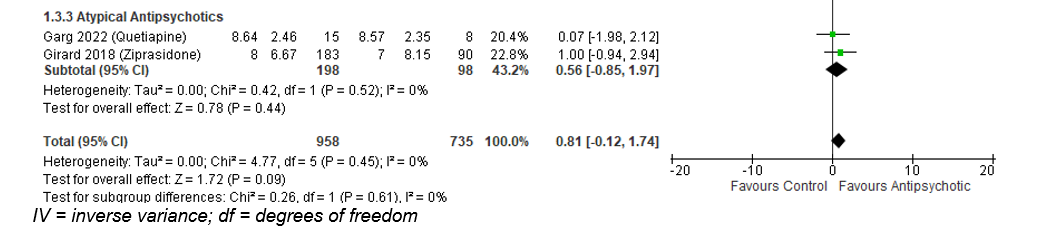
ICU length of stay was also not different in the group receiving antipsychotic: Mean difference -0.47 day, 95% CI -1.89 to 0.95).
Discussion:
The authors used both delirium -free and coma-free days as a composite outcome because they reasoned that delirium cannot be evaluated in unresponsive patients. This composite outcome might have affected the true incidence of delirium and the outcome of delirium-free days.
This meta-analysis would be different from previous ones that aimed to answer the same question. Previous studies compared either haloperidol vs a broader range of other medication (atypical antipsychotic, benzodiazepines) (Reference 2) or included all ICU patients with or without delirium who received haloperidol vs. placebo (Reference 3). Overall, those previous studies also reported that the use of haloperidol has not resulted in improvement of delirium-free days.
Conclusion:
There is evidence that the use of anti-psychotic medication does not result in difference of delirium- or coma-free days among critically ill patients with delirium.
1.Carayannopoulos KL, Alshamsi F, Chaudhuri D, Spatafora L, Piticaru J, Campbell K, Alhazzani W, Lewis K. Antipsychotics in the Treatment of Delirium in Critically Ill Patients: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. Crit Care Med. 2024 Jul 1;52(7):1087-1096. doi: 10.1097/CCM.0000000000006251. Epub 2024 Mar 15. PMID: 38488422.
2. Andersen-Ranberg NC, Barbateskovic M, Perner A, Oxenbøll Collet M, Musaeus Poulsen L, van der Jagt M, Smit L, Wetterslev J, Mathiesen O, Maagaard M. Haloperidol for the treatment of delirium in critically ill patients: an updated systematic review with meta-analysis and trial sequential analysis. Crit Care. 2023 Aug 26;27(1):329. doi: 10.1186/s13054-023-04621-4. PMID: 37633991; PMCID: PMC10463604.
3. Huang J, Zheng H, Zhu X, Zhang K, Ping X. The efficacy and safety of haloperidol for the treatment of delirium in critically ill patients: a systematic review and meta-analysis of randomized controlled trials. Front Med (Lausanne). 2023 Jul 27;10:1200314. doi: 10.3389/fmed.2023.1200314. PMID: 37575982; PMCID: PMC10414537.
Category: Ultrasound
Keywords: POCUS; FAST exam; Trauma (PubMed Search)
Posted: 6/17/2024 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Although the FAST exam can be helpful in expediting care of patients with intraabdominal injuries, there are a few pitfalls.
Pitfalls:
1. The FAST exam has a wide sensitivity which depends on sonographer skill and the patient's body habitus. It is best used as a “Rule In NOT Rule Out” exam.
2. The FAST exam is not good for identifying bowel injury or retroperitoneal bleeding and may not be able to pick up low volume hemoperitoneum.
3. The FAST exam is not able to identify the type of fluid e.g. ascites vs blood.
Some Tips for Performing the FAST exam:
1.Go slow, fan through the view completely. In the RUQ view make sure you are evaluating the liver tip.
2. Place the patient in slight Trendelenburg.
3. If you have clinical concern for injury, don't stop at a negative FAST.
Savatmongkorngul S, Wongwaisayawan S, Kaewlai R. Focused assessment with sonography for trauma: current perspectives. Open Access Emerg Med. 2017 Jul 26;9:57-62. doi: 10.2147/OAEM.S120145.
Category: Trauma
Keywords: hemorrhage, tourniquet, innovation, Delphi (PubMed Search)
Posted: 6/9/2024 by Robert Flint, MD
(Updated: 6/16/2024)
Click here to contact Robert Flint, MD
Appropriately, a great deal of time and energy is being expended to educate on the use of tourniquets to prevent mass hemorrhage. Are the current generation of tourniquets the best that we can have? These authors performed a Delphi study to assess needs with tourniquet design.
They concluded the next generation of tourniquets should have the following: “Capable of being used longer than 2 hours, applied and monitored by anyone, data displays, semiautomated capabilities with inherent overrides, automated monitoring with notifications and alerts, and provide recommended actions.”
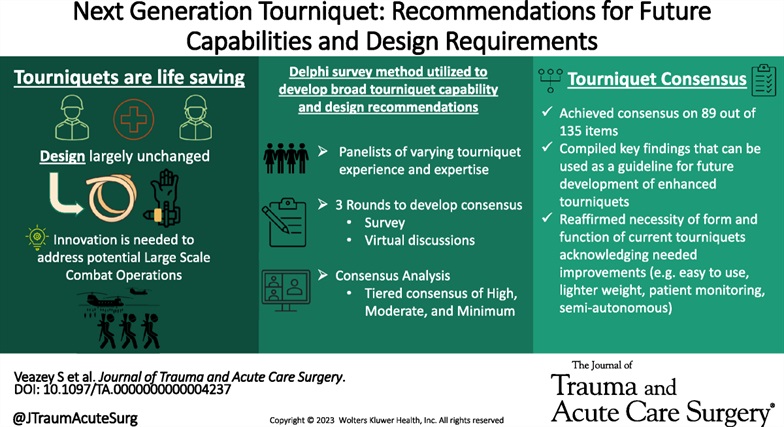
Veazey, Sena R. MS; Mike, Jared F. PhD; Hull, Darke R. BS; Ryan, Kathy L. PhD; Salinas, Jose PhD; Kragh, John F. Jr MD. Next-generation tourniquet: Recommendations for future capabilities and design requirements. Journal of Trauma and Acute Care Surgery 96(6):p 949-954, June 2024. | DOI: 10.1097/TA.0000000000004237
Category: Administration
Keywords: pulse oximetry, skin pigmentations (PubMed Search)
Posted: 6/15/2024 by Kevin Semelrath, MD
(Updated: 2/7/2026)
Click here to contact Kevin Semelrath, MD
This article shows us that even things we think of as objective measures in medicine may actually perpetuate systemic biases.
The study evaluated controlled hypoxemia in a group of volunteers. Traditional pulse ox devices measured falsely elevated pulse ox readings in participants with dark skin pigmentation and low tissue perfusion. It suggested different types of devices that may have improved accuracy in patients with darker skin pigmentation, but the underlying problem still exists.
Bottom line, this goes to prove what we have taught, never rely on a single value to reassure yourself of the patient's status, always take into account the bigger picture.
Low Perfusion and Missed Diagnosis of Hypoxemia by Pulse Oximetry in Darkly Pigmented Skin: A Prospective Study. Anesth Analg. 2024 Mar 1;138(3):552-561. doi: 10.1213/ANE.0000000000006755. Epub 2023 Dec 18. PMID: 38109495
Category: Pharmacology & Therapeutics
Keywords: Pharmacology, Toxicology, Acetaminophen, Acetylcysteine, NAC (PubMed Search)
Posted: 6/13/2024 by Matthew Poremba
Click here to contact Matthew Poremba
A panel comprised of 21 participants selected by four clinical toxicology societies (America’s Poison Centers, American Academy of Clinical Toxicology, American College of Medical Toxicology, and Canadian Association of Poison Control Centers) sought to develop consensus guidelines for management of acetaminophen poisoning in the US and Canada. Highlights from this framework include:
Acetylcysteine Stopping Criteria
A common misconception is that acetylcysteine is administered for 21 hours then discontinued. The consensus statement codifies the practice of reassessing the patient at the end of the acetylcysteine infusion and only stopping acetylcysteine if all of the following criteria are met:
Ingestion of Extended-Release Acetaminophen Products
Extended release acetaminophen products are available on the US market. Management is largely the same as for instant release acetaminophen except for several exceptions:
Management of Repeated Supratherapeutic Acetaminophen Ingestion
When a patient presents following repeated acetaminophen ingestions over a period of greater than 24 hours the Matthew-Romack nomogram is no longer applicable for guiding decisions regarding treatment with acetylcysteine. The consensus statement recommends initiating treatment in this scenario if the patient’s acetaminophen concentration is > 20 mcg/mL or if patient’s AST/ALT are abnormal.
Final Thoughts:
These guidelines will function as a useful reference and officially codify a general framework with evidence-based recommendations for the management of acetaminophen poisoning. As always, a poison center or clinical toxicologist should be consulted for any complicated or serious acetaminophen poisoning.
Dart, Richard C et al. “Management of Acetaminophen Poisoning in the US and Canada: A Consensus Statement.” JAMA network open vol. 6,8 e2327739. 1 Aug. 2023, doi:10.1001/jamanetworkopen.2023.27739
Category: Gastrointestional
Keywords: antibiotics appendicitis (PubMed Search)
Posted: 6/12/2024 by Neeraja Murali, DO, MPH
(Updated: 2/7/2026)
Click here to contact Neeraja Murali, DO, MPH
By now, most of us are aware that there's evidence supporting the use of an antibiotics-only approach for acute uncomplicated appendicitis. One of the major trials evaluating this is the Appendicitis Acuta II Trial. Our paper today continued longitudinal follow up of the original cohort enrolled in this study.
Patients were randomized to receive either oral antibiotic monotherapy (moxifloxacin 400 mg/d x 7 days) or IV and oral antibiotics (IV ertapenem 1 g/d x 2 days plus oral levofloxacin 500 mg/d + metronidazole500 mg q8h x 5 d).
Primary endpoint: resolution of acute appendicitis and hospital discharge without surgery and no reoccurence at time of follow up (3 years later).
There were 582 patients in the three year follow up cohort; Success was 63.4% (1-sided 95% CI, 58.8% to ?) in the oral antibiotics only group and 65.2% in the IV + oral antibiotics(1-sided 95% CI, 60.5% to ?). The difference in success rate was -1.8% (1-sided 95% CI, ?8.3 percentage points to ?; P?=?.14 for noninferiority).
No significant difference in secondary endpoints, including treatment-related adverse events, quality of life, length of hospital stay, and length of sick leave.
In this secondary analysis of the three year cohort from the APPAC II trial, there was a slightly higher appendectomy rate in patients who received oral antibiotic therapy; noninferiority of this regimen (as composed to combined) could not be demonstrated.
Selänne L, Haijanen J, Sippola S, et al. Three-Year Outcomes of Oral Antibiotics vs Intravenous and Oral Antibiotics for Uncomplicated Acute Appendicitis: A Secondary Analysis of the APPAC II Randomized Clinical Trial. JAMA Surg. Published online April 17, 2024. doi:10.1001/jamasurg.2023.5947
Category: Critical Care
Posted: 6/11/2024 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
Many patients present to the ED with hypercarbic respiratory failure (i.e. COPD exacerbation, obesity hypoventilation syndrome etc.). Typically, our first line of treatment is the use of BiPAP, where we set an inspiratory pressure (IPAP) and an expiratory pressure (EPAP). The difference between these two pressures (as well as patient effort) determines the tidal volumes (and consequently minute ventilation) a patient receives in our attempts to help the patient “blow off CO2.”
If you are having trouble with continued hypercarbia despite the use of BiPAP, another NIPPV mode that can be trialed is Average Volume-Assured Pressure Support (AVAPS). With BiPAP the patient receives the same fixed IPAP no matter what, even if their tidal volumes are lower than what is needed. With AVAPS, the ventilator will self-titrate the IPAP and increase (or decrease) the IPAP to reach the tidal volumes that you set, increasing the odds the patient will achieve the minute ventilation you are trying to achieve.
(AVAPS is essentially a non-invasive version of PRVC)
Initial settings (ask your RTs for help!):
Category: Pediatrics
Keywords: pediatrics, orthopedics, fracture (PubMed Search)
Posted: 6/6/2024 by Kathleen Stephanos, MD
(Updated: 6/10/2024)
Click here to contact Kathleen Stephanos, MD
The supracondylar fracture is one of the most common pediatric fractures. It typically occurs due to a FOOSH injury and is a result of fracture through an area of high growth (and therefore weaker bone structure) in the pediatric distal humerus. Appearance on x-ray depends on the degree of displacement, however in cases without obvious displacement, providers must look for more subtle signs on x-ray. For example, a “sail sign” of the anterior fat pad and appearance of a posterior fat pad indicate a joint effusion and are suggestive of a fracture. However, there are often still equivocal x-rays in children with notable tenderness on exam, and failure to appropriately immobilize these fractures can result in pain and higher risk of injury resulting in displacement.
In 2021, Varga et al, looked into the ability to assess for supracondylar fractures with ultrasound. This prospective study evaluated 5 locations in the pediatric elbow for signs of fracture. Ultimately, this was able to identify more fractures than x-ray alone, and was a useful tool for equivocal cases. This is not an isolated study, but one of the most comprehensive, looking into ultrasound as a tool for supracondylar fracture identification.
It may be time to grab that ultrasound probe to look for fractures in pediatric patients with pain but an unclear elbow x-ray.
Varga M, Papp S, Kassai T, Bodzay T, Gáti N, Pintér S. Standardized sonographic examination of pediatric elbow injuries is an effective screening method and improves diagnostic efficiency. Injury. 2021 Mar;52 Suppl 1:S25-S30. doi: 10.1016/j.injury.2020.02.056. Epub 2020 Feb 28. PMID: 32173077.
Category: Trauma
Keywords: BIG, transfer, head trauma, brain injury (PubMed Search)
Posted: 6/9/2024 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
This study used the modified Brain injury Guidelines retrospectively to assess whether the guidelines would have saved transfers to their level one facility safely. They concluded the guidelines would have effectively prevented unnecessary mBIG 1 and mBIG2 transfers with no patient harm.
TABLE 1 - Modified Brain Injury Guidelines Radiologic Stratification, as per Kahn et al.
| mBIG 1 | mBIG 2 | mBIG 3 | |
|---|---|---|---|
| Skull fracture | No | Non-displaced | Displaced |
| SDH | ?4 mm | 4–7.9 mm | ?8 mm |
| EDH | No | No | Yes |
| SAH | ?3 sulci and <1 mm | Single hemisphere or 1–3 mm | Bihemisphere or >3 mm |
| IVH | No | No | Yes |
| IPH | ?4 mm | 4–7.9 mm | ?8 mm or multiple |
EDH, epidural hematoma; IPH, intraparenchymal hemorrhage; IVH, intraventricular hemorrhage; SAH, subarachnoid hemorrhage.
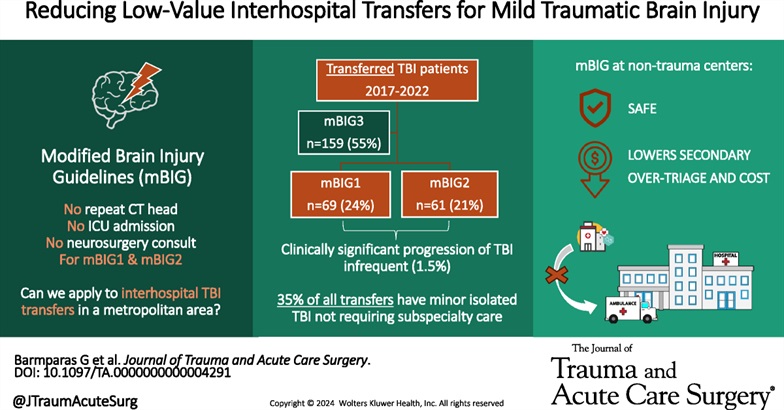
Shen, Aricia MD; Mizraki, Nathaniel MD; Maya, Marcel MD; Torbati, Sam MD; Lahiri, Shouri MD; Chu, Ray MD; Margulies, Daniel R. MD; Barmparas, Galinos MD. Reducing low-value interhospital transfers for mild traumatic brain injury. Journal of Trauma and Acute Care Surgery 96(6):p 944-948, June 2024. | DOI: 10.1097/TA.0000000000004291
Category: Orthopedics
Posted: 6/8/2024 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
A recent study attempted to investigate the relationship between a history of strength training with symptomatic and structural findings of knee osteoarthritis (OA).
For comparison, previous studies have shown that duration of football participation increases risk of radiographic knee OA.
Methods: Retrospective, cross-sectional multicenter study
2,607 participants without OA. Community population. 44% male. Mean age 64.3 years. Mean BMI 28.5.
Strength training (via self-administered questionnaire) defined as those exposed (n=1789 ) and not exposed (n=818). If exposed, groups were divided into low, medium and high.
Outcomes were 1) Radiographic OA. 2) Symptomatic radiographic OA. 3) Frequent knee pain
Results: Strength training at any point in life vs no strength training was associated with lower incidence of all outcome measures:
Odds ratio1) 0.82, 2) 0.83 and 3) 0.77.
Conclusions: Strength training is beneficial for future knee health
However, when separated by groups (low, medium and high), only the high-exposure group had significantly reduced odds of less frequent radiographic OA, symptomatic radiographic OA, and frequent knee pain.
Findings were similar for different age ranges
The association between strength training and less frequent radiographic OA, symptomatic radiographic OA, and frequent knee pain was strongest in the older age groups.
Lo GH, et al. Strength Training Is Associated With Less Knee Osteoarthritis: Data From the Osteoarthritis Initiative. Arthritis Rheumatol. 2024 Mar;76(3):377-383.
Category: Critical Care
Posted: 6/4/2024 by William Teeter, MD
Click here to contact William Teeter, MD
This really interesting study suggests that the classic site of CPR “in the middle of the chest” may actually not be the ideal place to perform CPR. Previous imaging studies demonstrate that the ventricles are primarily beneath the lower third of the sternum and that standard placement of CPR compressions may deform the aortic valve, blocking the LVOT, and theoretically limiting perfusion of the coronaries and brain.
This study compared a standard CPR group with those undergoing TEE-guided chest compressions to avoid aortic valve compression. Those in the non-AV compression group had significantly increased likelihood of ROSC, survival to ICU, and higher femoral arterial diastolic pressures. However, there was no difference in long-term outcomes or end-tidal CO2.
Summary: Avoiding AV compression during CPR significantly improved the chance at ROSC in adult OHCA, but this small observational study did not show any difference in long term outcomes when compared to standard practice. Lowering the point of chest compressions in CPR to the lower third of the sternum may be beneficial.
Category: Administration
Keywords: POCUS, musculoskeletal, fingers, water baths (PubMed Search)
Posted: 6/3/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
Do you have a patient with a finger injury or infection, or possibly a retained foreign body?
Try placing the hand in a water bath and use a linear ultrasound probe for evaluation. If there is an open wound, use a sterile ultrasound probe cover.
With ultrasound guidance, you can observe dynamic finger movements and identify areas that may require abscess drainage.
Category: Trauma
Posted: 5/29/2024 by Robert Flint, MD
(Updated: 6/1/2024)
Click here to contact Robert Flint, MD
In this Scandinavian study looking at 2,362 head injury patients on oral anticoagulants, the authors found only 5 cases of delayed hemorrhage and none of the five underwent neurosurgery. The authors concluded:
“In patients with head trauma, on oral anticoagulation, the incidence of clinically relevant delayed intracranial hemorrhage was found to be less than one in a thousand, with detection occurring four days or later after initial presentation.”
It would appear based on this study and others that it is safe to discharge these patients with a normal head CT and giving strict return precautions for headache, nausea, vomiting or other changes.
André, L., Björkelund, A., Ekelund, U. et al. The prevalence of clinically relevant delayed intracranial hemorrhage in head trauma patients treated with oral anticoagulants is very low: a retrospective cohort register study. Scand J Trauma Resusc Emerg Med 32, 42 (2024). https://doi.org/10.1186/s13049-024-01214-0
Category: Pediatrics
Posted: 5/31/2024 by Rachel Wiltjer, DO
(Updated: 2/7/2026)
Click here to contact Rachel Wiltjer, DO
Histamine is present in mosquito saliva contributing to itch with bites, however, certain populations – including children – can experience an exaggerated reaction. Skeeter syndrome is a large, localized inflammatory reaction secondary to a mosquito bite that presents with warmth, swelling, and itching. There can occasionally be associated lymphadenopathy and fever as well. The rapid onset is what best differentiates it from cellulitis. Treatment is primarily symptomatic in nature, focused on relieving itch, with antihistamines and topical therapy. There may also be a role for prophylactic antihistamine usage at times when mosquito bites will be unavoidable in a patient known to have developed Skeeter syndrome previously. Other patients who may be affected include those with immunologic and autoimmune phenomena, those with underlying atopy, outdoor workers with frequent exposure, and those with new exposure to indigenous mosquitos.
Take Home: Consider insect (mosquito bite) when evaluating for cellulitis/infection in pediatric patients, with impressive skin findings but otherwise unremarkable exams. They present with rapid onset and itching instead of pain. This can be especially prominent in periorbital and auricular presentations.
Vander Does A, Labib A, Yosipovitch G. Update on mosquito bite reaction: Itch and hypersensitivity, pathophysiology, prevention, and treatment. Front Immunol. 2022 Sep 21;13:1024559
Category: Misc
Keywords: sleep (PubMed Search)
Posted: 5/29/2024 by Visiting Speaker
(Updated: 2/7/2026)
Click here to contact Visiting Speaker
Title: Basics of Sleep Physiology and Architecture
By: Youssef Annous, MD
Sleep is integral for physical and mental health and performance. Sleep is extremely well conserved among species. All mammals need sleep to survive.1 A single sleep cycle typically lasts anywhere between 90 and 120 minutes and is broken down into two phases2:
Non-Rapid Eye Movement sleep
Stage 1 (Light Sleep)
This is the lightest form of sleep and the easiest to wake up from. During this stage, it is normal to experience muscle twitching and the sensation of drifting in and out of consciousness. This stage lasts approximately 5 minutes in the beginning of sleep and comprises around 5% of total sleep duration.2
Stage 2 (Light Sleep)
During this stage, you are likely to begin experiencing decrease in body temperature, heart rate (HR), blood pressure (BP) and respiratory rate (RR). Electroencephalography (EEG) during this phase of sleep would show sleep spindles and K complexes.2 These findings have been linked to memory consolidation.3
Stage 3 (Deep Sleep)
This is the deepest stage of sleep. During this phase, body temperature, HR, BP, and RR are at their lowest. This is the most restorative stage of sleep. It is essential for immune health, cardiovascular health, tissue repair, bone growth, and muscle recovery.2 It is also when growth hormone (GH) is at its highest. Physiological (e.g. illness) or psychological (e.g. anxiety) stressors can negatively impact this stage. We experience less deep sleep as we age.4
Rapid Eye Movement (REM) sleep
This stage of sleep is characterized by rapid eye movement, abundance of dreaming and heightened brain activity. During REM, there is total body paralysis with exception of ocular and respiratory muscles. It is theorized that your body is paralyzed during this stage to protect you from dream enactment. You experience more REM the longer you sleep. REM has been shown to be essential for memory consolidation, cognitive function, mood regulation and for coping with stress. This stage is particularly compromised by sedatives including but not limited to alcohol, benzodiazepines, and tetrahydro-cannabinoid (THC). Several studies in animals and humans showed that even modest REM sleep deprivation can result in increased mortality. 2,5,6
All sleep stages are extremely essential. Be careful of self-medicating with sleep aids such benzodiazepines or alcohol as this can be detrimental for your health. In later UMEM pearls, we will discuss protocols, supplements and behavioral ways to improve each stage of sleep for better mental and physical health.
References:
1 Miyazaki S, Liu C-Y, Hayashi Y. Sleep in vertebrate and invertebrate animals, and insights into the function and evolution of sleep. Neuroscience Research. 2017;118:3-12. doi:10.1016/j.neures.2017.04.017
2 JF; PAVK. Physiology, sleep stages. National Center for Biotechnology Information. Accessed May 26, 2024. https://pubmed.ncbi.nlm.nih.gov/30252388/.
3 Antony JW, Schönauer M, Staresina BP, Cairney SA. Sleep spindles and memory reprocessing. Trends in Neurosciences. 2019;42(1):1-3. doi:10.1016/j.tins.2018.09.012
4 El Shakankiry H. Sleep physiology and sleep disorders in childhood. Nature and Science of Sleep. Published online September 2011:101. doi:10.2147/nss.s22839
5 Della Monica C, Johnsen S, Atzori G, Groeger JA, Dijk D-J. Rapid eye movement sleep, sleep continuity and slow wave sleep as predictors of cognition, mood, and subjective sleep quality in healthy men and women, aged 20–84 years. Frontiers in Psychiatry. 2018;9. doi:10.3389/fpsyt.2018.00255
6 Leary EB, Watson KT, Ancoli-Israel S, et al. Association of Rapid Eye Movement Sleep with mortality in middle-aged and older adults. JAMA Neurology. 2020;77(10):1241. doi:10.1001/jamaneurol.2020.2108
