Category: Critical Care
Keywords: lung ultrasound, pulmonary edema, B-lines (PubMed Search)
Posted: 3/11/2014 by Feras Khan, MD
Click here to contact Feras Khan, MD
1. A comet-tail artifact
2. Arising from the pleural line
3. Well defined
4. Hyperechoic
5. Long (does not fade)
6. Erases A lines
7. Moves with lung sliding
Technique
1. Lichtenstein D, Mezie re G, Biderman P, et al. The comet-tail artifact. An ultra- sound sign of alveolar-interstitial syndrome. Am J Respir Crit Care Med 1997; 156(5):1640–6.
Category: Pediatrics
Keywords: asthma, pediatrics, dexamethasone, prednisone (PubMed Search)
Posted: 3/10/2014 by Danielle Devereaux, MD
Click here to contact Danielle Devereaux, MD
Hot off the press! Pediatrics March 2014 just published results of a meta-analysis that compared 1 or 2 dose regimens of Dexamethasone versus 5 day course of Prednisone/Prednisolone for management of acute asthma exacerbations in pediatric patients. The results showed that Dexamethasone was as efficacious as the longer course of Prednisone. End points used were return trips to the emergency department and hospital admissions. On further review of the literature, parents tend to prefer the shorter duration of therapy with Dexamethasone. Also, there is less vomiting associated with Dexamethasone. There have been several articles published that show Dexamethasone is more cost-effective than Prednisone. Bottom line: consider giving single dose of Dexamethasone in the ER and then sending patient home with 1 additional dose.
Keeney G, Gray M, Morrison A, et al. Dexamethasone for Acute Asthma Exacerbations in Children: A Meta-analysis, Pediatrics March 2014, pp 493-499.
Williams K, Andrews A, Heine D, et al. Parental Preference for Short versus Long Course Corticosteroid Therapy in Children With Asthma Presenting to the Pediatric Emergency Department, Clinical Pediatrics January 2012, pp 30-34.
Andrews A, Wong K, Heine D, et al. A Cost-effectiveness Analysis of Dexamethasone versus Prednisone in Pediatric Acute Asthma Exacerbations, Annals of Emergency Medicine July 2012, pp 943-949
Category: Cardiology
Keywords: Echo, Aortic Dissection (PubMed Search)
Posted: 3/9/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
Early diagnosis and surgical consultation for dissection of the ascending aorta can be life saving. Emergency physicians are increasingly using focused cardiac ultrasound to assess chest pain patients in the ED.
The suprasternal notch view (SSNV), may provide additional information in the assessment of thoracic aortic pathology. A recently performed pilot study aimed to determine the accuracy of using the SSNV, in addition to the more traditional parasternal long axis view in assessing aortic dimensions as well as pathology compared to CTA of the chest.
Using a maximal normal thoracic aortic diameter of 40 mm, diagnostic accuracy in detecting dilation of the aorta was 100%. The study showed that the SSNV is feasible and demonstrates high agreement with measurements made on CTA of the chest.
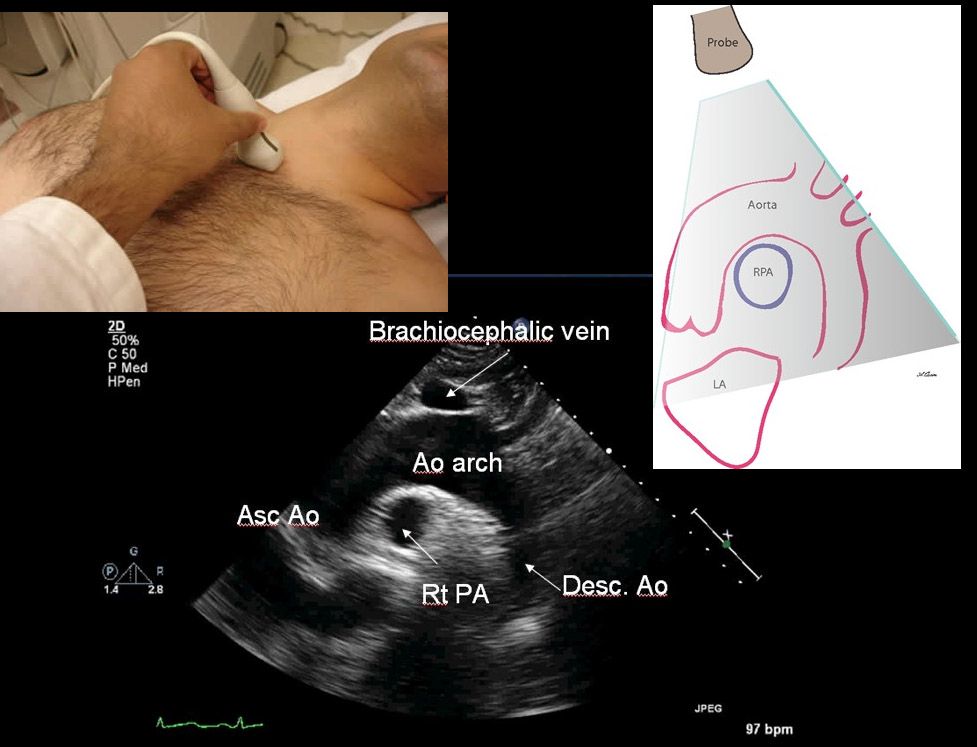
Kinnaman KA, Rempell JS, Kimberly HH, et al. Accuracy of Suprasternal Notch View Using Focused Cardiac Ultrasound to Evaluate Aortic Arch Measurements. YMEM. 2013;62(S):S81. doi:10.1016/j.annemergmed.2013.07.042. Image: http://echocardiographer.org/TTE.html
Category: Orthopedics
Keywords: Herpes Gladiatorum, skin rash, sports medicine (PubMed Search)
Posted: 3/9/2014 by Brian Corwell, MD
(Updated: 2/27/2026)
Click here to contact Brian Corwell, MD
Herpes Gladiatorum in Wrestlers
HSV causes non genital cutaneous infections primarily in wrestlers, commonly called herpes gladiatorum (HG)
Annual incidence in NCAA wrestlers is 20% to 40%
Most common cutaneous infection leading to lost practice time (40.5% of all infections)
Transmission is skin to skin.
Incubation period is 4 to 7 days from exposure. Healing usually occurs within 10 days after the initial lesion (without scaring).
Appearance: Numerous grouped uncomfortable (painful) vesicles/pustules on an erythematous base…evolve into moist ulcerations, followed by crusted plaques. Lesions typically get abraded during competition therefore may have an atypical appearance and may be mistaken for other infections such as staph. Distribution typically more diffuse than typical HSV infections. Occurs on body surfaces areas that typically come into contract with opponents (face, head, neck, ears, upper extremities). Lesion location typically on side of patient’s handedness. Recurrences occur at location of initial outbreak, a useful diagnostic aid.
Perform a thorough examination as ocular involvement was seen in 8% of high school wrestlers in one HG outbreak.
Typical treatment for primary infection is Valacyclovir 1g PO b.i.d. for 7 days. This is best started within 24h of symptom onset.
Cutaneous Infections in Wrestlers. Wilson et al., 2013. Sports Health.
Category: Pharmacology & Therapeutics
Keywords: aseptic meningitis,antibiotics,sulfamethoxazole,valacyclovir,antiepileptics,levetiracetam (PubMed Search)
Posted: 3/6/2014 by Ellen Lemkin, MD, PharmD
Click here to contact Ellen Lemkin, MD, PharmD
Aseptic meningitis is meningitis with negative bacterial cultures. Overall, viral infections are the most common etiology, however medications can also cause this illness.
Well known causes of aseptic meningitis include: antimicrobials (particularly sulfamethoxazole/trimethoprim), NSAIDS, antivirals (valacyclovir), and antiepileptics.
Recently an abstract was published that suggests that patients on levetiracetam have a higher risk of developing aseptic meningitis than those on topiramate and gabapentin. Lamotrigine has also been implicated, but appears to have a lower risk than levetiracetam, topiramate and gabapentin.
Teigland C, Chen P, Parente A, Bhattacharjee R. FDA Black Box Warning on Risk of Aseptic Meningitis with Use of Antiepileptic Drug Lamotrigine: Comparative Risk of Alternative Medications. Abstract, American Epilepsy Society. 2013
http://www.aesnet.org/go/publications/aes-abstracts/abstract-search/mode/display/st/parente/sy/2013/sb/Authors/id/1751398
Category: Critical Care
Posted: 3/4/2014 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Recruitment Maneuvers for ARDS
Keenan JC, et al. Lung recruitment in acute respiratory distress syndrome: what is the best strategy? Curr Opin Crit Care 2014; 20:63-8.
Category: Visual Diagnosis
Posted: 3/3/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
32 year-old male presents with the following. What's the diagnosis?

Answer: Hutchinson's Sign
Herpes zoster ophthalmicus (HZO)
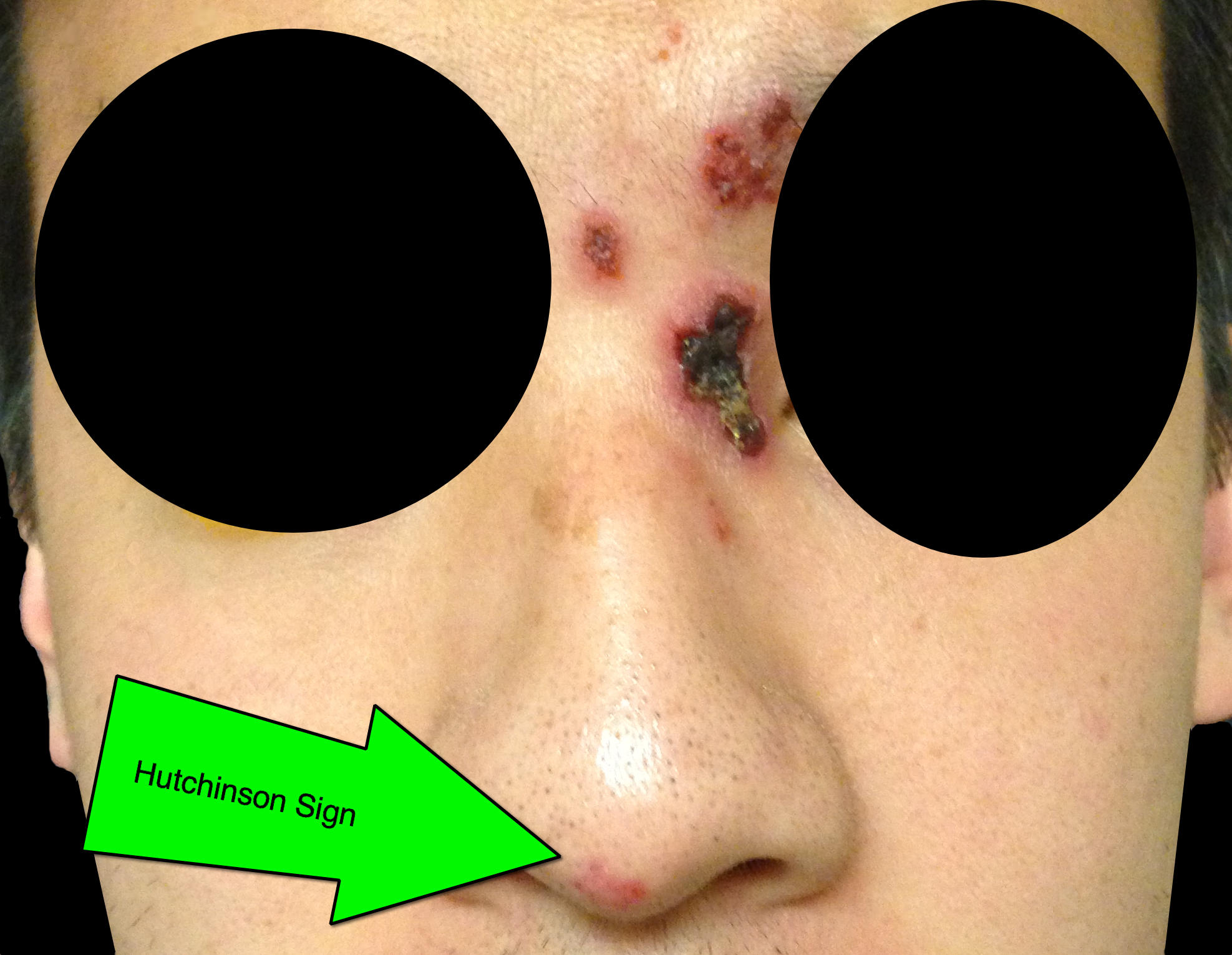
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: PEA (PubMed Search)
Posted: 2/27/2014 by Semhar Tewelde, MD
(Updated: 3/2/2014)
Click here to contact Semhar Tewelde, MD
Pulseless Electrical Activity (PEA)
ACLS algorithm for PEA focuses on memorizing the “ H's & T's" without a systematic approach on how to evaluate & treat the possible etiologies
A modified approach to PEA focuses on “cause-specific” interventions utilizing two simple tools: ECG and Bedside Ultrasound (US)
Simplified PEA Algorithm
♦1st obtain the ECG and assess the QRS-complex length (narrow vs. wide)
♦ A narrow QRS-complex suggests a mechanical problem: RV inflow or outflow obstruction
Utilize bedside US to assess for RV collapsibility vs. dilation
A collapsed RV suggests tamponade, tension PTX or mechanical hyperinflation
A dilated RV suggests PE
The above listed etiologies all have a preserved/hyperdynamic LV Tx begins w/aggressive IVF’s followed by “cause-specific” therapy: pericardiocentesis, needle decompression, forced expiration/vent management, and thrombolysis respectively
♦ A wide QRS-complex suggests a metabolic (hyperK/acidosis/toxins), ischemic, or LV problem
Utilize bedside US to assess for LV hypokinesis/akinesis
For metabolic/toxic etiologies treat w/calcium chloride and sodium bicarbonate +/- vasopressors
For ischemia and LV failure treat w/cardiac cath. vs. thrombolysis +/- vasopressors/inotropes
♦Trauma and several other etiologies of PEA that are seldom forgotten in any critically ill patient (hypothermia, hypoxia, and hypoglycemia) are not included in this algorithm.
Littmann L, Bustin D, Haley M. A Simplified and Structured Teaching Tool for the Evaluation and Management of Pulseless Electrical Activity. Med Princ Pract 2014; 23:1-6
Category: Pharmacology & Therapeutics
Keywords: epinephrine, cardiac arrest (PubMed Search)
Posted: 2/25/2014 by Bryan Hayes, PharmD
(Updated: 3/1/2014)
Click here to contact Bryan Hayes, PharmD
Background
The ACLS recommendation for epinephrine dosing in most cardiac arrest cases is 1 mg every 3-5 minutes. This dosing interval is largely based on expert opinion.
Primary Outcome
A new study reviewed 21,000 in-hospital cardiac arrest (IHCA) cases from the Get With the Guidelines-Resuscitation registry. The authors sought to examine the association between epinephrine dosing period and survival to hospital discharge in adults with an IHCA.
Methods
This pattern was consistent for both shockable and non-shockable cardiac arrest rhythms.
Warren SA, et al. Adrenaline (epinephrine) dosing period and survival after in-hospital cardiac arrest: A retrospective review of prospectively collected data. Resuscitation 2014;85(3):350-8. [PMID 24252225]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Toxicology
Keywords: hf, hydrofluoric acid (PubMed Search)
Posted: 2/27/2014 by Fermin Barrueto
(Updated: 2/27/2026)
Click here to contact Fermin Barrueto
Acid and Alkali burns are all known for their caustic cellular injury to local tissue. Acid burns and specifically hydrofluoric acid has systemic toxicity. HF can be lethal even if there is only a 5-10% total body surface area burn. You can find HF in brick cleaner, glass etching and wheel cleaner. They main metabolic derangement is hypocalcemia which can lead to cardiac dysrrhythmias and death.
Treatment has ranged from IV calcium or even intra-arterial calcium in the affected limb to treat the local severe pain associated with an HF burn. Checking a serum calcium to be sure IV calcium replacement is also necessary.
Remember HF -> severe pain, minimal tissue damage, hypocalcemia, hyokalemia, dysrrhythmias
Category: International EM
Keywords: Vaccine, disaster, international, (PubMed Search)
Posted: 2/26/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
Bottom Line:
University of Maryland Section of Global Emergency Health
Author: Veronica Pei
Use the CDC web module for travelers:
http://wwwnc.cdc.gov/travel/destinations/list
Category: Critical Care
Keywords: INTERACT 2, ATACH II, Intracranial Hemorrhage, Hypertensive Emergency, Hemodynamics (PubMed Search)
Posted: 2/24/2014 by John Greenwood, MD
(Updated: 2/25/2014)
Click here to contact John Greenwood, MD
Intensive BP Control in Spontaneous Intracranial Hemorrhage
Managing the patient with hypertensive emergency in the setting of spontaneous intracerebral hemorrhage (ICH) is often a challenge. Current guidelines from the American Stroke Association are to target an SBP of between 160 - 180 mm Hg with continuous or intermittent IV antihypertensives. Continuous infusions are recommended for patients with an initial SBP > 200 mm Hg.
An emerging concept is that rapid and aggressive BP control (target SBP of 140) may reduce hematoma formation, secondary edema, & improve outcomes.
Recently published, the INTERACT 2 trial (n=2,829) compared intensive BP control (target SBP < 140 within 1 hour) to standard therapy (target SBP < 180) found:
Study flaws: Patients treated with multiple drugs - combinations of urapadil, labetalol, nicardipine, nitrates, hydralazine, and diuretics. Management variability away from protocol seemed high. (Interesting editorial)
A Post-hoc analysis of the INTERACT 2 published just this month suggests that large fluctuations in SBP (>14 mmHg) during the first 24 hours may increase risk of death & major disability at 90 days.
Bottom Line: INTERACT 2 was a large RCT but not a great study (keep on the look out for ATACH II). However, in patients with spontaneous ICH, consider early initiation of an antihypertensive drip (preferably nicardipine) in the ED to reduce blood pressure fluctuations early with a target SBP of 140 mmHg.
Follow me on Twitter: @JohnGreenwoodMD
Category: Visual Diagnosis
Posted: 2/24/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
50 year-old with facial weakness and dysarthria. What's the diagnosis?
Stroke secondary to neurocysticercosis
Neurocysticercosis
Neurocysticercosis occurs secondary to ingestion of eggs from the Taenia solium tapeworm; ingestion typically occurs from ingestion of contaminated food.
Most patients are asymptomatic but symptoms of neurocysticercosis may include
Diagnosis is made via imaging such as CT scan; findings may vary depending on what stage of life the parasite is in (e.g., larvae); lumbar puncture should also be performed if the diagnosis is suspected.
Management should be symptomatic (e.g., seizures receive anticonvulsants) as well as eradication of the active parasites using steroids followed by albendazole (anti-parasitic drug)
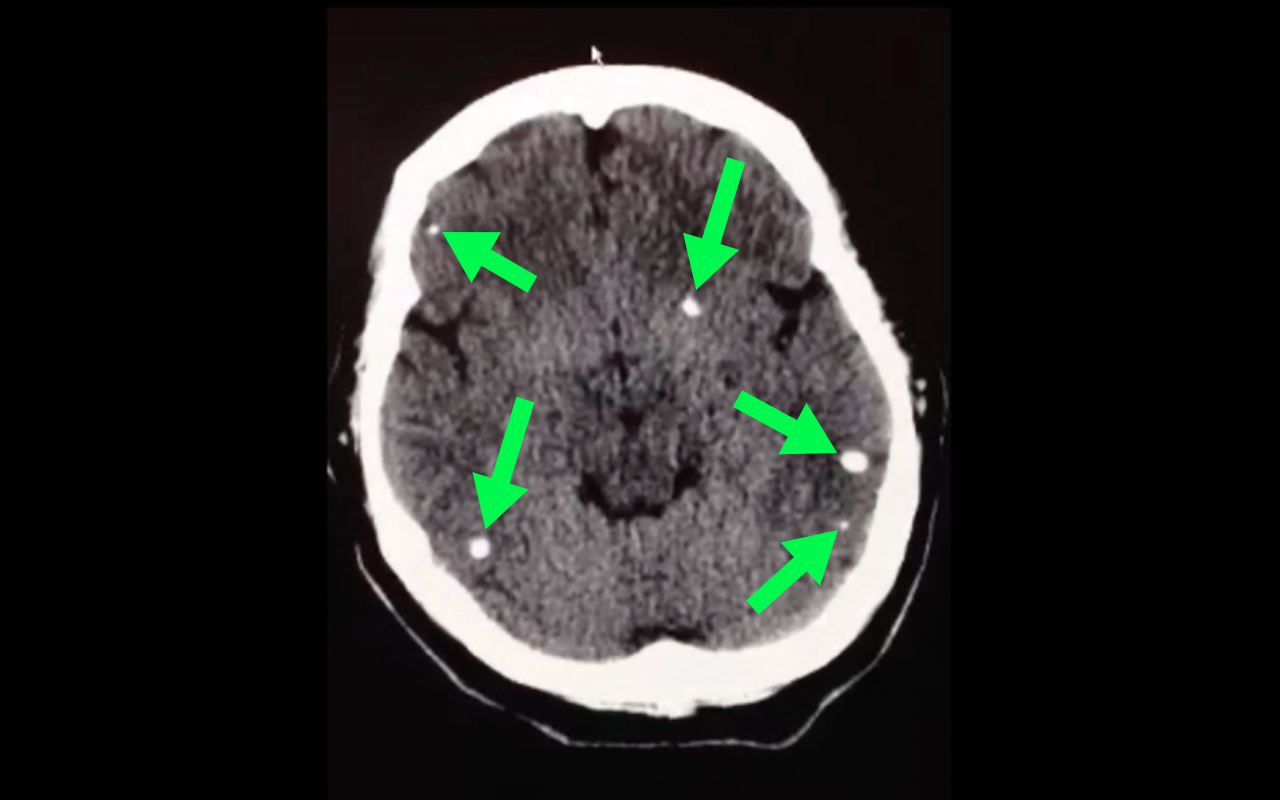
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Keywords: ACS, Stress Test (PubMed Search)
Posted: 2/23/2014 by Ali Farzad, MD
(Updated: 3/23/2014)
Click here to contact Ali Farzad, MD
1. Banerjee A, Newman DR, Van den Bruel A, Heneghan C. Diagnostic accuracy of exercise stress testing for coronary artery disease: a systematic review and meta-analysis of prospective studies. International Journal of Clinical Practice. 2012;66(5):477–492.
2. Walker J, Galuska M, Vega D. Coronary disease in emergency department chest pain patients with recent negative stress testing. West J Emerg Med. 2010;11(4):384–388.
3. Nerenberg RH, Shofer FS, Robey JL, Brown AM, Hollander JE. Impact of a negative prior stress test on emergency physician disposition decision in ED patients with chest pain syndromes. The American journal of emergency medicine. 2007;25(1):39–44.
Category: Orthopedics
Keywords: MRSA, arthocentesis (PubMed Search)
Posted: 2/22/2014 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The clinical examination is often unreliable in ruling out septic arthritis in the ED.
Diagnostic arthrocentesis is often performed.
Traditional teaching involved very high WBC count thresholds as part of diagnosis.
In one 2009 study, synovial leukocyte counts in cases of MRSA were often less than 25,000 cells/uL
Have a low threshold for empiric antibioitics even in the face of low WBC counts (and incredulous consultants)
How Common is MRSA in Adult Septic Arthritis? Frazee et al., 2009
Category: Pediatrics
Keywords: Passive leg raise, hypotension (PubMed Search)
Posted: 2/21/2014 by Jenny Guyther, MD
(Updated: 2/27/2026)
Click here to contact Jenny Guyther, MD
Passive leg raise (PLR) has been studied in adults as a bedside tool to predict volume responsiveness (see previous pearls from 5/7/13 and 6/17/2008). Can this be applied to children?
A single center prospective study looked at 40 intensive care patients ranging in age from 1 month to 12.5 years. They used a noninvasive monitoring system that could measure heart rate, stroke volume and cardiac output. These parameters were measured at a baseline, after PLR, after another baseline and after a 10 ml/kg bolus.
Overall, changes in the cardiac index varied with PLR. However, there was a statistically significant correlation in children over 5 years showing an increase in cardiac index with PLR and with a fluid bolus.
Bottom line: In children older then 5 years, PLR can be a quick bedside tool to assess for fluid responsiveness, especially if worried about fluid overload and in an under served area.
Lu et al. The Passive Leg Raise Test to Predict Fluid Responsiveness in Children - Preliminary Observations. Indian J Pediatr. Dec 2013. (epub ahead of print).
Category: International EM
Keywords: Cirrhosis, Hepatitis, International (PubMed Search)
Posted: 2/19/2014 by Andrea Tenner, MD
Click here to contact Andrea Tenner, MD
General Information:
Bottom Line:
Tenofovir has already become standard therapy for HIV (contained in Truvada and Atripla). This HBV study shows promise that this drug can not only decrease progression of disease but also reverse the cirrhosis associated with long-term infection. Given the prevalence of chronic HBV, larger scale role-out of this drug could markedly change the epidemiologic landscape of morbidity and mortality due to hepatitis B.
University of Maryland Section of Global Emergency Health
Author: Emilie J.B. Calvello
References: Marcellin P et al. Regression of cirrhosis during treatment with tenofovir disoproxil fumarate for chronic hepatitis B: A 5-year open-label follow-up study. Lancet 2012 Dec 10.
Category: Critical Care
Posted: 2/18/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Zimmerman, J.Cocaine intoxication. Crit Care Clinics 2012 Oct;28(4):517-26
Category: Visual Diagnosis
Posted: 2/17/2014 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
44 year-old construction worker fell off a ladder and presents with elbow pain. What's the diagnosis and what is the most commonly associated nerve injury?

Olecranon fracture; the ulnar nerve is most commonly injured
Pearls for Olecranon Fracture
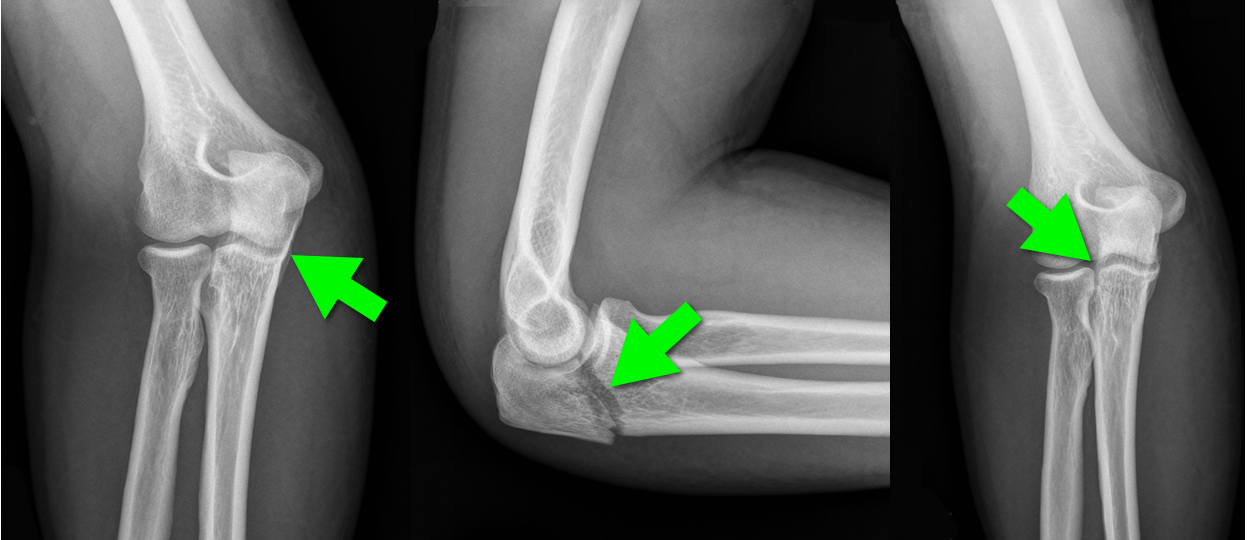
Follow me on Twitter (@criticalcarenow) or Google+ (+criticalcarenow)
Category: Cardiology
Posted: 2/16/2014 by Semhar Tewelde, MD
(Updated: 2/27/2026)
Click here to contact Semhar Tewelde, MD
Early Atherosclerosis Detection
50 middle-aged asymptomatic subjects free of vascular disease underwent carotid ultrasound (CUS) for risk stratification were also invited to undergo coronary computed tomography angiography (CCTA) or coronary artery calcium score (CAC) to identify which of the 3 imaging modalities was best at identification of early atherosclerosis
Atherosclerosis was observed in 28%, 78%, and 90% of subjects using CAC, CCTA, and CUS, respectively
36 patients with a CAC score = 0, 69% and 86% had atherosclerosis on CCTA and CUS, respectively
Concordance between modalities was highly variable
CUS and CCTA detection of plaque were significantly more sensitive than CAC
Considering the prevalence of subclinical disease on CUS and CCTA, the threshold at which to treat warrants further research
Schroeder B, Francis G, et al. Early Atherosclerosis Detection in Asymptomatic Patients: A Comparison of Carotid Ultrasound, Coronary Artery Calcium Score, and Coronary Computed Tomography Angiography. Canadian Journal of Cardiology, 2013-12-01, Volume 29, Issue 12, Pages 1687-1694
