Category: Critical Care
Keywords: map, sepsis, septic shock, hypertension (PubMed Search)
Posted: 4/7/2014 by Feras Khan, MD
(Updated: 4/8/2014)
Click here to contact Feras Khan, MD
How low should you go? MAP Goals in Septic Shock
Background:
The Trial:
Outcome:
Bottom Line:
Pierre Asfar, M.D., Ph.D. et al. for the SEPSISPAM Investigators
March 18, 2014DOI: 10.1056/NEJMoa1312173
Category: Visual Diagnosis
Posted: 4/7/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
23 year-old female presents complaining of progressive right lower quadrant pain after doing "vigorous" pushups. CT abdomen/pelvis below. What’s the diagnosis? (Hint: it’s not appendicitis)

Answer: Rectus sheath hematoma
Rectus Sheath Hematoma (RSH)
Rectus muscle tear causing damage to the superior or inferior epigastric arteries with subsequent bleeding into the rectus sheath; uncommon cause of abdominal pain but mimics almost any abdominal condition.
May occur spontaneously, but suspect with the following risk factors:
Typically a self-limiting condition, but hypovolemic shock may result from significant hematoma expansion.

Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/31/2014 by Semhar Tewelde, MD
(Updated: 4/6/2014)
Click here to contact Semhar Tewelde, MD
Perinatally Infected HIV & Cardiovascular Disease
*Perinatally HIV-infected adolescents are susceptible to aggregate atherosclerotic cardiovascular disease risk, but few studies have quantified risk or developed a scoring system
*A recent study of perinatally HIV-infected adolescents calculated coronary artery and abdominal aorta PDAY (Pathobiological Determinants of Atherosclerosis in Youth) scores using modifiable risk factors: HTN, HLD, smoking, obesity and hyperglycemia
*Significant predictors of a high coronary arteries and abdominal aorta scores include: male sex, Hx AIDS-defining condition, long duration of ritonavir-boosted protease inhibitor, and no prior use of tenofovir
*PDAY scores may be useful in identifying high-risk youth who may benefit from early lifestyle or clinical interventions given their trend of increased aggregate atherosclerotic cardiovascular disease risk factor burden
Patel K, Et al. Aggregate Risk of Cardiovascular Disease Among Adolescents in Perinatally Infected with the Human Immunodeficiency Virus. Circulation Vol 129(11) 18 March 2014, p1204-1212.
Category: Pharmacology & Therapeutics
Keywords: azithromycin, levofloxacin, cardiovascular risk, mortality, dysrhythmia (PubMed Search)
Posted: 3/24/2014 by Bryan Hayes, PharmD
(Updated: 4/5/2014)
Click here to contact Bryan Hayes, PharmD
A new study of almost 2 million prescriptions in VA patients compared the risk of cardiovascular death or dysrhythmia in patients receiving azithromcyin, levofloxacin, and amoxicillin.
What they found
Compared with amoxicillin, azithromycin was associated with a significant increase in mortality (HR = 1.48; 95% CI, 1.05-2.09) and dysrhythmia risk (HR = 1.77; 95% CI, 1.20-2.62) on days 1 to 5, but not 6 to 10.
Levofloxacin was associated with an increased risk throughout the 10-day period. Days 1-5 mortality (HR = 2.49, 95% CI, 1.7-3.64) and serious cardiac dysrhythmia (HR = 2.43, 95% CI, 1.56-3.79). Days 6-10 mortality (HR = 1.95, 95% CI, 1.32-2.88) and dysrhythmia (HR = 1.75; 95% CI, 1.09-2.82).
Important limitations
This study did not have a comparator group of patients getting no antibiotics. Previous data suggest patients on any antibiotic (eg, penicillin) have a higher risk of death or dysrhythmia.
The supplemental index shows that patients receiving azithromycin and levofloxacin had more serious infections (eg, PNA, COPD, etc.) which may have put them at higher risk for worse outcome irrespective of antibiotic choice.
What it means
It seems azithromycin and levofloxacin may contribute to a small increase in cardiovascular mortality and dysrhythmia during their use. A previous study found this is more likely in those with existing cardiovascular disease.
Rao GA, et al. Azithromyicin and levofloxacin use and increased risk of cardiac arrhythmia and death. Ann Fam Med 2014;12(2):121-7. [PMID 24615307]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: naloxone,overdose,heroin,opioid (PubMed Search)
Posted: 4/3/2014 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
1. https://www.networkforphl.org/_asset/qz5pvn/network-naloxone-10-4.pdf (Contains each law per state as of March 15, 2014)
2. http://www.usatoday.com/story/news/nation/2014/02/20/stateline-drug-overdose-deaths/5637519/
3. Intranasal Naloxone for Treatment of Opioid Overdose. The Medical Letter. Volume 56 (Issue 1438). March 17, 2014
Category: International EM
Keywords: HIV, global health, infectious disease, rash, puritis (PubMed Search)
Posted: 4/1/2014 by Andrea Tenner, MD
(Updated: 4/2/2014)
Click here to contact Andrea Tenner, MD
You are working in a clinic in Tanzania (or Baltimore, for that matter) when a 24 year old presents with this itchy rash on his feet. What's the diagnosis and what underlying systemic condition does it indicate?
Pruritic Papular Eruptions in HIV
Presentation:
University of Maryland Section for Global Emergency Health
Authors: Van Pham, MD and Colleen Holley, MD
Category: Critical Care
Posted: 4/1/2014 by Mike Winters, MBA, MD
(Updated: 2/8/2026)
Click here to contact Mike Winters, MBA, MD
Coagulopathies in Critical Illness - DIC
Hunt B. Bleeding and coagulopathies in critical care. NEJM 2014;370:847-59.
Category: Visual Diagnosis
Posted: 3/31/2014 by Haney Mallemat, MD
(Updated: 4/1/2014)
Click here to contact Haney Mallemat, MD
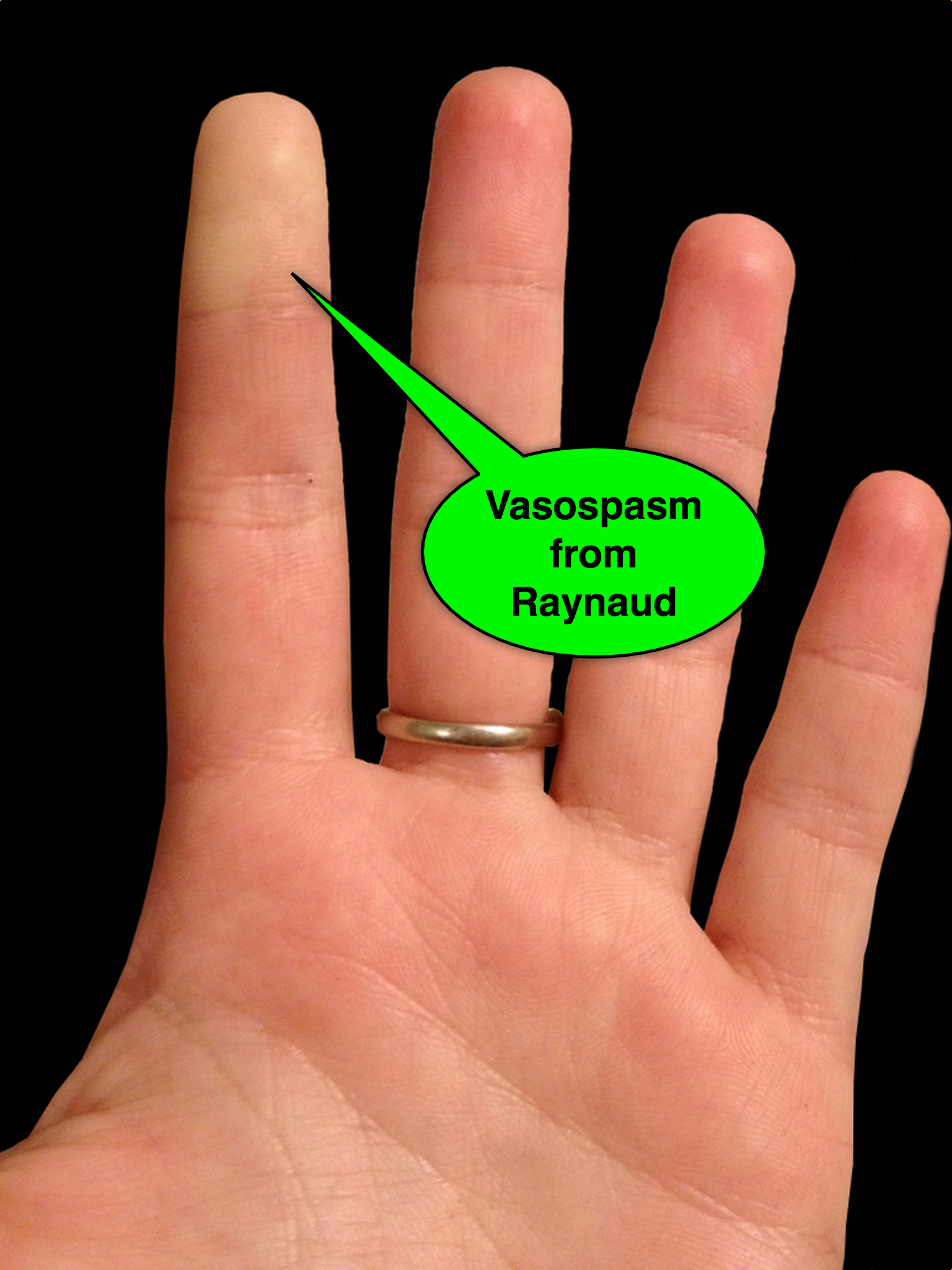
25 year-old female presents with the following. It seems to have occurred spontaneously and spontaneously resolves during her ED evaluation.

Answer: Raynaud phenomenon
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Orthopedics
Keywords: DeQuervain, Intersection, Syndrome, Tenosynovitis (PubMed Search)
Posted: 3/30/2014 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
DeQuervain and Intersection Syndromes:
Category: Toxicology
Keywords: opioids (PubMed Search)
Posted: 3/27/2014 by Fermin Barrueto
(Updated: 2/8/2026)
Click here to contact Fermin Barrueto
What are characteristics that increase the chance a patient is at risk for opioid-related death? A recent JAMA article begins to tackle this very issues. Baumblatt et al. found the following:
1) Patient with 4 or more prescribers had adjusted odds ratio 6.5 for opioid-related death
2) Patient with 4 or more pharmacies where they get their prescriptions aOR - 6.0
3) Patient with more than 100 mg of morphine equivalents mean per day aOR - 11.2
With the new Maryland Prescription Drug Monitoring program (PDMP) we can start looking at a patient's prescription drug use pattern. The recent JAMA article can help you identify patients at high risk to die an opioid-related death. Use the PDMP and be wary if a patient has more than 4 prescribers or pharmacies or has >100mg of morphine equivalents per day.
High-Risk Use by Patients Prescribed Opioids for Pain and Its Role in Overdose Deaths.
Baumblatt JA, Wiedeman C, Dunn JR, Schaffner W, Paulozzi LJ, Jones TF.
JAMA Intern Med. 2014 Mar 3. doi: 10.1001/jamainternmed.2013.12711. [
Category: International EM
Keywords: multiple myeloma, x-ray, global, neoplasm (PubMed Search)
Posted: 3/26/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
You are evaluating a 40 year old trauma victim and see this on pelvic xray. What are you worried about?

University of Maryland Section for Global Emergency Health
Authors: Colleen Holley, MD and Van Pham, MD
Mulligan, Michael. Multiple Myeloma Imaging. available: http://emedicine.
Category: Critical Care
Keywords: ARDS, Nitric Oxide, acute respiratory failure, mechanical ventilation (PubMed Search)
Posted: 3/23/2014 by John Greenwood, MD
(Updated: 3/26/2014)
Click here to contact John Greenwood, MD
Nitric Oxide appears to have NO role in ARDS
Background: The use of inhaled nitric oxide (iNO) in acute respiratory distress syndrome (ARDS) & severe hypoxemic respiratory failure has been thought to potentially improve oxygenation and clinical outcomes. It is estimated that iNO is used in up to 14% of patients, despite a lack of evidence to show improved outcomes.
Mechanism: Inhaled NO works as a selective pulmonary vasodilator which has been found to improve PaO2/FiO2 by 5-13%, but is costly ($1,500 - $3,000 per day) and increases risk of renal failure in the critically ill.
Study: A recent systematic review analyzed 9 different RCTs (N=1142) and compared mortality between those with severe (PaO2/FiO2 < 100) and less severe (PaO2/FiO2 > 100) ARDS and found that iNO does not reduce mortality in patients with ARDS, regardless of the severity of hypoxemia.
Bottom Line: Inhaled NO is an intriguing option for the treatment of refractory hypoxemic respiratory failure, however there does not appear to be a mortality benefit to justify it's high cost and potentially negative side effects. In the ED, it is important to focus on appropriate lung protective ventilation strategies (TV: 6-8 cc/kg IBW) and maintaining plateau pressures < 30 cm H2O in the initial stages of ARDS to prevent ventilator induced lung injury while awaiting ICU admission.
Reference
Adhikari NK, Dellinger RP, Lundin S, et al. Inhaled nitric oxide does not reduce mortality in patients with acute respiratory distress syndrome regardless of severity: systematic review and meta-analysis. Crit Care Med. 2014;42(2):404-12. [PMID: 24132038]
Follow me on Twitter (@JohnGreenwoodMD)
Category: Cardiology
Keywords: Cardiac arrest, LVAD, CPR, Chest compressions (PubMed Search)
Posted: 3/23/2014 by Ali Farzad, MD
Click here to contact Ali Farzad, MD
The number of patients with left ventricular assist devices (LVADs) is increasing and development of optimal resuscitative strategies is becoming increasingly important. Despite a lack of evidence, many device manufacturers and hospitals have recommended against performing chest compressions because of fear of cannula dislodgment or damage to the outflow conduit.
A recent retrospective analysis of outcomes in LVAD patients who received chest compressions for cardiac arrest did not support the theory that LVADs would be harmed by conventional resuscitation algorithms.
The study was a limited case series of only 8 LVAD patients over a 4 year period. All patients received compressions and device integrity was subsequently assessed by blood flow data from the LVAD control monitor or by examination on autopsy. Although more research is necessary to determine the utility and effectiveness of compressions in this population, none of the patients in this study had cannula dislodgment and half of the patients had return of neurologic function.
Shinar Z, Bellezzo J, Stahovich M, et al. Chest compressions may be safe in arresting patients with left ventricular assist devices (LVADs). Resuscitation. 2014. doi:10.1016/j.resuscitation.2014.01.003.
Category: Orthopedics
Keywords: ankle sprain (PubMed Search)
Posted: 3/22/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Ankle Syndesmosis Injuries are also called high ankle sprains as they involve trauma to the ligaments above the ankle joint
Most ankle sprains are lateral ankle sprains. High ankle sprains are relatively uncommon.
Usual mechanism: External rotation injuries
Exam: Tenderness at the syndesmosis and compression of the tib/fib at the mid calf level causing syndesmosis pain (squeeze test)
Median recovery time is almost 4 times as long as a lateral ankle sprain 62days vs. 15days
Emergency department care is similar tto that of other ankle sprains but the added benefit of patient education and advice may improve overall care and follow-up.
Category: Pediatrics
Keywords: Head injury, vomiting, PECARN (PubMed Search)
Posted: 3/21/2014 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Category: International EM
Keywords: echocardiography, rheumatic heart disease, endocarditis, international (PubMed Search)
Posted: 3/19/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
35yo M with history of rheumatic heart disease presents with fever. What disease process is suggested by the echo?
Burke AP. Pathology of rheumatic heart disease. Medscape. 2013. Accessed 19 Mar 2013 at http://emedicine.medscape.com/article/1962779-overview#aw2aab6b4.
Category: Critical Care
Posted: 3/19/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
In 2001, Rivers et al. published a landmark article demonstrating an early-goal directed protocol of resuscitation that reduced mortality in septic Emergency Department patients.
Many questions have arisen throughout the years with respect to that trial; critics have complained about the overwhelming change in clinical practice based on this one single-center randomized trial.
Challenging Rivers data are the ProCESS (Protocolized Care for Early Septic Shock) investigators, who released the results from a multi-center randomized control trial of 1351 septic Emergency Department patients; the primary end-point was 60-day mortality. Click here for NEJM article.
Patients in this trial were randomized to one of three groups:
Protocol-based EGDT
Protocol-based standard (did not require central lines, inotropes, or blood transfusions
Usual care (no specific protocol; care was left to the bedside clinicians)
Bottom-line: The investigators did not find any difference in mortality between patients in the three groups and comment that the most important aspects of managing the septic patient may be prompt recognition and early treatment with IV fluids and antibiotics.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Visual Diagnosis
Posted: 3/17/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
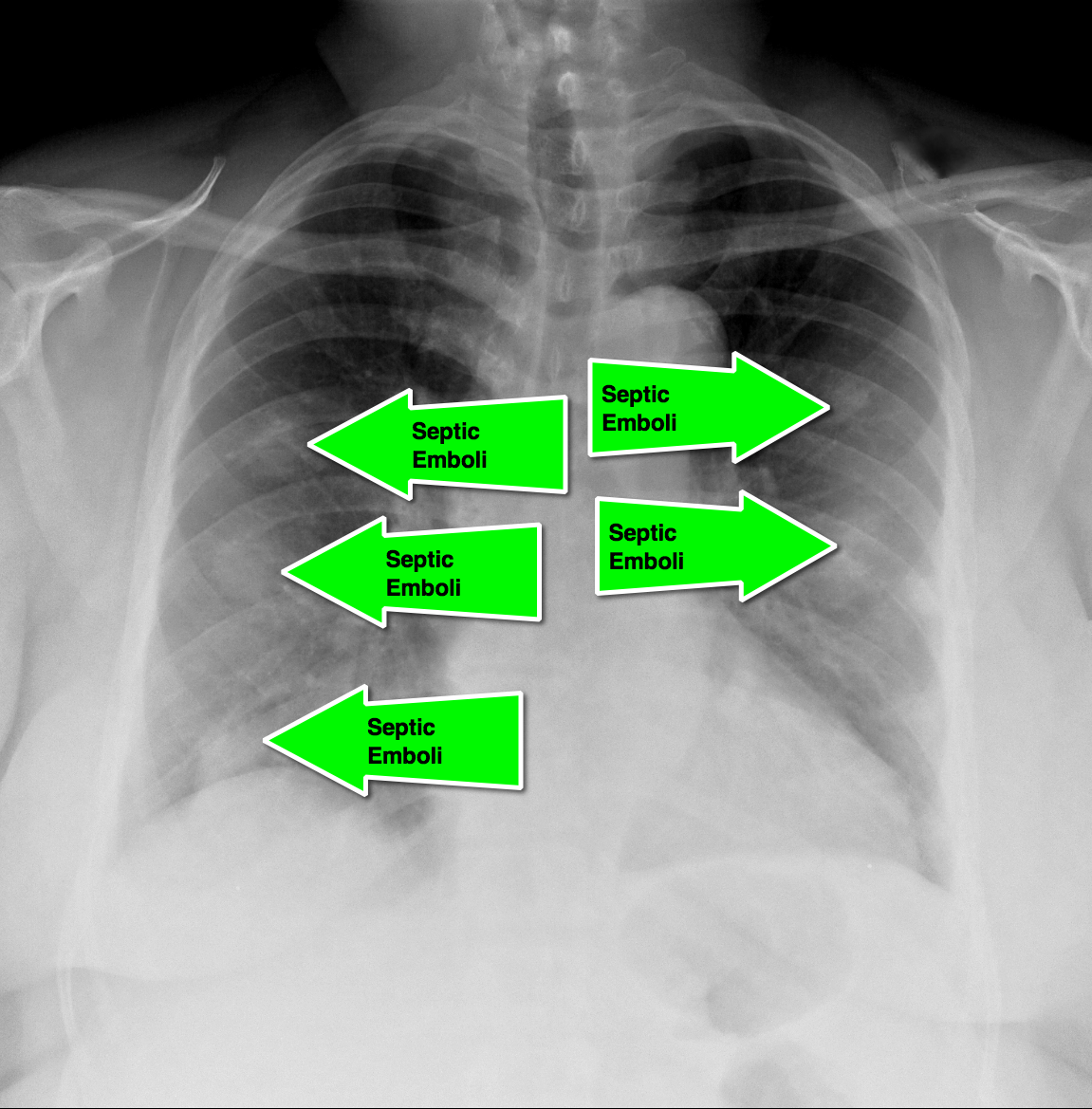
62 year-old male presents with weakness, chills, cough, and malaise. Recently, he had four teeth extracted but felt fine immediately after the extraction. Past medical history includes diabetes and hypertension; CXR is below. What’s the diagnosis?

Answer: Septic pulmonary emboli (a.k.a. pulmonary puffballs); he was eventually diagnosed with bacterial endocarditis.
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 3/16/2014 by Semhar Tewelde, MD
Click here to contact Semhar Tewelde, MD
The HEART Score
Acute coronary syndrome defines a spectrum of diseases (unstable angina, NSTEMI, STEMI), without clear ECG abnormalities the diagnosis and disposition can be challenging
Several scoring systems have attempted to risk stratify patients: TIMI, PURSUIT, and GRACE
The TIMI & PURSUIT scores were designed to identify higher-risk patients and long-term mortality
A pilot/observational study has utilized a novel scoring system to risk stratify low to intermediate risk patients
The HEART (History, ECG, Age, Risk factors and Troponin) score:
This scoring system is limited given the small study size and requires further study/validation, but may be an easy, quick, and reliable predictor of outcome in chest pain patients
Six AJ, Backus BE, Kelder JC. Chest pain in the emergency room: value of the HEART score. Neth Heart J. Jun 2008; 16(6): 191–196.
Category: Toxicology
Keywords: Carbon Monoxide, (PubMed Search)
Posted: 3/15/2014 by Michael Bond, MD
Click here to contact Michael Bond, MD
Carbon Monoxide Half-Life:
