Category: Pediatrics
Keywords: pediatrics, sepsis, SIRS, septic shock (PubMed Search)
Posted: 4/5/2024 by Kelsey Johnson, DO
(Updated: 2/8/2026)
Click here to contact Kelsey Johnson, DO
Sepsis remains a leading cause of mortality in the pediatric population, and we have long been overdue for an update in recognizing and risk stratifying our pediatric patients.
Until now, pediatric sepsis screening guidelines have followed a framework modeled after the adult screening criteria from 2001 (Sepsis-2): Systemic Inflammatory Response Syndrome (SIRS). While attempts were made in 2005 to adjust these criteria to the pediatric population, data has shown poor specificity correlating to PICU admissions, need for critical interventions, end organ damage, and mortality.
As a reminder: Pediatric SIRS criteria: Temp >38.5 C or <36 C, tachycardia (or bradycardia if <1yr old), Tachypnea, leukocytosis/ leukopenia or >10% bandemia
In 2016, Sepsis-3 revised the criteria for sepsis and septic shock for the adult cohort by placing the focus on the presence of life-threatening organ dysfunction, which led to adopting criteria such as the SOFA and qSOFA scores to predict mortality risk.
Enter: The Phoenix Sepsis Score
An international, multidisciplinary task force convened by the Society of Critical Care Medicine in 2019 used evidence from an international survey, systematic review and meta-analysis to develop and validate a scoring tool intended to identify life-threatening organ dysfunction in children. Scoring tool was derived and validated retrospectively using an international, multi-center electronic medical record review of 3 million pediatric hospital encounters (excluding pre-term infants born <37 weeks and birth hospitalizations).
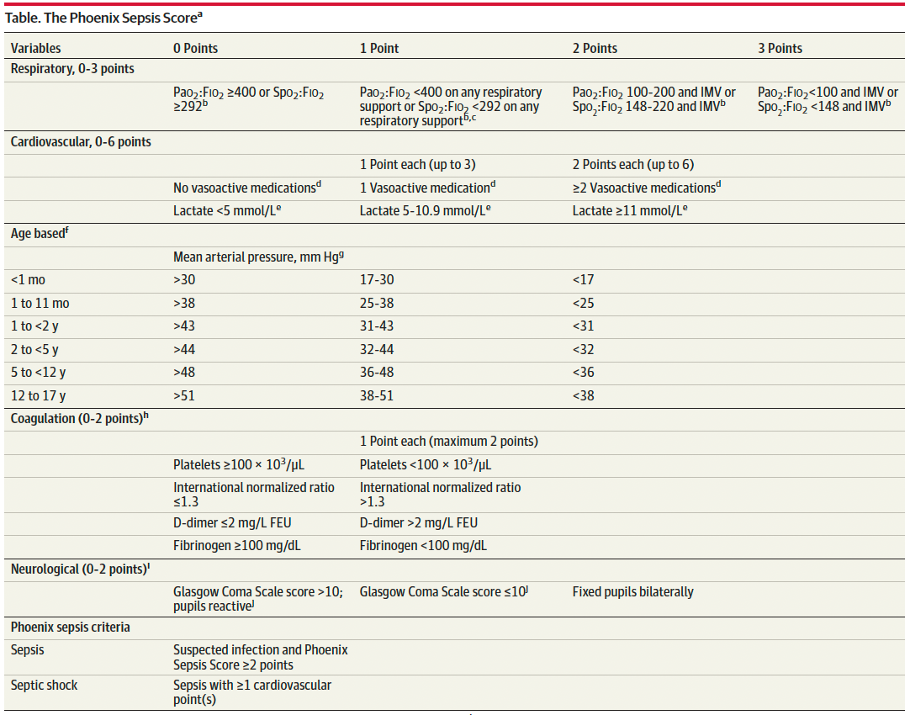
A Phoenix score of at least 2 carried a 7.1% risk of in-hospital mortality (in higher resource settings such as the USA).
Children with sepsis and organ dysfunction remote from the primary site of infection (eg respiratory failure in a child with meningitis) carried the highest mortality burden (8%) in this study.
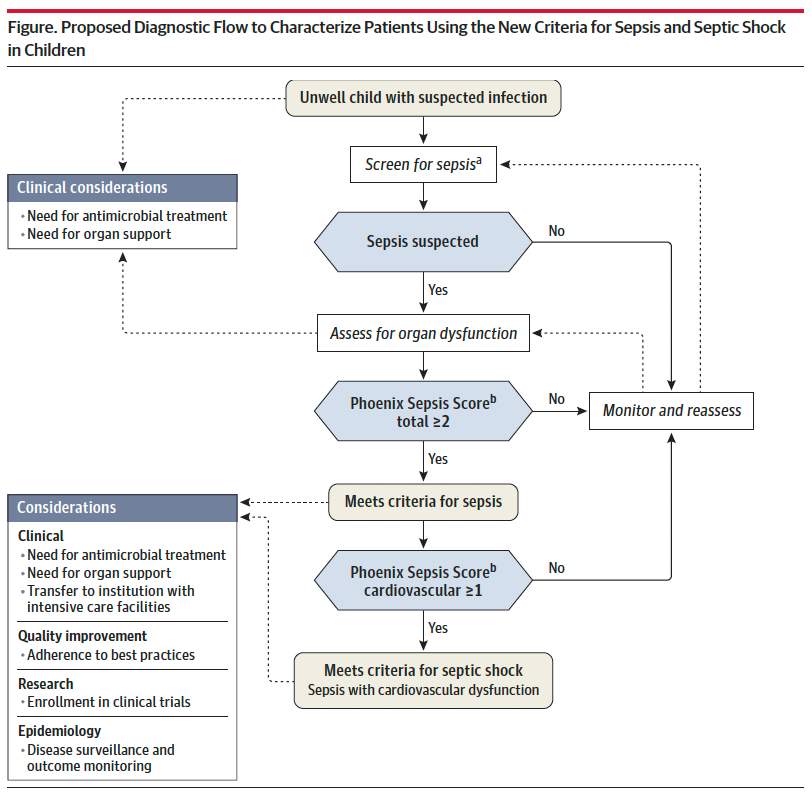
Sepsis is identified in children with suspected infection and an overall Phoenix score of 2 or more points, as this indicates potentially life-threatening organ dysfunction and thus carries higher mortality risk. Septic shock is identified by a score of 1 or more point(s) in cardiovascular dysfunction.
Lastly, it is important to recognize that this scoring criteria is NOT a sepsis screening tool, but rather should be applied when there is clinical suspicion for significant infection in the unwell child, or meeting sepsis screening criteria per your institutional criteria. Screening pediatric patients remains a clinical challenge, and there is not yet a reliable tool to apply to this population.
Bottom Line: Sepsis remains a significant cause of pediatric morbidity and mortality. The Phoenix Sepsis Score should be applied to the unwell child with suspected infection to identify sepsis and septic shock, thereby providing risk stratification and improving clinical care. Sepsis is defined by a Phoenix score of 2 or more and septic shock by a score of 1 or more in the cardiovascular category.
Schlapbach LJ, Watson RS, Sorce LR, et al. International Consensus Criteria for Pediatric Sepsis and Septic Shock. JAMA. 2024;331(8):665–674. doi:10.1001/jama.2024.0179
Category: Obstetrics & Gynecology
Keywords: postpartum, hemorrhage, pregnancy, maternal (PubMed Search)
Posted: 4/4/2024 by Michele Callahan, MD
Click here to contact Michele Callahan, MD
Postpartum hemorrhage (defined as >500 mL blood loss after birth by the WHO and >1000 mL blood loss within 24 hours of birth by ACOG), accounts for 27% of maternal deaths worldwide. It is the leading cause of maternal complications and death worldwide, with approximately 70,000 deaths globally.
In a randomized trial published in the NEJM in 2023, they implemented a bundle of first-response treatments including uterine massage, uterotonic medications, and tranexamic acid and compared this intervention group with a control group providing "usual care". They concluded that early detection of PPH and use of bundled treatment led to a lower risk of postpartum hemorrhage, lower need for laparotomy for bleeding, or lower risk of death from bleeding compared with usual care amongst patients having a vaginal delivery.
This study confirms the already widely-published recommendations for prevention of PPH with active management of the third stage of labor using prophylactic uterotonic medication (most commonly Oxytocin), uterine massage for atony, early cord clamping, and controlled cord traction for delivery of the placenta. Prompt escalation to more aggressive management (including blood transfusion, TXA, and more invasive treatments such as uterine tamponade or surgical intervention) should occur when initial treatments fail.
Gallos I, Devall A, Martin J, et al. Randomized Trial of Early Detection and Treatment of Postpartum Hemorrhage. The New England Journal of Medicine. 2023 Jul;389(1):11-21. DOI: 10.1056/nejmoa2303966. PMID: 37158447.
Category: EMS
Keywords: cardiac arrest, ECMO, E-CPR, mechanical ventilation (PubMed Search)
Posted: 4/3/2024 by Ben Lawner, MS, DO
Click here to contact Ben Lawner, MS, DO
BACKGROUND:
The ideal strategy for out of hospital ventilation is a matter of long standing debate and clinical controversy. To date, improved out of hospital outcomes have been associated with non invasive (BVM) and supraglottic airway (SGA) management strategies. A recent, prospective trial featured in Resuscitation offers a slightly different perspective. The trial enrolled 420 adult patients with refractory out of hospital cardiac arrest due to a shockable rhythm. The study looked at outcomes for patients who received endotracheal intubation (ETI) or supraglottic airway placement. Importantly, the study involved a high volume cannulation center and codified screening criteria for eCPR including: a) ongoing arrest despite 3 shocks, b) treatment with amiodarone, c) mechanical CPR and d) anticipated time to arrival at ECMO cannulation center of <30 minutes.
OUTCOMES:
Compared to patients in the SGA group, patients receiving ETI demonstrated:
In accordance with the study institution's cannulation criteria, more patients in the SGA group were deemed ineligible for ECMO.
BOTTOM LINE:
In this single center study, patients who received ETI as a primary strategy for out of hospital airway management were more likely to meet ECMO eligibility critera and exhibit improved oxygenation and ventilation.
While this is not necessarily a practice changing article, it illustrates the complexities inherent in out of hospital cardiac arrest management. EMS has largely transitioned from a “scoop and run” cardiac arrest strategy to a plan that emphasizes treat in place. For patients who may benefit from E-CPR, additional research is indicated to shed light on best out of hospital resuscitation (and airway management) practices.
Bartos JA, Clare Agdamag A, Kalra R, Nutting L, Frascone RJ, Burnett A, Vuljaj N, Lick C, Tanghe P, Quinn R, Simpson N, Peterson B, Haley K, Sipprell K, Yannopoulos D. Supraglottic airway devices are associated with asphyxial physiology after prolonged CPR in patients with refractory Out-of-Hospital cardiac arrest presenting for extracorporeal cardiopulmonary resuscitation. Resuscitation. 2023 May;186:109769. doi: 10.1016/j.resuscitation.2023.109769. Epub 2023 Mar 17. PMID: 36933882.
Category: Critical Care
Keywords: IV Fluid, balanced solutions (PubMed Search)
Posted: 4/3/2024 by Mark Sutherland, MD
(Updated: 2/8/2026)
Click here to contact Mark Sutherland, MD
Multiple studies have suggested differences in patient outcomes with balanced solutions (e.g. plasmalyte) vs unbalanced solutions (e.g. normal saline) when large volumes are administered. But what about when giving smaller volumes of fluid? Does it matter which one you choose?
A recent study by Raes et al in the Journal of Nephrology looked at urine and serum effects of administering 1L of normal saline, vs 1L of plasmalyte, to ICU patients needing a fluid bolus. Chloride levels, strong ion difference (SID), and base excess were all significantly different between the two groups. There was no difference in blood pressure or need for vasopressors. As best I can tell, other clinically significant differences such as kidney injury were unfortunately not reported.
Bottom Line: When giving small (e.g. 1L) volumes of IVF, there ARE real physiologic differences seen between balanced and unbalanced solutions. Whether these differences translate to patient-oriented or clinically significant outcomes remains unclear.
Raes, M., Kellum, J. A., Colman, R., Wallaert, S., Crivits, M., Viaene, F., Hemeryck, M., Benoît, D., Poelaert, J., & Hoste, E. (2024). Effect of a single small volume fluid bolus with balanced or un-balanced fluids on chloride and acid–base status: a prospective randomized pilot study (the FLURES-trial). JN. Journal Of Nephrology (Milano. 1992). https://doi.org/10.1007/s40620-024-01912-z
Category: Ultrasound
Keywords: POCUS; Ultrasound Artifacts (PubMed Search)
Posted: 4/1/2024 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
Ultrasound artifacts can sometimes be helpful, but sometimes they can be misleading.
For example:
1)Does this patient have a gallstone?
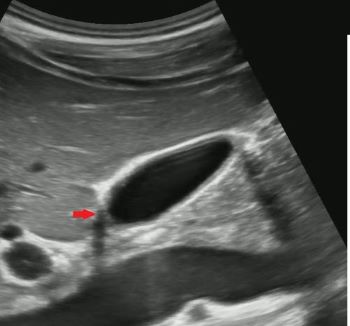
No, this is edge artifact! This is due to the ultrasound signals refracting off the side of the gallbladder wall.

No, this is side lobe artifact! This is due to a bright reflector outside of the central beam of the ultrasound signal that the machine mistakenly places with in the center of the beam. Side lobe artifact can occur near fluid filled masses such as the gallbladder and bladder.

No, this is mirror artifact!! This is due to ultrasound signals bouncing off a highly reflective surface such as the diaphragm. The ultrasound machine misinterprets the time delay from the reflected ultrasound signal as a structure deeper in the image.
Category: Toxicology
Keywords: Alcohol, mortality, predictor, trauma (PubMed Search)
Posted: 3/31/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This retrospective population cohort study looked at first time ED visits for adolescents and young adults comparing those with visits related to alcohol to those not related to alcohol. Patients in the alcohol related visit group had a threefold increased one year mortality rate. Cause of death was trauma, poisoning by drug and alcohol. Risk factors include being male, age 20-29, history of mental health and having a visit for withdrawal.
Adolescents and young adults presenting to an emergency department for an alcohol related complaint are high risk for one year mortality and deserve intervention and appropriate referral.
Academic Emergency MedicineVolume 31, Issue 3 p. 220-229
Mortality in adolescents and young adults following a first presentation to the emergency department for alcohol
Lyndsay D. Harrison MSc, Asnake Y. Dumicho MSc, Anan Bader Eddeen MSc, Peter Tanuseputro MD, MHSc, Claire E. Kendall MD, PhD, Jess G. Fiedorowicz MD, PhD, Tea Rosic MD … See all authors
Category: Misc
Posted: 3/26/2024 by Heidi Teague, MD
(Updated: 3/30/2024)
Click here to contact Heidi Teague, MD
Advancements in complex illness management have led to an increasing number of patients surviving longer, with subsequent development of end-stage organ disease, cancer, and dementia. EDs are encountering patients with more complex medical needs who present with challenging complaints such as functional loss, bounce-back visits for uncontrolled symptoms, and caregiver fatigue. ACEP underscored the importance of advancing access to palliative care in 2013 and is one of its top five measures in the Choosing Wisely campaign, aimed at minimizing unwarranted and excessive medical interventions. Proactive symptom management, including promptly addressing pain, dyspnea, nausea, and other distressing symptoms, as well as goals of care conversations, and early referral to hospital and outpatient palliative services can enhance patient and caregiver comfort and quality of life.
Wang DH. Beyond Code Status: Palliative Care Begins in the Emergency Department. Annals of emergency medicine. 2017;69(4):437-443. doi:10.1016/j.annemergmed.2016.10.027
Category: Pediatrics
Posted: 3/29/2024 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Standard practice regarding various pediatric fractures has started to shift over the last several years, often to less restrictive means of treatment. Torus (buckle) fractures of the distal radius are one of the most common pediatric fractures and tend to heal very well with minimal intervention.
The FORCE study (FOrearm fracture Recovery in Children Evaluation), a multicenter study out of the UK, was conducted to compare rigid immobilization (splinting) to a soft bandage used as needed per family discretion for treatment of these fractures. There was no different in outcomes of self-reported pain, function, quality of life, complications, or school absences. UK orthopedic guidelines have been updated to reflect a recommendation against rigid immobilization as well as against any need for specialist follow-up. American guidelines are slower to follow suit, but in recent years have transitioned to an approach of a removable brace.
Take Home: Pediatric torus fractures of the distal radius likely do not require immobilization and can be managed with self-limited activity instead. Practice in the US is in flux, but it is reasonable to manage with a removable brace or soft dressing as well as pediatrician follow up.
Hussain, M, Perry, D, and Messahel, S. Summary of Recent Advances in Management of Torus Fracture of the Distal Radius in Children_. Arch Dis Child_. Epub ahead of print
Knight R, Dritsaki M, Mason J, Perry DC, Dutton SJ. The Forearm Fracture Recovery in Children Evaluation (FORCE) trial: statistical and health economic analysis plan for an equivalence randomized controlled trial of treatment for torus fractures of the distal radius in children. Bone Jt Open. 2020 Jun 9;1(6):205-213.
Category: Misc
Posted: 3/12/2024 by Mike Witting, MS, MD
(Updated: 3/28/2024)
Click here to contact Mike Witting, MS, MD
Considering starting a research project? Apply the FINER criteria:
Feasible
Do you have the resources to study this? Enough patients? Support?
Interesting
Does it interest you enough to devote your time to it? Does it interest colleagues?
Novel
Would it provide new findings, or confirm, refute, or extend prior findings?
Ethical
Can you think of a way to ethically study it?
Relevant
Consider possible outcomes of your research. Could the study advance care or policy?
Adapted from Hulley SB, Cummings SR. Designing clinical research, 4th edition, Lippincott, Williams and Wilkins, 2013.
Category: Administration
Keywords: Administration, Patient Experience, Microaggression, Discrimination (PubMed Search)
Posted: 3/27/2024 by Mercedes Torres, MD
(Updated: 2/8/2026)
Click here to contact Mercedes Torres, MD
Do microaggressions and discrimination impact the patient experience in your ED? How can we address this?
This article is one of few studies to address this topic specifically in the ED. Authors used quantitative (discrimination scale) and qualitative (follow-up interviews) methods to answer this question in two urban academic EDs.
Common themes from patient responses provide food for thought and action in this regard:
Punches BE, Osuji E, Bischof JJ, et al. Patient perceptions of microaggressions and discrimination toward patients during emergency department care. Acad Emerg Med. 2023; 30: 1192-1200. doi:10.1111/acem.14767
Category: Critical Care
Posted: 3/26/2024 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Bag-Valve-Mask Ventilation During OHCA
Idris AH, et al. Bag-valve-mask ventilation and survival from out-of-hospital cardiac arrest: A multicenter study. Circulation. 2023;148:1847-56.
Category: Trauma
Keywords: Alcohol, withdrawal, trauma, protocol, sparing (PubMed Search)
Posted: 3/24/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This study compared admitted trauma patients with alcohol withdrawal or those at risk of withdrawal before and after a benzodiazepine sparing protocol (using clonidine and gabapentin) was initiated. They found a lower daily CIWA score and significantly less lorazepam use in the benzodiazepines sparing group. This sparing protocol appears to be safe and effective.
McCullough, Mary Alyce MD; Miller, Preston R. III MD; Martin, Tamriage MD; Rebo, Kristin A. PharmD; Stettler, Gregory R. MD; Martin, Robert Shayn MD; Cantley, Morgan PharmD; Shilling, Elizabeth H. PhD; Hoth, James J. MD, PhD; Nunn, Andrew M. MD
Journal of Trauma and Acute Care Surgery 96(3):p 394-399, March 2024. | DOI: 10.1097/TA.0000000000004188
Category: Orthopedics
Posted: 3/23/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
The OPAL trial attempted to investigate the effectiveness of opioids in the acute management of neck and back pain.
346 adults presenting to the Emergency department or primary care provider with 12 weeks or less of lower back pain, neck pain or both (of at least moderate intensity).
51% male. 49% female.
Location: Sydney, Australia
All participants received guideline care (advice to stay active, reassurance of a positive prognosis, avoidance of bed rest, and, if required, other non-opioid analgesics).
Patients were then randomly assigned to an opioid (oxycodone, up to 20 mg PO qD) or and an identical placebo, for up to 6 weeks*.
*Trial used a combination oxycodone/naloxone to reduce risk of opioid induced constipation and assist with blinding.
*Trial used a modified release formulation that could be dosed q12h rather than q4-6h to increase adherence.
*Recommended regimen was oxycodone 5mg every 12 hours, with titration as necessary, max dose 20mg total per day.
*Trial physicians were able to individualize the prescription to suit the patient’s needs.
* Mean prescribed dose was approx. oxycodone 10mg total daily.
*Most patients only treated for 2 weeks
Primary outcome: Pain severity at 6 weeks
Results: Mean pain score at 6 weeks was identical between groups.
Trend towards faster recovery in the placebo group in the first 2 weeks.
Take home: Consider the likely benefit vs harm of prescribing opioids for acute back and neck pain in the ED.
Friedman BW, Irizarry E, Chertoff A, Feliciano C, Solorzano C, Zias E, Gallagher EJ. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department-based Randomized Study. Acad Emerg Med. 2020 Mar;27(3):229-235.
Category: EMS
Keywords: Suicide, EMS, prevention, causes (PubMed Search)
Posted: 3/20/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
7,365 suicide related cardiac arrests were included in this study that included a several year study period in Queensland Australia. Cardiac arrests where resuscitation was attempted by EMS and where circumstances were concerning for suicide were included. ROSC rates were 28.6% with survival at 30 days being only 8%. 30-day survival for medical cardiac arrests in this jurisdiction was 16.4%. Overdose and poisoning had the best survival rate (19.9%), while hanging and chemical asphyxia were the worst (7.3 and 1.1% respectively).
Bottom line: Survival rates for suicide related out of hospital cardiac arrest were worse compared to other causes of medical arrest. Suicide prevention should become a focus with emphasis on early identification and treatment of people at high risk of suicide. While EMS is well trained on the management of cardiac arrest, training should also emphasize suicide risk assessment and identification.
Doan et al. Suicide related out-of-hospital cardiac arrests in Queensland, Australia: temporal trends of characteristics and outcomes over 14 years. Prehospital Emergency Care. 2023.
Category: Critical Care
Keywords: ROSC, OHCA, cardiac arrest, shock, vasopressors, norepinephrine, noradrenaline, epinephrine, adrenalin (PubMed Search)
Posted: 3/19/2024 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Post-arrest shock is a common entity after ROSC. There is support for the use of continuous norepinephrine infusion over epinephrine to treat shock after ROSC, due to concerns about increased myocardial oxygen demand and associations with higher rates of rearrest [1,2] and mortality [2,3] with the use of epinephrine compared to norepinephrine, and increased refractory shock with use of epinephrine infusion after acute MI [4].
An article in this month’s AJEM compared norepinephrine and epinephrine infusions to treat shock in the first 6 hours post-ROSC in OHCA [5]. With a study population of 221 patients, they found no difference in the primary outcome of incidence of tachyarrhythmias, but did find that in-hospital mortality and rearrest rates were higher in the epinephrine group.
Bottom Line: Absent definitive evidence, norepinephrine should probably be the first pressor you reach for to manage post-arrest shock, especially if there is strong suspicion for acute myocardial infarction.
Category: Trauma
Keywords: Geriatric trauma, outcome, hospice (PubMed Search)
Posted: 3/17/2024 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
This was a database study of nearly 2 million trauma patients over age 65 who were discharged looking at all levels of trauma centers. The authors found:
“Dominance analysis showed that proportion of patients with Injury Severity Score of >15 contributed most to explaining hospice utilization rates (3.2%) followed by trauma center level (2.3%), proportion White(1.9%), proportion female (1.5%), and urban/rural setting (1.4%).”
Level one centers had the lowest level of discharge to hospice. The authors felt: “As the population ages, accurate assessment of geriatric trauma outcomes becomes more critical. Further studies are needed to evaluate the optimal utilization of hospice in end-of-life decision making for geriatric trauma.”
Fakhry, Samir M. MD, FACS; Shen, Yan PhD; Wyse, Ransom J. MPH; Garland, Jeneva M. PharmD; Watts, Dorraine D. PhD
Journal of Trauma and Acute Care Surgery 94(4):p 554-561, April 2023. | DOI: 10.1097/TA.0000000000003883
Category: Administration
Keywords: Ramadan, fasting (PubMed Search)
Posted: 3/16/2024 by Kevin Semelrath, MD
(Updated: 2/8/2026)
Click here to contact Kevin Semelrath, MD
This study is out of the American University of Beirut, Lebanon, and courtesy of our own Mazen El Sayed!
Many patients of Muslim faith will observe fasting during the month of Ramadan, with no food, water, oral of IV medication taken from sunrise to sunset
This study showed a lower daily ED volume than during non Ramadan months, however did show a higher length of stay during Ramadan.
It also found an increase in mortality rates during Ramadan (OR 2.88) and 72 hour ED bounce-backs (OR 1.34)
Be sensitive and aware of the needs of your patients of Muslim faith during this holy month of fasting.
Ramadan Kareem
Impact of Ramadan on emergency department visits and on medical emergencies. Reem G Al Assaad, Rana Bachir, Mazen J. El Sayed. Europena Journal of Emergency Medicine. 2018, 25:440-444.
Category: Pediatrics
Keywords: Pediatric intubation, airway, cuffed, depth (PubMed Search)
Posted: 3/15/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
The gold standard for confirming ETT position is a chest xray, but this can often be delayed while the patient is stabilized. Many physicians will estimate ETT insertion depth to be 3x the ETT size, but this is based on selection of the correct tube. There are several other published formulas, including the PALS guidelines [age in years/2 + 12] which applies to children older than one year. In 1982, there was an article published that cited the formulas of [Height (cm) x 0.1 +5] or [Weight(kg)/5 + 12].
This was a retrospective study where the ideal position of cuffed ETT (from the front teeth) was determined by looking at post intubation xrays of 167 patients between 28 days and 18 years. The individual optimal ETT insertion depth was plotted against age, weight and height for all children. This study showed that there is not a fully linear relationship between age, height or weight which is a flaw of all of these formulas. Calculations using the patients’ weight performed the worst. Age based and height formulas performed the best.
Ebenebe et al. Recommendations for endotracheal tube insertion depths in children. Emerg Med J 2023; 0:1-5. epub ahead of print.
Category: Pharmacology & Therapeutics
Keywords: Bactrim, skin and soft tissue infections, Streptococcus spp (PubMed Search)
Posted: 3/14/2024 by Wesley Oliver
Click here to contact Wesley Oliver
MYTH: Bactrim cannot be used as monotherapy for nonpurulent skin and soft tissue infections.
Not True!
Organisms of concern: Streptococcus spp.
Here’s why:
TRUTH: Bactrim CAN be used as monotherapy for nonpurulent skin and soft tissue infections.
Prepared by Rianna Fedora, PharmD on 2/26/24
Category: Critical Care
Posted: 3/12/2024 by Quincy Tran, MD, PhD
(Updated: 2/8/2026)
Click here to contact Quincy Tran, MD, PhD
Background: There is no clear guidelines regarding whether norepinephrine or epinephrine would be the preferred agent to maintain hemodynamic stability after cardiac arrest. In recent years, there has been more opinions about the use of norepinephrine in this situation.
Settings: retrospective multi-site cohort study of adult patients who presented to emergency departments at Mayo Clinic hospitals in Minnesota, Florida, Arizona with out-of-hospital-cardiac arrest (OHCA). Study period was May 5th, 2018, to January 31st, 2022
Participants: 18 years of age and older
Outcome measurement: tachycardia, rate of re-arrest during hospitalization, in-hospital mortality.
Multivariate logistic regressions were performed.
Study Results:
Discussion:
It was retrospective study that uses electronic health records. Thus, other important factors from the pre-hospital settings might not be accurate.
On the other hand, the patient population came from multiple hospitals with varying practices so the patient population is more generalizable.
Conclusion:
Although the rate of tachyarrhythmia was not different between patients receiving norepinephrine vs. epinephrine after ROSC. This study would add more data to the current literature that norepinephrine might be more beneficial for patients with post-cardiac arrest shock.
Normand S, Matthews C, Brown CS, Mattson AE, Mara KC, Bellolio F, Wieruszewski ED. Risk of arrhythmia in post-resuscitative shock after out-of-hospital cardiac arrest with epinephrine versus norepinephrine. Am J Emerg Med. 2024 Mar;77:72-76. doi: 10.1016/j.ajem.2023.12.003. Epub 2023 Dec 10. PMID: 38104386.
