Category: Pediatrics
Keywords: pediatric trauma, ultrasound, FAST (PubMed Search)
Posted: 7/1/2022 by Rachel Wiltjer, DO
(Updated: 2/8/2026)
Click here to contact Rachel Wiltjer, DO
Bottom line: A positive FAST warrants further workup and may be helpful in the hemodynamically unstable pediatric trauma patient, but a negative FAST does not exclude intraabdominal injury and evidence for performing FAST in hemodynamically stable pediatric patients is limited.
Guyther, J. Advances in Pediatric Abdominal Trauma: What’s New is Assessment and Management. Trauma Reports 2016; 17: 1-15.
Holmes JF, Kelley KM, Wootton-Gorges SL, Utter GH, Abramson LP, Rose JS, Tancredi DJ, Kuppermann N. Effect of Abdominal Ultrasound on Clinical Care, Outcomes, and Resource Use Among Children With Blunt Torso Trauma: A Randomized Clinical Trial. JAMA. 2017 Jun 13;317(22):2290-2296.
Category: Critical Care
Keywords: Insulin infusion, diabetes mellitus, diabetic ketoacidosis, DKA, subcutaneous, long-acting (PubMed Search)
Posted: 6/29/2022 by Kami Windsor, MD
(Updated: 9/21/2022)
Click here to contact Kami Windsor, MD
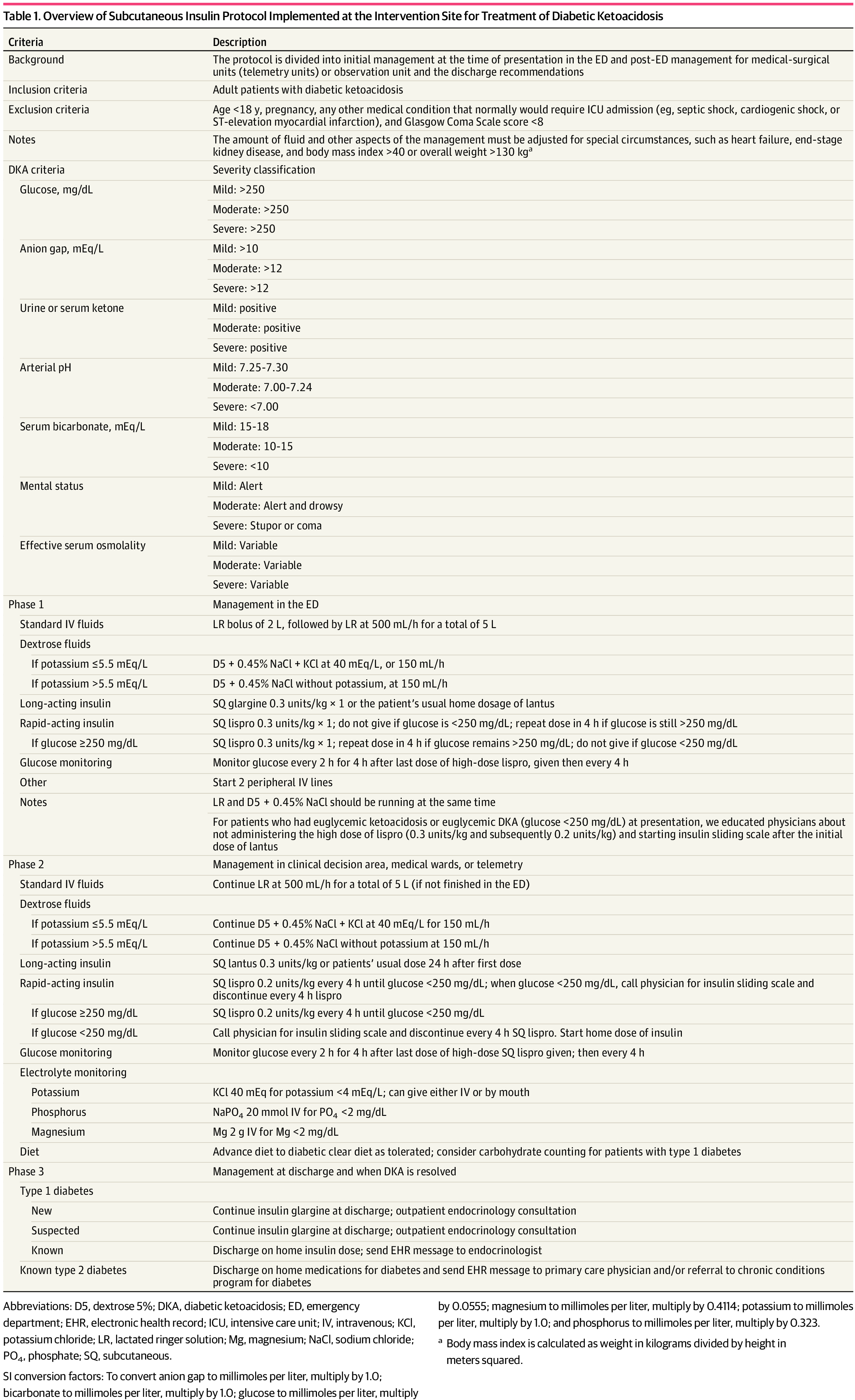
Background: It is classically taught that the tenets of DKA management are IV fluids, electrolyte repletion, and an insulin infusion that is titrated until approximately 2 hours after anion gap closure, when long-acting subcutaneous insulin is administered if the patient is tolerating oral intake. It has been previously found that earlier administration of subcutaneous long-acting insulin can shorten the time to anion gap closure, while other small studies have noted similar efficacy in subcutaneous insulin compared to IV in mild/moderate DKA.
A recent JAMA article presents a retrospective evaluation of a prospectively-implemented DKA protocol (see "Full In-Depth" section) utilizing weight-based subcutaneous glargine and lispro, rather than IV regular insulin, as part of initial and ongoing floor-level inpatient treatment.
When compared to the period before the DKA protocol:
The only exclusion criteria were age <18 years, pregnancy, and presence of other condition that required ICU admission.
Bottom Line: Not all DKA requires IV insulin infusion.
At the very least, we should probably be utilizing early appropriate-dose subcutaneous long-acting insulin. With ongoing ICU bed shortages and the importance of decreasing unnecessary resource use and hospital costs, perhaps we should also be incorporating subcutaneous insulin protocols in our hospitals as well.
As a part of the DKA protocol, patients:
Elevated BMI was not included in exclusion criteria, however the authors note that their DKA protocol has been amended to exclude patients >166kg due to concerns regarding insulin absorption.
Rao P, Jiang S, Kipnis P, et al. Evaluation of Outcomes Following Hospital-Wide Implementation of a Subcutaneous Insulin Protocol for Diabetic Ketoacidosis. JAMA Netw Open. 2022;5(4):e226417. doi:10.1001/jamanetworkopen.2022.6417
Houshyar J, Bahrami A, Aliasgarzadeh A. Effectiveness of Insulin Glargine on Recovery of Patients with Diabetic Ketoacidosis: A Randomized Controlled Trial. J Clin Diagn Res. 2015 May;9(5):OC01-5. doi: 10.7860/JCDR/2015/12005.5883.
Mohamed A, Ploetz J, Hamarshi MS. Evaluation of Early Administration of Insulin Glargine in the Acute Management of Diabetic Ketoacidosis. Curr Diabetes Rev. 2021;17(8):e030221191986. doi: 10.2174/1573399817666210303095633.
Karoli R, Fatima J, Salman T, Sandhu S, Shankar R. Managing diabetic ketoacidosis in non-intensive care unit setting: Role of insulin analogs. Indian J Pharmacol. 2011 Jul;43(4):398-401. doi: 10.4103/0253-7613.83109.
Ersöz HO, Ukinc K, Köse M, Erem C, Gunduz A, Hacihasanoglu AB, Karti SS. Subcutaneous lispro and intravenous regular insulin treatments are equally effective and safe for the treatment of mild and moderate diabetic ketoacidosis in adult patients. Int J Clin Pract. 2006 Apr;60(4):429-33. doi: 10.1111/j.1368-5031.2006.00786.x.
Category: Orthopedics
Keywords: Radial nerve compression, peripheral nerve injury, wrist drop (PubMed Search)
Posted: 6/25/2022 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
The radial nerve is susceptible to compressive neuropathy against the spiral grove of the humerus which can lead to neuropraxia.
When the upper arm is compressed against a chair back or bar edge sometimes from a lost battle with alcohol: Saturday night palsy.
When another individual sleeps on someone’s arm overnight compressing the radial nerve: Honeymoon palsy
From nerve compression from improper technique with crutches: Crutch palsy
If diagnosis not clear from history, DDx includes other entities that can also present with isolated wrist, thumb/finger drop
Horses: Radial verve palsy, CVA, C7 compression
Zebras: Lead toxicity, acute porphyrias (often polyneuropathy but upper extremity before lower and frequently distal extensors
Careful history and exam important in differentiating
In cases of peripheral compression against the spital groove the triceps maintains strength.
The distal extensors lose strength (wrist and fingers)
Including the thumb abduction (abductor pollicis longus is radial-innervated)
AND so will the brachioradialis
The brachioradialis (despite being a forearm flexor) has dual innervation from the radial nerve in 80% of people.
Brachioradialis strength is often preserved in a central lesion.
Best tested with arm supported on a surface in mid pronation/supination (hammer curl position) and have patient flex against resistance and evaluate muscle strength and bulk.
Category: Critical Care
Keywords: Vasopressors, Hypotension, Shock, Sepsis (PubMed Search)
Posted: 6/21/2022 by Mark Sutherland, MD
(Updated: 2/8/2026)
Click here to contact Mark Sutherland, MD
Although it is well-documented that there is no true "maximum" dose of vasopressor medications, further blood pressure support as doses escalate to very high levels tends to be limited. As such, debate has raged in Critical Care as to when is the "right" time to start a second vasoactive medication. The VASST trial (Russell et al, NEJM, 2008) is considered to be the landmark trial in this area, and found a trend towards improvement with early addition of vasopressin to norepinephrine, but no statistically significant difference, and may have been underpowered.
Partly as a result of VASST, the pendulum has tended to swing towards maximizing a single vasoactive before adding a second over the past decade. The relatively high cost of vasopressin in the US has also driven this for many institutions. However, more recently a "multi-modal" approach, emphasizing an earlier move to second, or even third, vasoactive medication, is increasingly popular. Although cost is often prohibitive for angiotensin-2 given controversial benefits, many now advocate for targeting adrenergic receptors (e.g. with norepinephrine or epinephrine), vasopressin receptors (e.g. with vasopressin or terlipressin) and the RAAS system (e.g. with angiotensin 2) simultaneously in patients with refractory shock. A recent review by Wieruszewski and Khanna in Critical Care (see references) outlines this approach well.
Bottom Line: When to add a second vasoactive medication (e.g. vasopressin) for patients with refractory shock after a first vasoactive is controversial and not known. Current practice is trending towards earlier addition of a second (or third) agent, especially if targeting different receptors, but there is limited high-quality evidence to support this approach. Many practicioners (including this author) still follow VASST and consider vasopressin once doses of around 5-15 micrograms/min (non-weight based) of norepinephrine are reached.
Wieruszewski PM, Khanna AK. Vasopressor Choice and Timing in Vasodilatory Shock. Crit Care. 2022 Mar 22;26(1):76. doi: 10.1186/s13054-022-03911-7. PMID: 35337346; PMCID: PMC8957156.
Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, Holmes CL, Mehta S, Granton JT, Storms MM, Cook DJ, Presneill JJ, Ayers D; VASST Investigators. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008 Feb 28;358(9):877-87. doi: 10.1056/NEJMoa067373. PMID: 18305265.
Early addition of Terlipressin: Article Title (ijccm.org)
Category: Pediatrics
Keywords: PNA, pediatrics, duration of treatment (PubMed Search)
Posted: 6/17/2022 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Williams DJ, Creech CB, Walter EB, Martin JM, Gerber JS, Newland JG, Howard L, Hofto ME, Staat MA, Oler RE, Tuyishimire B, Conrad TM, Lee MS, Ghazaryan V, Pettigrew MM, Fowler VG Jr, Chambers HF, Zaoutis TE, Evans S, Huskins WC; The DMID 14-0079 Study Team. Short- vs Standard-Course Outpatient Antibiotic Therapy for Community-Acquired Pneumonia in Children: The SCOUT-CAP Randomized Clinical Trial. JAMA Pediatr. 2022 Mar 1;176(3):253-261. doi: 10.1001/jamapediatrics.2021.
Category: Critical Care
Posted: 6/14/2022 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Vasopressor Tips in the Critically Ill
Legrand M, et al. Ten tips to optimize vasopressor use in the critically ill patient. Intensive Care Med. 2022; online ahead of print.
Category: Airway Management
Keywords: Concussion, risk, head impact (PubMed Search)
Posted: 6/11/2022 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Head Impact Exposure and Concussion Incidence
There has been a major focus on head impact biomechanics as a cause of single-impact concussion in football.
The role of repeated subclinical (without diagnosed concussion) head impact exposure (HIE)
during the preseason and regular season may also be contributory.
There may exist individualized concussion tolerance levels. This threshold may be reduced by the burden of sustained subconcussive impacts
NCAA Division 1 football athletes sustain a median of 426 impacts over the course of a football season
652 impacts/season in high school football
Total head impact exposure during the preseason occurred at 2x the rate of the regular season
This association was investigated over 1120 athlete seasons from 6 NCAA D1 football programs across 5 years
Head Impact Telemetry was used to record head impact exposure
Elevated preseason HIE was strongly associated with preseason and in season concussion incidence
Total season HIE was strongly associated with total season concussion incidence.
Conclusion: There is a prolonged effect of HIE on concussion risk starting with preseason football.
Athletes with higher preseason HIE may have higher risk of concussion for the entire fall season.
In Practice:
In 2016, the Ivy League eliminated full contact practices from the regular season in addition to their existing limits on the amount of full contact in practice during the spring and preseason.
Currently, the NCAA has the following limitations: Teams won’t be allowed to hold full-contact practices on more than two days in a row. Each practice session is limited to only 75 minutes of full contact, in addition to a limit of two preseason scrimmages.
Stemper BD, et al; CARE Consortium Investigators. Association between Preseason/Regular Season Head Impact Exposure and Concussion Incidence in NCAA Football. Med Sci Sports Exerc. 2022 Jun 1;54(6):912-922.
Category: Airway Management
Keywords: Hemorrhage, Pre-hospital, Trauma, Shock (PubMed Search)
Posted: 6/9/2022 by Lucas Sjeklocha, MD
Click here to contact Lucas Sjeklocha, MD
Enthusiasm for early transfusion of blood products in patients with traumatic shock has increased with increasing availability of pre-hospital blood and plasma and results of studies such as the PAMPer trial of pre-hospital plasma have shown potential mortality benefits. The deployment of prehospital blood for patients in hemorrhagic shock is promising but has significant cost and logistical considerations.
The RePHILL trial was a UK pre-hospital-based study of packed red blood cells and lyophilized plasma versus normal saline in trauma patients with presumed hemorrhagic shock. Patients older than age 16 with an SBP<90 or an absent radial pulse were eligible to get up to 1L of the study intervention. Multiple centers took part in the trial with 1:1 randomization stratified by study center. The primary outcome was a combination of mortality or lactate clearance less than 20% per hour or both.
A total of 432 patients were assigned a study fluid. The population was 82% male, median of 38 years old, with 78% of injuries classified as blunt, and 82% of the presumed hemorrhage classified at non-compressible. This was a very ill population with an average SBP of 73, an average GCS of 7 and an ISS of 36. The average from emergency call to EMS arrival was 30 minutes, average to study intervention was 26 minutes and time from EMS activation to ED arrival was 90 minutes.
The results showed no difference in the primary composite endpoint (64% vs 65%), with no difference in mortality (43% vs 45%) or lactate clearance (50% vs 55%). Interestingly, patients in the blood product arm had similar vital signs, lactate, and INR on ED arrival but received more blood products in the first 24 hours after ED arrival (pRBC 6.34 vs 4.41, p=0.004 and Plasma 5.04 vs 3.37, p=0.002). The was a trend toward improved early mortality at 3hr in the pre-hospital blood group (16% vs 22%, p=0.08).
Bottom Line(s):
Prehospital packed red blood cells and lyophilized plasma as compared to saline for traumatic shock did not improve mortality or lactate clearance in a well conducted multicenter RCT.
The use of prehospital blood products is promising but population which benefits, and the optimal type of product and delivery mechanism remain unclear.
Increased blood utilization and lower early mortality in the blood product group may represent alteration in the spectrum of disease that requires different early management.
The reasons for this counterintuitive result are unclear and further trials of whole blood as well as fibrinogen concentrates are ongoing.
Resuscitation with blood products in patients with trauma-related haemorrhagic shock receiving prehospital care (RePHILL): a multicentre, open-label, randomised, controlled, phase 3 trial. Crombie et al. Lancet Hematology. 2022.
https://doi.org/10.1016/ S2352-3026(22)00040-0
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
Click here to contact Michael Bond, MD
Small Bowel Obstruction
For more information on how to perform these exams and research data take a look at coreultrasound.com, thepocusatlas.com and ultrasoundgel.org.
Category: Critical Care
Keywords: low tidal volume, Emergency Department (PubMed Search)
Posted: 5/31/2022 by Quincy Tran, MD, PhD
Click here to contact Quincy Tran, MD, PhD
Background:
Lung-protective ventilation with low-tidal volume improves outcome among patients with Acute Respiratory Distress Syndrome. The use of low tidal volume ventilation in the Emergency Departments has been shown to provide early benefits for critically ill patients.
Methodology:
A systemic review and meta-analysis of studies comparing outcomes of patients receiving low tidal volume ventilation vs. those who did not receive low tidal volume ventilation.
The authors identified 11 studies with approximately 11000 patients. The studies were mostly observational studies and there was no randomized trials.
The authors included 10 studies in the analysis, after excluding a single study that suggested Non-low tidal volume ventilation was associated with higher mortality than low tidal volume ventilation (1).
Results:
Comparing to those with NON-Low tidal volume ventilation in ED, patients with Low-Tidal volume ventilation in ED were associated with:
Discussion:
Conclusion:
Although there was low quality of evidence for low tidal volume ventilation in the ED, Emergency clinicians should continue to consider this strategy.
1. Prekker ME, Donelan C, Ambur S, Driver BE, O'Brien-Lambert A, Hottinger DG, Adams AB. Adoption of low tidal volume ventilation in the emergency department: A quality improvement intervention. Am J Emerg Med. 2020 Apr;38(4):763-767. doi: 10.1016/j.ajem.2019.06.026. Epub 2019 Jun 15. PMID: 31235218.
2. De Monnin K, Terian E, Yaegar LH, Pappal RD, Mohr NM, Roberts BW, Kollef MH, Palmer CM, Ablordeppey E, Fuller BM. Low Tidal Volume Ventilation for Emergency Department Patients: A Systematic Review and Meta-Analysis on Practice Patterns and Clinical Impact. Crit Care Med. 2022 Jun 1;50(6):986-998. doi: 10.1097/CCM.0000000000005459. Epub 2022 Feb 7. PMID: 35120042.
Category: Orthopedics
Keywords: Boxer, reduction (PubMed Search)
Posted: 5/28/2022 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
28-year-old male present with dorsal hand pain after “losing his temper”
On exam, you note dorsal swelling, tenderness, and deformity
AP, lateral and oblique views are obtained.
There is no rotational deformity but using the lateral view, you note that there is angulation
Measured as the shaft of the metacarpal as compared to the mid-point of the fracture fragment
Acceptable shaft angulation generally accepted to be less than 40°
Patient has greater that acceptable angulation so you have to perform closed reduction
After appropriate pain control consider the “90-90 method.”
Flex the MCP, DIP, and PIP joints to 90 degrees.
This positioning stretches the MCP collateral ligaments helping to optimize reduction
Next, apply volar pressure over the dorsal aspect of the fracture site while applying pressure axially to the flexed PIP joint.
Best demonstrated below
https://www.youtube.com/watch?v=40irKoUJqsM
Category: Critical Care
Posted: 5/24/2022 by Caleb Chan, MD
Click here to contact Caleb Chan, MD
-If the patient is able to maintain mentation/airway/SpO2/hemodynamics and cough up blood, intubation is not immediately necessary
-If you do intubate, intubate with the largest ETT possibly to faciliate bronchoscopic interventions and clearance of blood
-The CT scan that typically needs to be ordered is a CTA (not CTPA) with IV con
-See if you can find prior/recent imaging in the immediate setting (e.g. pre-existing mass/cavitation on R/L/upper/lower lobes)
-Get these meds ready before the bronchoscopist gets to the bedside to expedite care:
-If the pt's vent suddenly has new high peak pressures or decreased volumes after placement of endobronchial blocker, be concerned that the blocker has migrated
Charya AV, Holden VK, Pickering EM. Management of life-threatening hemoptysis in the ICU. J Thorac Dis. 2021;13(8):5139-5158.
Category: Critical Care
Posted: 5/23/2022 by William Teeter, MD
(Updated: 2/8/2026)
Click here to contact William Teeter, MD
Encountered a situation in CCRU where we needed to prepare for a patient exsanguinating from gastric varices, and found a great summary of the different types of gastroesophageal balloons from EMRAP.
Summary: https://www.youtube.com/watch?v=Yv4muh0hX7Y
More in depth video on the Minnesota tube: https://www.youtube.com/watch?v=4FHIiA_doWU
Nice review article: https://www.sciencedirect.com/science/article/abs/pii/S0736467921009136
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
Click here to contact Michael Bond, MD
Aortic Dissection
Ultrasound has a great specificity for aortic dissection. Remember to take a look at your aorta on all cardiac views.
Let’s give a shout out to Nikki Cali for diagnosing aortic dissection in a patient with a recent PE. Can you find the dissection flap in this image?
For more information on how to perform these exams and research data take a look at coreultrasound.com, thepocusatlas.com and ultrasoundgel.org.
Category: Pediatrics
Keywords: motrin, narcotics, oxycodone, fracture care (PubMed Search)
Posted: 5/20/2022 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Ali et al. An observational cohort study comparing ibuprofen and oxycodone in children with fractures. PLos ONE 16(9): e0257021.
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
Click here to contact Michael Bond, MD
Peritonsillar Abscess
For more information on how to perform these exams and research data take a look at coreultrasound.com, thepocusatlas.com and ultrasoundgel.org.
Category: Orthopedics
Keywords: Varus, knee (PubMed Search)
Posted: 5/15/2022 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
4-year-old patient comes to the ED for an unrelated complaint and you notice that his knees appear to be touching while his ankles remain apart.
Genu Varum or “knock knees” may be caused by Infantile Blount’s disease
-A progressive pathologic condition causing genu varum in children between ages 2 to 5
- Centered at the tibia
-Bilateral in up to 80%
-More common in boys
-Leg length discrepancy
- Articular incongruity
Risk factors: Early walkers (<1 year), overweight, large stature, Hispanic and African American
Results in disruption of normal cartilage growth at the MEDIAL aspect of the proximal tibia while LATERAL growth continues normally
May complain of knee soreness or subjective instability
On physical exam
Focal angulation of the proximal tibia
Lateral thrust during stance phase of walking (brief lateral shift of proximal fibula and tibia)
No tenderness or effusion
Imaging: Plain film shows varus deformity of the proximal tibia with medial beaking (beak like appears of bone) and downward slope of the proximal tibia metaphysis (increased metaphyseal-diaphyseal angle)
https://paleyinstitute.org/wp-content/uploads/blounts1.jpg
Treatment depends upon the age of the child and the severity
Successful in up to 80%
Note: In adolescent variant bracing is ineffective and surgery is only treatment
: Genu varum is normal in children <2 years old and becomes neutral at 14 months
DDX: Physiologic varus, Rickets
Category: Visual Diagnosis
Posted: 5/11/2022 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Appendicitis
Ultrasound has a reported high specificity (97.9) for acute appendicitis in moderate to high pre-test probability of patients.
Let’s give a shout out to Reed Macy, who diagnosed appendicitis in a male with vomiting and abdominal pain!
Category: Pharmacology & Therapeutics
Keywords: Droperidol, QTc (PubMed Search)
Posted: 5/7/2022 by Wesley Oliver
Click here to contact Wesley Oliver
A recent prospective cohort study investigated the effect of low-dose droperidol on QTc in an emergency department:
Low-dose droperidol has a small effect on QTc and most patients remained below 500 ms.
Hernández-Rodríguez L, Bellolio F, Cabrera D, et al. Prospective real-time evaluation of the QTc interval variation after low-dose droperidol among emergency department patients. Am J Emerg Med. 2022 Feb;52:212-219.
Category: Pediatrics
Keywords: autism spectrum disorder, neurodevelopmental disorder (PubMed Search)
Posted: 5/6/2022 by Rachel Wiltjer, DO
(Updated: 2/8/2026)
Click here to contact Rachel Wiltjer, DO
