Category: Toxicology
Keywords: mortality, predictors, MALA, pH, lactate (PubMed Search)
Posted: 2/12/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Metformin associated lactic acidosis (MALA) has a high rate of mortality, ranging from 25% to 50%. Lactate level and acidemia are frequently associated with poor clinical outcome in many disease/medical conditions (e.g. sepsis).
A study investigated, via meta-analysis, if lactate level and pH were predictive of mortality in MALA.
Results
44 studies were identified from PubMed, EMBASE and Web of Science.
170 cases of MALA were included
pH and lactate were poor predictors of mortality based upon ROC curve
Conclusion
Category: Neurology
Keywords: spinal cord injury, cauda equina, urinary retention, incontinence (PubMed Search)
Posted: 2/12/2020 by WanTsu Wendy Chang, MD
Click here to contact WanTsu Wendy Chang, MD
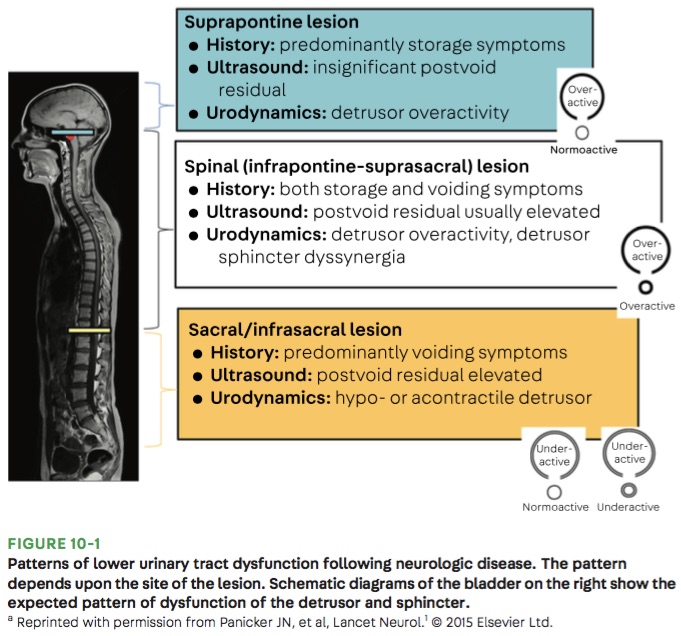
Bottom Line: Urinary retention can be seen with neurological injury involving the lower brainstem, spinal cord, cauda equina, and peripheral nerves.
Panicker JN, Sakakibara R. Lower urinary tract and bowel dysfunction in neurologic disease. Continuum (Minneap Minn). 2020;26(1):178-199.
Follow me on Twitter @EM_NCC
Category: Critical Care
Keywords: cerebral fat embolism, trauma, long bone fracture (PubMed Search)
Posted: 2/10/2020 by Mark Sutherland, MD
(Updated: 2/7/2026)
Click here to contact Mark Sutherland, MD
Don't forget cerebral fat embolism syndrome (FES) on the differential for altered trauma patients. FES is typically associated with long bone fractures, but has been reported with other fractures, orthopedic reaming (i.e. aggressive orthopedic procedures), and in rare cases even with non-fracture (soft-tissue) trauma. Typically symptoms occur between 24 and 72 hours after injury, but there have been cases both earlier and later. Diagnosis is clinical, but MRI may be helpful, and will often show multiple cerebral white matter lesions. It is debated whether FES is truly an embolic phenomena (i.e fat molecules traveling to and blocking blood supply of organs), or rather an inflammatory response to free fatty acids in the blood stream (i.e. more of a vasculitis type pathology). Management is supportive care, but give these patients time as there can be favorable outcomes, even after prolonged coma.
Morales-vidal SG. Neurologic Complications of Fat Embolism Syndrome. Curr Neurol Neurosci Rep. 2019;19(3):14.
From the diagnosis to the therapeutic management: cerebral fat embolism, a clinical challenge
https://www-ncbi-nlm-nih-gov.proxy-hs.researchport.umd.edu/pmc/articles/PMC6324602/
Category: Orthopedics
Keywords: Back pain (PubMed Search)
Posted: 2/8/2020 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Taking an accurate history to diagnose Cauda Equina Syndrome (CES)
Classic teaching is to inquire specifically about bowel and bladder function, sexual dysfunction, and/or loss of sensation in the groin.
Rather than asking about urinary incontinence, clinicians should ask specifically about difficulty passing urine, new leakage and retention.
Discussing issues related to sexual dysfunction are difficult for both clinicians and patients.
Rather than asking if there are any issues with sexual function, a more direct and informative way would be to ask if the patient has a “change in ability to achieve an erection or ejaculate” or “loss of sensation in genitals during sexual intercourse.”
Saddle anesthesia has the highest predictive value in diagnosing MRI-proven CES. Loss of sensation may be incomplete and patchy. Ask about change in sensation with wiping after a bowel movement.
Greenhalgh S, Truman C, Webster V, Selfe J. Development of a toolkit for early identification of cauda equina syndrome. Prim Health Care Res Dev. 2016;17(6):559-567.
Category: Pulmonary
Keywords: CAP, Pneumonia (PubMed Search)
Posted: 2/1/2020 by Ashley Martinelli
(Updated: 2/7/2026)
Click here to contact Ashley Martinelli
The new IDSA and American Thoracic Society guidelines for community acquired pneumonia were recently released. Major updates to the guidelines include but are not limited to:
1. It is not recommended to obtain sputum cultures in routine care. Consider only in patients who are intubated or empirically being treated for hospital associated pathogens such as MRSA or P. aeruginosa.
2. Blood cultures are only recommended for severe CAP managed in the hospital or those empirically being treated for MRSA or P. aeruginosa, or prior infection with those pathogens, or hospitalized and received parenteral antibiotics in the last 90 days.
3. Test for influenza during time periods when influenza is prominent (as in our current 2020 influenza outbreak).
4. Healthy patients can receive either amoxicillin 1g TID, doxycycline 100mg BID, or azithromycin 500mg followed by 250mg daily x 4 doses.
5. Patients with comorbidities such as chronic heart, lung, liver, or renal disease, diabetes, alcoholism, malignancy, or asplenia should receive combination therapy with a beta-lactam (amoxicillin/clavulanate, cefdinir, or cefpodoxime) + azithromycin or doxycycline. If allergies preclude the use of a beta-lactam, a fluoroquinolone (levofloxacin or moxifloxacin) can be used.
6. Patient admitted for non-severe CAP can receive combination beta-lactam (ampicillin/sulbactam, or ceftriaxone) and azithromycin therapy. Patients with severe beta-lactam allergies can receive either levofloxacin or moxifloxacin).
7. It is no longer recommended to add anaerobic coverage for suspected aspiration pneumonia unless the patient is suspected to have a lung abscess or empyema. It is most likely a chemical pneumonitis and should resolve within 24-48 hours with supportive therapy.
Metlay JP, Waterer GW, Long AC, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Resp Crit Care. 2019;200(7):e45-e67.
Category: Critical Care
Keywords: Encephalitis, autoimmune, psychosis, movement disorders (PubMed Search)
Posted: 1/24/2020 by Robert Brown, MD
(Updated: 2/7/2026)
Click here to contact Robert Brown, MD
Dr. Bryan Hayes wrote a Pearl 10/4/2013 to remind us autoimmune encephalitis can present like neuroleptic malignant syndrome.
Dr. Danya Khouja wrote a Pearl 6/28/2017 to inform us autoimmune encephalitis is associated with tumors and can be investigated with serum and CSF antibody panels.
Since those publications, the number of validated autoimmune biomarkers in these panels has increased dramatically. In 2020 we now know, autoimmune encephalitis is at least as common as infectious encephalitis.
Here is how to diagnose it
1. Suspect the diagnosis in patients with subacute/rapidly progressive altered mental status, memory loss, or psychiatric symptoms. It can be mistaken for a new diagnosis of schizophrenia or bipolar disorder.
2. Look for one or more additional findings: new seizures, focal CNS findings, CSF pleocytosis, MRI findings
3. Exclude other likely etiologies (but try not to get hung up on a positive drug test, especially if drug use was not recent).
Why is this important?
Early treatment with steroids and plasmapheresis can prevent progression of disease (prevent seizures, prevent months-long hospitalizations).
Young girls are especially likely to have teratomas as a cause for the disease. Finding and resecting those tumors is life-saving.
Titulaer M, McCracken L, Gabilondo I, et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: An observational cohort study. The Lancet Neurology 2013; 12(2):157-165.
Dubey D, Pittock S, Kelly C, et al. Autoimmune Encephalitis Epidemiology and a Comparison to Infectious Encephalitis. Annals of Neurology 2018;83:166-177
Guasp M, Modena Y, Armangue T, et al. Clinical features of seronegative, but CSF antibody-positive, anti-NMDA receptor encephalitis. Neurology: Neuroimmunology and Neuroinflammation 2020; 7(2):e659-664.
Category: Orthopedics
Keywords: Concussion, (PubMed Search)
Posted: 1/25/2020 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Timeliness of Concussion Referral
Do patients with a self-limited diagnosis of “concussion” require specialty follow up?
If so, is there a benefit to earlier evaluation?
Recently published research from the University of Pittsburgh Sports Medicine Concussion Program suggests so.
Subjects: 162 concussed athletes between the ages of 12 and 22
Findings: Athletes treated in the first week after injury recovered faster than those who did not receive care until 8 to 21 days post injury.
Note: Once in care the length of time spent recovering was the same for both groups. This suggests that the amount of time prior to the initiation of care may explain the longer recovery time of the 2nd group.
Earlier recovery can help minimize effects on mood, quality of life and lost time in school/work.
Take home: Consiuder early follow up referral to a qualified provider for all concussed patients seen in the ED
Kontos et al., 2020. Association of Time Since Injury to the First Clinic Visit With Recovery Following Concussion. Jama Neurology.
Kontos et al., 2020. Association of Time Since Injury to the First Clinic Visit With Recovery Following Concussion. Jama Neurology.
Category: Toxicology
Keywords: risk of death, intentional drug overdose (PubMed Search)
Posted: 1/23/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Intentional drug overdose (IDO) can lead to significant morbidity and can increased patient's risk of death. A study was recently performed to identify the predictors of death in a cohort of patient who intentionally overdose on drug(s).
National Self-Harm Registry and National Drug-Related Death Index were reviewed (between January 1st, 2007 and December 31st, 2014) to identify the study cohort.
Results
|
| Non fatal IDO | Fatal IDO |
| Number of cases | 63,831 | 364 |
| Incidence | 148.8/100,000 | 1.01/100,000 |
| Male | 42.0% | 55.2% |
| Age, years (median) | 35 | 44 |
| Multiple drug ingestion | 48.5% | 78.3% |
Risk of death
Conclusion
International Journal of Drug Policy76https://doi.org/10.
Category: Critical Care
Posted: 1/21/2020 by Mike Winters, MBA, MD
Click here to contact Mike Winters, MBA, MD
Mechanical Ventilation Pearls for Acute Ischemic Stroke
Robba C, et al. Mechanical ventilation in patients with acute ischemic stroke: from pathophysiology to clinical practice. Crit Care. 2019;23:388.
Category: Pediatrics
Keywords: ENT, post tonsillectomy bleeding, T and A (PubMed Search)
Posted: 1/17/2020 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Tonsillectomy and adenoidectomy (T&A) is the second most common ambulatory surgery performed in the US. Children younger than 3 years, children with craniofacial disorders or sleep apnea are typically admitted overnight as studies have shown an increase rate of airway or respiratory complications in this population.
The most common late complications include bleeding and dehydration. Other complications include nausea, respiratory issues and pain.
Post-operatively, the overall 30-day emergency department return rate is up to 13.3%. Children ages 2 and younger were more likely to present to the ED. There is significantly higher risk of dehydration for children under 4 years. Children over the age of 6 had significantly higher bleeding risk and need for reoperation for hemorrhage control.
Lindquist NR, Feng Z and Mukerji SS. Age-related causes of emergency department visits after pediatric adenotonsillectomy at a tertiary pediatric referral center. International Journal of Pediatric Otorhinolaryngology 2019; 127: 109668.
Category: Toxicology
Keywords: non-fatal opioid overdose, risk of fatality (PubMed Search)
Posted: 1/16/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Many patients are treated in the emergency room for non-fatal opioid overdose. However, it is unknown what proportion of these patient population experience subsequent fatality after their ED visit.
A recent study investigated the 1-year mortality rate among Massachusetts ED patients who were treated and discharged from ED for non-fatal opioid overdose.
Results
Of those who died,
Manner of death
Place of death
Conclusion
Weiner SG et al. One-year mortality of patients after emergency department treatment for nonfatal opioid overdose. Ann Emerg Med 2020 https://doi.org/10.1016/j.annemergmed.2019.04.020
Category: Critical Care
Keywords: Vitamin D, critically ill (PubMed Search)
Posted: 1/14/2020 by Quincy Tran, MD, PhD
(Updated: 2/7/2026)
Click here to contact Quincy Tran, MD, PhD
Settings: multicenter, double-blind, phase 3 trial (apparently vitamin D worked in phase 2 trials).
Study Results:
Discussion:
Conclusion:
Early administration of high dose vitamin D did not improve 90-day all cause mortality.
Early High-Dose Vitamin D3 for Critically Ill, Vitamin D-Deficient Patients.
National Heart, Lung, and Blood Institute PETAL Clinical Trials Network, Ginde AA, Brower RG, Caterino JM, Finck L, Banner-Goodspeed VM, Grissom CK, Hayden D, Hough CL, Hyzy RC, Khan A, Levitt JE, Park PK, Ringwood N, Rivers EP, Self WH, Shapiro NI, Thompson BT, Yealy DM, Talmor D. N Engl J Med. 2019 Dec 26;381(26):2529-2540.
Category: Airway Management
Keywords: back pain, urinary retention, CES (PubMed Search)
Posted: 1/11/2020 by Brian Corwell, MD
(Updated: 2/7/2026)
Click here to contact Brian Corwell, MD
Known effects and side effects of prescribed medicines may masquerade as cauda equina syndrome (CES) .
Analgesic medicines used by patients with chronic back pain may also cloud the diagnosis of CES.
Cholinergic medications (glaucoma/myasthenia) may lead to voiding issues.
Anticholinergic medications (COPD/urinary incontinence) may lead to urinary retention.
Opioids – Constipation, reduced bladder sensation
Anticonvulsants (Gabapentin/Pregabalin)- Urinary incontinence
Antidepressants (Amitriptyline) – Urinary retention, sexual dysfunction, reduced awareness of need to pass urine
NSAIDs – Urinary retention.
Verhamme KM, et al. Nonsteroidal anti-inflammatory drugs and increased risk of acute urinary retention. Arch Intern Med. 2005:165;1547-1551.
Category: Airway Management
Keywords: Adrenal Crisis (PubMed Search)
Posted: 1/7/2020 by Caleb Chan, MD
(Updated: 2/7/2026)
Click here to contact Caleb Chan, MD
Adequate treatment of adrenal crisis (AC) is often delayed, even when a h/o adrenal insufficiency is known.
Besides refractory hypotension, also consider in pts with:
Beware of triggers:
Treatment:
Amrein K, Martucci G, Hahner S. Understanding adrenal crisis. Intensive Care Med. 2018;44(5):652-655.
Rushworth RL, Torpy DJ, Falhammar H. Adrenal Crisis. N Engl J Med. 2019;381(9):852-861.
Category: Pharmacology & Therapeutics
Keywords: Influenza, Pneumonia, MRSA, Antibiotics (PubMed Search)
Posted: 1/4/2020 by Wesley Oliver
Click here to contact Wesley Oliver
Influenza is a common cause of community-acquired pneumonia and invasive bacterial coinfection may occur. In addition, secondary bacterial pneumonia due to MRSA is becoming more prevalent. Due to the higher incidence of MRSA, it is recommended that antibiotics with activity against MRSA (vancomycin or linezolid) be included in the empiric treatment regimen, especially if the patient is critically ill.
Take Home Point: Don’t forget to add MRSA coverage to your empiric treatment regimen in those influenza patients with severe disease or secondary bacterial pneumonia.
1. Uyeki, Timothy M et al. Clinical Practice Guidelines by the Infectious Diseases Society of America: 2018 Update on Diagnosis, Treatment, Chemoprophylaxis, and Institutional Outbreak Management of Seasonal Influenzaa. Clin Infect Dis. 2019;68: e1-e47.
2. Metlay JP, Waterer GW, Long AC, Anzueto A, Brozek J, Crothers K, et al. Diagnosis and treatment of adults with community-acquired pneumonia. An official clinical practice guideline of the American Thoracic Society and Infectious Diseases Society of America. Am J Respir Crit Care Med. 2019;200:e45–e67.
Category: Toxicology
Keywords: acetaminophen, pharmcobezoar (PubMed Search)
Posted: 1/2/2020 by Hong Kim, MD
Click here to contact Hong Kim, MD
Pharmacobezoars (clumps of medication/pills) formation has been demonstrated in few medications such as aspirin, and ferrous sulfate tablets. Their presence can alter management due to prolonged absorption and may cause GI obstruction.
Acetaminophen (APAP) is a commonly available over-the-counter medication that is often implicated in an acute overdose event. A recently published in-vitro study (using pig stomach) investigated whether APAP can form a pharmacobezoar.
APAP group/dosage
Positive control group
Negative control group
Results
Conclusion
Li YK et al. In vitro study of pharmacobezoar formation in simulated acetaminophen overdose. Clin Toxicol (Phila) 2019. https://doi.org/10.1080/15563650.2019.1705971
Category: Critical Care
Keywords: pregnancy, peripartum, antepartum, fetal (PubMed Search)
Posted: 12/31/2019 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
The arrival of a critically ill pregnant patient to the ED can be anxiety-provoking for emergency physicians as two lives and outcomes must be considered.
Some basic tenets of care, regardless of underlying issue, include:
Finally, once critical illness is identified the OB and NICU teams should be consulted immediately. Fetal distress in a viable pregnancy may be an indication for delivery, and initiation of the transfer process should occur if the supportive specialties are not in-house.
Gaffney A. Critical care in pregnancy: Is it different? Semin Perinatol 2014;38(6):329-40.
Pacheco LD, Saade GR, Hankins GDV. Mechanical ventilation during pregnancy: Sedation, analgesia, and paralysis. Clin Obstet Gynecol 2014;57(4):844-50.
Practice Guidelines of Obstetric Anesthesia: An updated report by the American Society of Anesthesiologists Task Force on Obstetric Anesthesia and the Society for Obstetric Anesthesia and Perinatology. Anesthesiology 2016;124(2):270-300.
Guntupalli KK, Hall N, Karnad D, et al. Critical illness in pregnancy. Chest 2015;148(4):1093-1104.
Category: Toxicology
Keywords: gabapentin, misuse (PubMed Search)
Posted: 12/26/2019 by Hong Kim, MD
Click here to contact Hong Kim, MD
Non-opioid medications such as gabapentin are frequently prescribed for the management of pain.
A retrospective study of the National Poison Data System (data collected by the U.S. Poison Centers) from 2013 – 2017 showed increasing trend of gabapentin exposure.
Gabapentin exposure increased between 2013 and 2017 by:
5 most commonly co-ingested substances with gabapentin
16.7% of the isolated gabapentin exposure required hospitalization.
Conclusion:
Category: Airway Management
Keywords: HLH, Hemophagocytic Lymphohistiocytosis (PubMed Search)
Posted: 12/24/2019 by Kim Boswell, MD
Click here to contact Kim Boswell, MD
Hemophagocytic Lymphohistiocytosis (HLH) – Part I
A rare, but important disease that is becoming more widely recognized and more frequently diagnosed. This disease, while uncommon, is rapidly progressive and caries a high mortality rate.
Causes are not completely understood, but involve abnormal activation of the immune response due to a failure of the typical downregulation in hyperinflammatory processes.
Two types exist:
Congenital/Familial – genetic predisposition which usually requires a triggering event to occur
Acquired – occurs in adults with no known predisposition (often have underlying genetic predispositions) – triggering events include infections , immunodeficiency, rheumatologic disorders, and malignancy in addition to many others.
Diagnosis is challenging due to the wide variety of symptoms and constellation of symptoms, which often mimic more common infections/sepsis presentations. Common symptoms include the following:
Symptoms can, and do, occur in any body system – rashes, conjunctivitis, DIC, LFT abnormalities, hypotension/shock, and respiratory failure are all common concomitant findings in the presentation of HLH
More on the specific diagnosis and treatment to follow in part II...
McClain KL. Clinical features and diagnosis of hemophagoctyic lymphohistiocytosis. UpToDate.Waltham, MA:UpToDate Inc. https://www.uptodate.com (Accessed on December 24, 2019.)
Category: Pediatrics
Keywords: Urinary retention, formulas (PubMed Search)
Posted: 12/20/2019 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Urinary retention in pediatrics is defined as the inability to void for more than 12 hours in the presence of a palpable bladder or a urine volume greater than expected for age.
Maximum urine volume calculation for age: (age in years + 2) x 30ml.
Causes of urinary retention include mechanical obstruction, infection, fecal impaction, neurological disorders, gynecological disorders and behavioral problems.
The distribution is bimodal occurring between 3 and 5 years and 10 to 13 years.
Nevo A, Mano R, Livne P, Sivan B and Ben-Meir. Urinary Retention in Children. Urology 2014; 84(6):1475-1479.
