Category: Toxicology
Keywords: amlodipine, non-dihydropyridines, high-dose insulin (PubMed Search)
Posted: 6/1/2023 by Hong Kim, MD
(Updated: 2/7/2026)
Click here to contact Hong Kim, MD
Calcium channel blocker (CCB) overdose can lead to severe shock/hypotension. A small study was conducted to compare the hemodynamic effects of high-dose insulin (HDI) for two classes of CCB (dihydropyridines vs. non-dihydropyridines) that work differently to manage hypertension.
Study design:
Study sample:
Result
Median number of maximum concomitant vasopressors (p=0.04)
Median difference in max concomitant vasopressors: 1 (95% CI: 0 – 2)
Median max epinephrine dosing
Use of rescue methylene blue (p=0.009)
Conclusion:
Cole JB, Lee SC, Prekker ME, Kunzler NM, Considine KA, Driver BE, Puskarich MA, Olives TD. Vasodilation in patients with calcium channel blocker poisoning treated with high-dose insulin: a comparison of amlodipine versus non-dihydropyridines. Clin Toxicol (Phila). 2022 Nov;60(11):1205-1213. doi: 10.1080/15563650.2022.2131565. Epub 2022 Oct 25. PMID: 36282196.
Category: Trauma
Keywords: pain control, fentanyl, oral medication, trauma (PubMed Search)
Posted: 5/31/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
A study looking at 177 trauma patients (predominately skiing injuries) treated with oral trans mucosal fentanyl (600 and 800 mcg dosing) found a statistically and clinically significant reduction in pain. This therapy could be an adjunct to patients who require pain relief but IV access is delayed for various reasons.
Pietsch, U., Fischer, H., Rüst, C.A. et al. Oral transmucosal fentanyl citrate analgesia in prehospital trauma care: an observational cohort study. Scand J Trauma Resusc Emerg Med 31, 2 (2023). https://doi.org/10.1186/s13049-023-01066-0
Category: Critical Care
Keywords: thrombocytopenia, bleeding, hemorrhage, platelets, transfusions, central lines, CVCs (PubMed Search)
Posted: 5/30/2023 by Kami Windsor, MD
Click here to contact Kami Windsor, MD
Background: In general practice, platelets are typically transfused for invasive procedures when the platelet count falls below 50 x 109/L. Regarding the placement of central venous catheters (CVCs), there is minimal data to support or refute decisions to transfuse platelets in these patients, although the 2015 Clinical Practice Guideline from the AABB (formerly, the American Association of Blood Banks) recommends deferring platelet transfusion until a platelet count of 20 x 109/L for CVC placement [weak recommendation, low quality evidence].1
In a study published this month in NEJM,2 van Baarle et al. performed a multicenter randomized controlled noninferiority trial comparing platelet transfusion to no transfusion in patients with platelets 10 to 50 x 109/L prior to US-guided CVC insertion. The primary outcome was the occurrence of catheter-related bleeding Grades 2-4 (Grade 1 = oozing; managed with <20 min of manual compression, not requiring RBC transfusion, & Grades 2-4 is everything else up to death) within 24 hours post-procedure.
Bottom Line: The jury is still out on best platelet transfusion practices prior to CVC placement, but I would strongly consider prophylactic platelet transfusion in patients with platelets < 30 x 109/L, those with underlying hematologic malignancy, and patients receiving larger CVCs such as dialysis lines. How much to transfuse in those with more severe thrombocytopenia is uncertain.
Separately, I would also strongly recommend use of US-guidance for any CVC placement in this population as well, based on practical common sense and some supportive literature as well.5
Additional Background: Data in pediatric oncology patients indicates that CVC placement with platelets <50 x 109/L is associated w/ increased occurence of minor but not major post-procedure bleeding,3 while adult data indicates that CVC placement can be performed until a threshold of 20 x 109/L before transfusions are needed to prevent severe bleeding.4
Additional Study Data:
Category: Administration
Keywords: POCUS, Lung Ultrasound, Pneumothorax (PubMed Search)
Posted: 5/29/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
We hope that you enjoy your Memorial Day!
Don't forget your Sandy Beach Sign vs Barcode Sign of Lung Ultrasound:
Normal lung will have good pleural sliding. When you image the lung with M-Mode it looks like a Sandy Beach.
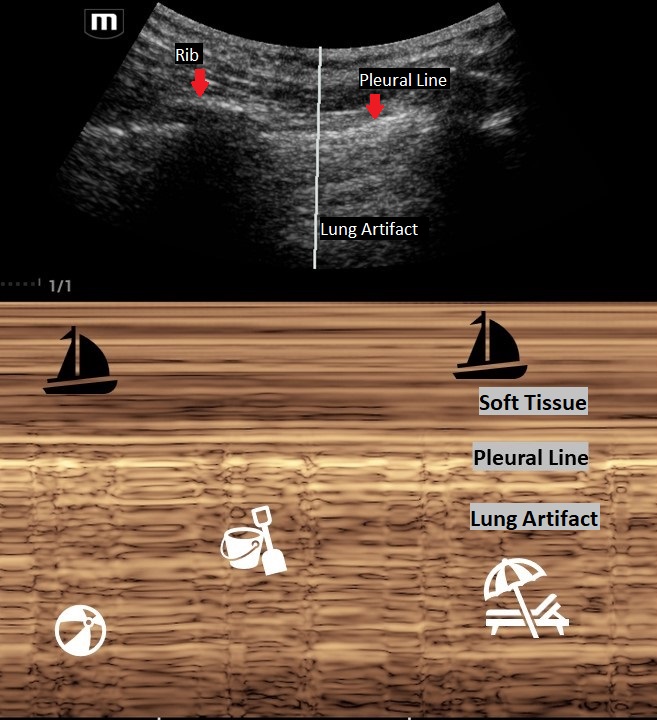
A lung with a pneumothorax will have poor lung sliding. When you image the lung with M-Mode it looks like a classic barcode or "stratosphere sign."
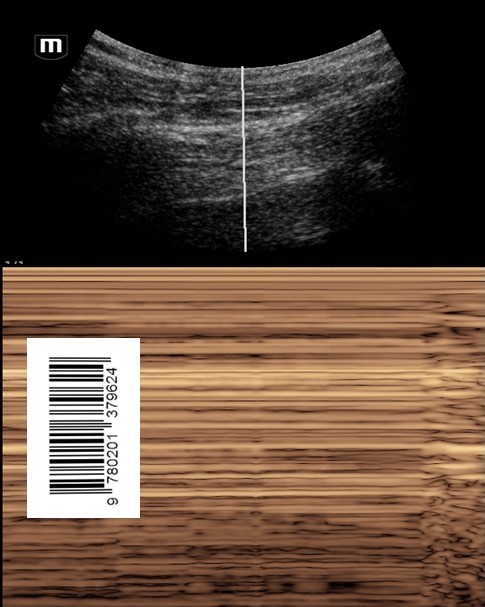
Make sure that you are on "Lung Mode" or decrease the gain to better image the movement of the pleural line. The negative predictive value for lung sliding on ultrasound is 99%. This means that if you see lung sliding you do not have a pneumothorax in that area. However, lung sliding is affected by certain conditions such as blebs, pulmonary fibrosis, pleural adhesions and right mainstem intubation. So, like any other radiology study, clinically correlate!
Thinking about placing a chest tube or have a patient with multiple rib fractures? Take a look at how to perform a Serratus Anteror Plane Block here: https://www.thepocusatlas.com/thoracoabdominal-blocks#Serratus
Husain LF, Hagopian L, Wayman D, Baker WE, Carmody KA. Sonographic diagnosis of pneumothorax. J Emerg Trauma Shock. 2012 Jan;5(1):76-81. doi: 10.4103/0974-2700.93116. PMID: 22416161; PMCID: PMC3299161.
Category: Trauma
Keywords: firearm, death, suicide, intentional, (PubMed Search)
Posted: 5/25/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
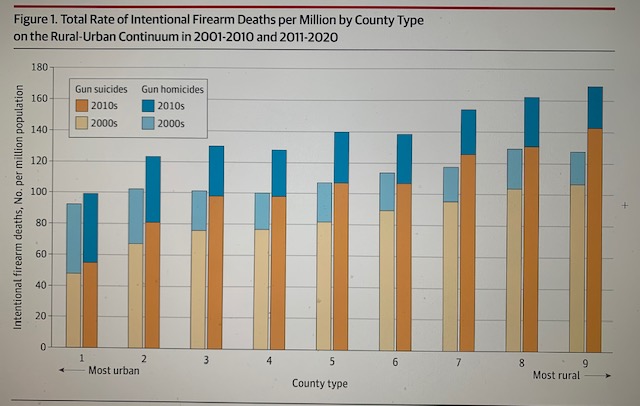
This study looked at 20 years of death by firearm and stratified the location of death from urban to rural. The authors concluded:
“Descriptively, in all county types and both decades of the study, per capita gun suicides were more common than per capita gun homicides, and the most rural counties had higher rates of firearm death compared with the most urban counties. Firearm death rates were meaningfully higher in 2011-2020 compared with 2001-2010, primarily because of an increase in gun suicides.”
Paul M. Reeping, PhD1; Allison Mak, MD2,3; Charles C. Branas, PhD1; et al
Firearm Death Rates in Rural vs Urban US Counties
JAMA Surg. Published online April 26, 2023. doi:10.1001/jamasurg.2023.0265
Category: Orthopedics
Keywords: overuse injury, wrist (PubMed Search)
Posted: 5/25/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Intersection syndrome
Intersection syndrome is an overuse injury of the forearm.
Pain is located approximately 2 finger breaths (4cm) proximal to the wrist joint.
https://www.sportsmedreview.com/wp-content/uploads/2020/11/intersectionsyndrome.png
Mechanism: friction is caused by repetitive wrist extension activities
Commonly: Rowing, skiing, tennis, canoeing and weightlifting
Friction may cause crepitus with finger/wrist extension.
Tenderness, mild swelling may be present
Category: Visual Diagnosis
Keywords: C Spine, osteomyelitis, (PubMed Search)
Posted: 5/25/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD


Neck pain and trouble swalowing. No trauma.
Osteomyelitis of the cervical spine is the least common location to find spinal infection. “Osteomyelitis of the cervical spine is a rare disease, representing only 3% – 6% of all cases of vertebral osteomyelitis. In contrast with other locations of spinal infections, osteomyelitis of the cervical spine can be a much more dramatic and rapidly deteriorating process, leading to early neurologic deficit”.
Note the bony destruction as well as the abscess labeled on the lateral view.
Category: Administration
Keywords: patient experience, clinician wellbeing (PubMed Search)
Posted: 5/24/2023 by Mercedes Torres, MD
Click here to contact Mercedes Torres, MD
Clinician Well-Being and the Patient Experience
Did you know that most patient experience responses are overwhelmingly positive? Rather than focusing all our attention on the bad, let’s focus on the good to promote clinician well-being. See below for a few key points from a recent study on this:
Consider emphasizing positive patient experiences when providing feedback to emergency physicians. It will promote clinician well-being and help improve performance in your practice.
Dudley J and Lee TH. Patient Experience and Clinician Well-Being Aren’t Mutually Exclusive. Harvard Business Review. Published online at hbr.org, July 18, 2022.
Category: Critical Care
Keywords: Intubation, Trauma, Cervical Spine, Laryngoscopy (PubMed Search)
Posted: 5/23/2023 by Mark Sutherland, MD
Click here to contact Mark Sutherland, MD
Ability to move the head and neck freely can be clutch in endotracheal intubation, so in patients such as certain trauma patients who may have c-spine instability and need to be immobilized, it's all the more important to choose the optimal intubation approach to maximize success and minimize head movement.
Choi et al recently published a study in Anesthesia looking at:
-Video laryngoscopy with a standard geometry Mac blade
vs
-Fiberoptic intubation
as the initial method for intubating patients in c-collars about to undergo spinal surgery. This is an interesting contrast between two extremes, as standard geometry is the most "traditional" approach, whereas fiberoptic is kind of the opposite end of the spectrum, jumping to a more advanced method which might be more flexible (no pun intended) but also introduces new complexities.
All outcomes actually favored standard geometry VL over fiberoptic, including first pass success (98% vs 91%), time to intubation (50s vs 81s) and need for additional airway maneuvers (18% vs 56%). There was no difference in complication rates, although a bigger study might be needed to find rare complications (this study had 330 patients).
In my opinion, it's unfortunate they didn't include hyperangulated VL, as it would be interesting to see how this approach compares. Personally I think of hyperangulated VL in these patients as a nice blend of the two methods, bringing the familiarity and speed of typical VL intubation, but often requiring less neck movement like fiberoptic.
Bottom Line: This study does not support a fiberoptic first approach to intubating patients with cervical spine instability. In fact, it may cause harm.
Choi S, Yoo HK, Shin KW, Kim YJ, Yoon HK, Park HP, Oh H. Videolaryngoscopy vs. flexible fibrescopy for tracheal intubation in patients with cervical spine immobilisation: a randomised controlled trial. Anaesthesia. 2023 May 5. doi: 10.1111/anae.16035. Epub ahead of print. PMID: 37145935.
Category: Trauma
Keywords: circulation, trauma, hemorrhage, atls (PubMed Search)
Posted: 5/20/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
It is time to abandon the ABC's that ATLS teaches and move to hemorhage control (circulation) as well as resucitation before we deal with airway in the majority of trauma patients. Tounriquets save lives. Pelvic binders save lives. Blood transfusion (whole blood) saves lives. Poisitive presssure ventilation, sedativies, and decreasing sympathetic drive in hypoternsive patients makes their hypotension worse.
Please consider changing to a CAB approach to the hyhpotensive trauma patient.
Ferrada P, Dissanaike S. Circulation First for the Rapidly Bleeding Trauma Patient—It Is Time to Reconsider the ABCs of Trauma Care. JAMA Surg. Published online May 17, 2023. doi:10.1001/jamasurg.2022.8436
Category: Quality Assurance/Quality Improvement
Keywords: Ct scan, abdominal pain, IV contrast, diagnosis (PubMed Search)
Posted: 5/20/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Does IV contrast help to make the diagnosis in ED abdominal pain patients undergoing CT scan? The authors of this study tried to answer that question. This study was a retrospective diagnostic accuracy study looking at contrast enhanced vs. non-enhanced images in 201 consecutive ED patients. The study demographics were:
“There were 201 included patients (female, 108; male, 93) with a mean age of 50.1 (SD, 20.9) years and mean BMI of 25.5 (SD, 5.4).”
The study found: “Unenhanced CT was approximately 30% less accurate than contrast-enhanced CT for evaluating abdominal pain in the ED.”
This study is limited by the small size, the overwhelming female to male inclusion, the reliance on radiology reading as the gold standard of pathology, and the retrospective nature. It does, however, show that there is a need for further study and at this time giving IV contrast has limited down side and potentially improves diagnostic accuracy of abdominal CT scans.
Shaish H, Ream J, Huang C, et al. Diagnostic Accuracy of Unenhanced Computed Tomography for Evaluation of Acute Abdominal Pain in the Emergency Department. JAMA Surg. Published online May 03, 2023. doi:10.1001/jamasurg.2023.1112
Category: Pediatrics
Keywords: IV, EMS, transfer, pediatrics (PubMed Search)
Posted: 5/19/2023 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Mangus CW, Canares T, Klein BL, et al. Interhospital Transport of Children With Peripheral Venous Catheters by Private Vehicle: A Mixed Methods Assessment. Pediatr Emerg Care. 2022;38(1):e105-e110. doi:10.1097/PEC.
Category: Misc
Keywords: EMS, Alternate destinations, pediatric, EMS, reduce transport times (PubMed Search)
Posted: 5/17/2023 by Jenny Guyther, MD
(Updated: 2/7/2026)
Click here to contact Jenny Guyther, MD
Ward CE, Singletary J, Campanella V, Page C, Simpson JN. Caregiver Perspectives on Including Children in Alternative Emergency Medical Services Disposition Programs: A Qualitative Study [published online ahead of print, 2023 May 5]. Prehosp Emerg Care. 2023;1-9. doi:10.1080/10903127.2023.
Category: Critical Care
Posted: 5/16/2023 by Mike Winters, MBA, MD
(Updated: 2/7/2026)
Click here to contact Mike Winters, MBA, MD
Bicarbonate Use for Lactic Acidosis?
Wardi G, et al. A review of bicarbonate use in common clinical scenarios. J Emerg Med. 2023; online ahead of print.
Category: Administration
Keywords: POCUS, Cardiac Arrest, Arterial Doppler (PubMed Search)
Posted: 5/15/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/7/2026)
Click here to contact Alexis Salerno Rubeling, MD
Did you know that you can use the linear probe with pulse wave (PW) doppler over the femoral artery to look for a pulse during CPR pauses?
Well, the researchers of this article took this skill one step further to evaluate if they could use the femoral artery PW doppler while CPR was in progress to look for signs of a pulse.
The authors found that:
- pulsations due to compressions were organized with uniform pulsations.
- when there was also native cardiac activity, the pulsations were nonuniform and may have an irregular cadence.
Although there were several limitations, Arterial doppler was 100% specific and 50% sensitive in detecting organized cardiac activity during active CPR.
Take Home Point: Take a look at your arterial doppler for signs of organized cardiac activity during a resuscitation.
Reference: Gaspari RJ, Lindsay R, Dowd A, Gleeson T. Femoral Arterial Doppler Use During Active Cardiopulmonary Resuscitation. Ann Emerg Med. 2023 May;81(5):523-531. doi: 10.1016/j.annemergmed.2022.12.002. Epub 2023 Feb 7. PMID: 36754697.
Category: Trauma
Keywords: hypoxia, delayed sequence, RSI, Ketamine, succinylcholine (PubMed Search)
Posted: 5/7/2023 by Robert Flint, MD
(Updated: 2/7/2026)
Click here to contact Robert Flint, MD
Delayed sequence intubation can be valuable in the agitated, combative trauma patients who will not tolerate pre-intubation pre-oxygenation. We know peri-intubation hypoxia leads to significant morbidity and mortality. DSI offers us an option to avoid peri-inubation hypoxia.
This study randomized 200 trauma patients into a rapid induction group (Ketamine followed immediately by succinylcholine with immediate intubation) vs. delayed induction group (Ketamine followed by a 3-minute oxygenation period followed by succinylcholine, followed by intubation). The authors found: “Peri-intubation hypoxia was significantly lower in group DSI (8 [8%]) compared to group RSI (35 [35%]; P = .001). First-attempt success rate was higher in group DSI (83% vs 69%; P = .02).”
Anjishnujit Bandyopadhyay 1, Pankaj Kumar, Anudeep Jafra, Haneesh Thakur, Laxmi Narayana Yaddanapudi, Kajal Jain Peri-Intubation Hypoxia After Delayed Versus Rapid Sequence Intubation in Critically Injured Patients on Arrival to Trauma Triage: A Randomized Controlled Trial. Anesth Analg. 2023 May 1;136(5):913-919. doi:10.1213/ANE.0000000000006171. Epub 2023 Apr 14.
Category: Orthopedics
Keywords: Baker's cyst, knee, effusion (PubMed Search)
Posted: 5/13/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
A Baker's cyst is a common incidental finding on ultrasound reports and bedside physical exam.
Clinically, these cysts are commonly found in association with intra-articular knee disorders. Most commonly: osteoarthritis, RA and tears of the meniscus.
Sometimes Baker's cysts are a source of posterior knee pain.
In an orthopedic clinic setting, Baker’s cysts are frequently discovered on routine MRI in patients with symptomatic knee pain. They tend to occur in adults from ages 35 to 70.
Over 90% of Baker’s cysts are associated with an intraarticular knee disorder. While most frequently associated with OA and meniscal tears, other knee pathologies that have been associated include inflammatory arthritis and tears of the anterior cruciate ligament.
DDX: DVT, cystic masses (synovial cyst), solid masses (sarcoma) and popliteal artery aneurysms.
Based on cadaveric studies, a valvular opening of the posterior capsule, proximal/medial and deep to the medial head of the gastrocnemius is present in approximately 50% of healthy adult knees.
Fluid flows in one way from knee joint to cyst and not in reverse. This valve allows flow only during knee flexion as it is compressed shut during extension due to muscle tension.
Most common patient complaint is that of the primary pathology, meniscal pain for example. At times, symptoms related to the cyst are likely due to increasing size as they may report fullness, achiness, stiffness.
In one small study, the most common symptoms were 1) popliteal swelling and 2) posterior aching. Patients may complain of loss of knee flexion from an enlarged cyst that can mechanically block full flexion.
If the Baker cyst is large enough the clinician will feel posterior medial fullness and mild tenderness to palpation. The cyst will be firm and full knee extension and softer during the flexion (Foucher’s sign).
This may help with differentiation from other popliteal masses (hematoma, soft tissue tumor, popliteal artery aneurysm).
With cyst rupture, severe pain can simulate thrombosis or calf muscle rupture, (warmth, tenderness, and erythema). A ruptured cyst can also produce bruising, which may involve the posterior calf starting from the popliteal fossa and extending distally towards the ankle.
Treatment: initial treatment for symptomatic Baker cysts is nonoperative unless vascular or neural compression is present (very unlikely)
Treatment involves physical therapy to maintain knee flexibility. A sports medicine physician may perform an intraarticular knee corticosteroid injection as this has been found to decrease size and symptoms of cysts in two-thirds of patients.
For patients that fail above, refer for surgical evaluation. Inform patients that they are not undergoing ED drainage of this symptomatic cyst due to the extremely high rate of recurrence which, as a result of the ongoing presence of the untreated intraarticular pathology, results in the recurrent effusion.
Category: Pharmacology & Therapeutics
Keywords: contraception (PubMed Search)
Posted: 5/11/2023 by Ashley Martinelli
(Updated: 2/7/2026)
Click here to contact Ashley Martinelli
Emergency contraception is highly effective at preventing unwanted pregnancies and has been on the market for 20+ years.
Levonogestrel (LNG) 1.5 mg PO x 1 dose (OTC Available)
Ulipristal acetate (UPA) 30 mg PO x 1 dose (Requires RX)
Original studies with LNG was estimated to prevent up to 80% of expected pregnancies. In the subsequent trials that brought UPA to the market and compared the two medications, LNG prevented 69% (95% CI, 46-82%) and 52.2% (95% CI, 25.1-69.5%).
While pregnancy rates are low with both options there is concern with patients of higher weight/BMI that the effectiveness of levonorgestrel decreases as weight rises. One large study of over 1700 patients specifically noted that a weight > 75 kg was associated with up to 6.5% pregnancy rate (95% CI 3.1-11.5) compared to 1.4% (95% CI 0.5-3.0) in patients weighing 65-75 kg. Patients weighing > 85 kg had similarly high rates at 5.7% (95% CI 2.9-10.0).
The cost difference is minimal between products, especially when considering costs associated with treatment failures and subsequent need for care- the largest difference is with respect to access as LNG is OTC and UPA requires an RX. Either can be administered in an ED setting as long as they are on formulary.
ACOG also recommends that ulipristal be utilized for it higher overall efficacy compared to levonorgestrel.
Consider:
For patients above 75 kg, ulipristal can be used as first line emergency contraception for up to 5 days following unprotected intercourse.
Patients < 75 kg and < 72 hours following unprotected intercourse can use levonorgestrel or ulipristal as an appropriate emergency contraception method.
Patients < 75 kg and 72-120 hours following unprotected intercourse should use ulipristal due to its efficacy beyond 72 hours.
Kapp N, Abitbol JL, Mathe H, et al. Effect of body weight and BMI on the efficacy of levonogestrel emergency contraception. Contraception. 2015;91(2):97-104.
Emergency contraception. Practice Bulletin No. 152. American College of Obstetricians and Gynecologists. Obstet Gynecol 2015;126:e1–11
Category: Gastrointestional
Keywords: cannabis hyperemesis syndrome (PubMed Search)
Posted: 5/10/2023 by Neeraja Murali, DO, MPH
Click here to contact Neeraja Murali, DO, MPH
Bottom Line: With the increasing acceptance and legalization of marijuana and its derivatives, emergency departments have seen an increase in patients with cannabis hyperemesis syndrome (CHS). In this patient population, when other pathologies have been excluded, consider droperidol (0.625 mg – 2.5 mg) or haloperidol (0.05 mg/kg or 0.1 mg/kg) for management of symptoms.
Two separate articles were reviewed for this pearl. One is a systematic review of existing literature, and the other is a randomized controlled trial.
The systematic review examined 17 existing studies, including case reports, RCTs, retrospective studies, and other systematic reviews. This included adults aged 18-85 who were using recreational or medicinal cannabinoids. There was a consensus that cessation of cannabinoid use is the best way to alleviate symptoms of CHS. Other options discussed include:
As mentioned above, the HaVOC study examined various doses of haloperidol versus odansetron. This randomized controlled trial was triple blinded and had three groups: haloperidol 0.05 mg/kg or 0.1 mg/kg or odansetron 8 mg IV. The outcome of interest was reduction in abdominal pain and nausea at two hours after treatment. Either dose of haloperidol was found to be superior to odansetron, with improvements in pain and nausea (54% versus 29%; 95% CI -16% to 59%), and less use of rescue antiemetics (31% versus 59%, with 95% CI -61% to 13%). Haloperidol also resulted in shorter ED length of stay (3.1 h vs 5.6 h, 95% CI 0.1-5.0 h, p=0.03). However, 2 patients in the high dose haloperidol group had dystonic reactions precipitating return visits. The study does not specifically discuss differences in outcomes between the high and lower dose haloperidol groups.
Neither paper discussed the best alternatives when QTc prolongation is of concern. Clinicians should use their best judgment and the available information when deciding on a treatment option.
Senderovich H, Patel P, Jimenez Lopez B, Waicus S. A Systematic Review on Cannabis Hyperemesis Syndrome and Its Management Options. Med Princ Pract. 2022;31(1):29-38. doi:10.1159/000520417
Ruberto AJ, Sivilotti MLA, Forrester S, Hall AK, Crawford FM, Day AG. Intravenous Haloperidol Versus Ondansetron for Cannabis Hyperemesis Syndrome (HaVOC): A Randomized, Controlled Trial. Ann Emerg Med. 2021;77(6):613-619. doi:10.1016/j.annemergmed.2020.08.021
Category: Critical Care
Keywords: OHCA, Critical Care, Whole Body CT, Post Cardiac Arrest Care (PubMed Search)
Posted: 5/9/2023 by Lucas Sjeklocha, MD
Click here to contact Lucas Sjeklocha, MD
Just scan ‘em? Should everyone with unexplained out-of-hospital cardiac arrest get whole-body CT/CTA?
Background: Determination of the cause and subsequent management of out-of-hospital cardiac arrest is clinically challenging in those patients who survive to hospital admission without a clear diagnosis. CT imaging is often used to ascertain the cause of an arrest, find potentially intervenable etiologies, and assess for neurological injury but this practice and diagnostic yield are inconsistent and not well studied.
Study and Methods: The CT FIRST study is a single center cohort study using head-to-pelvis contrasted triple phase CT within 6 hours for cardiac arrest without obvious cause (sudden death CT or SDCT) studied in a before and after manner compared to usual care to determine the influence of early pan CT on diagnostic yield and outcomes. The primary outcome was diagnostic yield following SDCT and secondary outcomes include time to diagnosis of “time critical” findings and survival to discharge. 104 patients undergoing SDCT were compared to 143 historical controls after study implementation. Patients deemed to have a clear cause or are too unstable for CT were among exclusions.
Results: For the primary outcome of diagnostic yield: 92% of SDCT cohort received a separately adjudicated diagnosis for the arrest compared to 75% of the control cohort (p = 0.001). With time to such diagnosis of 3.1hrs in SDCT versus 14.1hrs of controls, with 39% versus 17% being made by CT. Time critical diagnoses including MI, PE, aortic dissection, pneumonia, embolic or hemorrhagic CVA and abdominal catastrophe were identified in 32% versus 24% (non significant) of the cohorts with delay greater than 6hrs to diagnosis reported in 12% in SDCT versus 62% in usual care (p=0.001).
There was no difference in survival to hospital discharge and no difference in safety measures and no evaluation reporting changes to and timing of patient managements.
The SDCT cohort had 100% scan rate compared to usual care where 81% received early head CT with chest CT and abdominal CT done in 36% and 18%, respectively. Notably there were no CT reported diagnoses that were later reversed on adjudication in either cohort. The planned economic and resource analysis was not reported in this study.
Discussion: There was a notable increase in diagnostic yield based on the study design with faster time to potentially time sensitive diagnoses. There were, however, no differences in mortality and it was not clear the degree to which these diagnoses influenced patient management given the limited numbers in this study and diverse set of diagnoses associated with cardiac arrest. Like previous studies of selective versus whole body CT in trauma populations, the increased diagnostic yield was not associated with reduced mortality or reported changes in management. The yield numbers suggest increased confidence by exclusion as much as positive findings of the cause. As always, the caveats of a relatively small single center before-and-after cohort study apply.
An interesting twist is that no CT diagnosis pointing to the cause of the arrest was reversed on subsequent review, this may speak to the accuracy of modern CT and radiology interpretation, but I sometimes worry that this can also be reflective of diagnostic fixation, especially with “objective” tests, as well as nihilism about the utility of clinical diagnosis.
That said, non-selective CT has many potential benefits for many critically ill and unexaminable populations with diagnostic uncertainty, as demonstrated here, which must be balanced against risks of intrahospital transport and of resource utilization as we do not yet have clear data that patients benefit from the practice despite increased diagnostic yield.
Kelley R.H. Branch, M.O. Gatewood, P.J. Kudenchuk et al., Diagnostic yield, safety, and outcomes of Head-to-pelvis sudden death CT imaging in post arrest care: The CT FIRST cohort study, Resuscitation, https://doi.org/10.1016/j. resuscitation.2023.109785
