Category: Administration
Keywords: predictive rule, EHR, utilization, AI (PubMed Search)
Posted: 6/16/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Author- Steve Schenkel, MD MPP Professor of Emergency Mediciner at UMEM:
A recent Annals of Emergency Medicine Publication (here https://www.annemergmed.com/article/S0196-0644(22)01276-8/fulltext) tested a predictive rule for Likelihood to Occupy an Inpatient Bed associated with a common Electronic Health Record.
At the individual patient level, the score performed ok. Depending on the chosen threshold, it traded off sensitivity and specificity and generally became more accurate the longer the patient was in the ED.
The authors and the associated editorial (here https://www.annemergmed.com/article/S0196-0644(22)01401-9/fulltext) suggest a different, potentially more beneficial use: to allow aggregate prediction of admissions across an entire department and therefore prompt earlier planning to prevent crowding on account of boarding.
The takeaway: Administrative prediction rules oriented toward individual patients may be more meaningfully used to predict resource needs, including in-patient beds, across the ED population.
Category: Critical Care
Keywords: NEWS, MEWS, IEWS, international Early Warning Score, mortality (PubMed Search)
Posted: 6/27/2023 by Quincy Tran, MD, PhD
(Updated: 2/8/2026)
Click here to contact Quincy Tran, MD, PhD
Settings: Retrospective data from 3 Dutch EDs (development of the score), 2 Denmark ED (for validation of the score). The novel score (International Early Warning Score) will be composed of the National Early Warning Score (NEWS) + Age +Sex
Components of the National Early Warning Score:
Participants: All adult patients in the Netherlands Emergency department Evaluation Database (NEED) and Danish Multicenter Cohort (DMC).
Outcome measurement: in-hospital mortality, including death in EDs.
Study Results:
Discussion:
Conclusion:
This multicenter study showed that IEWS perform better than the NEWS for predicting in-hospital mortality for ED patients.
Candel BGJ, Nissen SK, Nickel CH, Raven W, Thijssen W, Gaakeer MI, Lassen AT, Brabrand M, Steyerberg EW, de Jonge E, de Groot B. Development and External Validation of the International Early Warning Score for Improved Age- and Sex-Adjusted In-Hospital Mortality Prediction in the Emergency Department. Crit Care Med. 2023 Jul 1;51(7):881-891. doi: 10.1097/CCM.0000000000005842. Epub 2023 Mar 23. PMID: 36951452; PMCID: PMC10262984.
Category: Orthopedics
Keywords: POCUS, Hip Fractures, Nerve Blocks, Administration (PubMed Search)
Posted: 6/26/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
The use of a fascia iliaca compartment block has been shown to reduce pain, decrease length of stay and decrease the opiate requirements for patients with hip fractures.
Check out this page on how to perform this procedure.
Fascia iliac blocks can be challenging to implement routinely in the emergency department. Studies show that 2.5% of eligible patients, despite departmental implementation, receive a block.
One recently published article showed that large scale multi-disciplinary implementation can increase the use of fascia iliac blocks. After implementation, the study team found that 54% of eligible patients received a fascia iliac block.
This article is interesting as it provides helpful resources including physician and nursing protocols for performing this block.
Downs T, Jacquet J, Disch J, Kolodychuk N, Talmage L, Krizo J, Simon EL, Meehan A, Stenberg R. Large-scale Implementation of Fascia Iliaca Compartment Blocks in an Emergency Department. West J Emerg Med. 2023 May 3;24(3):384-389. doi: 10.5811/westjem.58793. PMID: 37278790; PMCID: PMC10284502.
Category: Trauma
Keywords: lidocaine, trauma, rib fractures (PubMed Search)
Posted: 6/25/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Use of intravenous lidocaine has been proposed as an adjunct/replacement for opioids in trauma patients with rib fractures. These small studies show a signal that the use of lidocaine decreased the need for opiate pain medication in this cohort of patients. Larger studies are needed, however, trauma surgeons maybe reaching for intravenous lidocaine in patients they are admitting with rib fractures. Also, transdermal lidocaine patches have been shown to have a similar effect in this patient cohort. “In admitted trauma patients with acute rib fractures not requiring continuous intravenous opiates, lidocaine patch use was associated with a significant decrease in opiate utilization during the patients’ hospital course.” 3
1. Patton, Petrease MD, MSc; Vogt, Kelly MD, MSc; Priestap, Fran MSc; Parry, Neil MD; Ball, Ian M. MD, MSc. Intravenous lidocaine for the management of traumatic rib fractures: A double-blind randomized controlled trial (INITIATE program of research). Journal of Trauma and Acute Care Surgery 93(4):p 496-502, October 2022. | DOI: 10.1097/TA.0000000000003562
2. Jeff Choi , Kirellos Zamary, Nicolas B. Barreto, Lakshika Tennakoon, Kristen M. Davis, Amber W. Trickey, David A. Spain. Intravenous lidocaine as a non-opioid adjunct analgesic for traumatic rib fractures. Published: September 28, 2020 https://doi.org/10.1371/journal.pone.0239896
3. Johnson M, Strait L, Ata A, et al. Do Lidocaine Patches Reduce Opioid Use in Acute Rib Fractures? The American SurgeonTM. 2020;86(9):1153-1158. doi:10.1177/0003134820945224
Category: Administration
Keywords: concussion recovery (PubMed Search)
Posted: 6/24/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
How much screen time after concussion?
Adolescents spent more than 7 hours daily on screen time during the pandemic.
Historically, experts recommended screen time abstinence to various degrees after concussion.
Prior study: RCT of concussion patients (ages 12 to 25) found that those who abstain from screen time for the first 48 hours recovered 4.5 days sooner than those who were permitted screen time.
Population: 633 children and adolescents with acute concussion and 334 with orthopedic injuries aged 8 to 16, recruited from 5 Canadian pediatric emergency departments.
Post concussion symptoms were measured at 7 to 10 days, weekly for three months, and biweekly for three to six months post injury. Screen time was measured.
Results: Screen time was a significant predictor of post concussion symptom recovery with both parent reported somatic and self-reported cognitive symptoms.
There may be an effect of low to moderate screen time (Goldilocks effect) demonstrating that those in the 25th to 50th percentiles had less severe symptoms than those on the higher end of screen time use or those who minimally use of screens!
Low and high screen time were both associated with relatively more severe symptoms in the concussion group compared to the orthopedic injury group during the first 30 days post recovery but not after 30 days.
Conclusion: The association of early screen time with post concussion symptoms is not linear. Recommending moderation in screen time may be the best approach to clinical management.
Children need to strike a balance between avoiding boredom, deconditioning, isolation, and overexerting themselves physically or cognitively.
Cairncross M, al. Early Postinjury Screen Time and Concussion Recovery. Pediatrics. 2022
Category: EMS
Keywords: ambulance, crash, response, fatality, collision (PubMed Search)
Posted: 6/22/2023 by Jenny Guyther, MD
Click here to contact Jenny Guyther, MD
Prehosp Emerg Care. 2023;27(4):455-464. doi:10.1080/10903127.2022.
Category: Vascular
Keywords: POCUS, AAA, (PubMed Search)
Posted: 6/19/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
It is difficult to diagnosis a ruptured AAA with POCUS. However, based on one systematic review and meta-analysis, POCUS has a sensitivity of 97.8% and a specificity of 97% for diagnosing AAA in patients supsected of having a ruptured AAA.
Remeber:
Laslty, make sure you are measuring the aortic wall and not a mural thrombus.
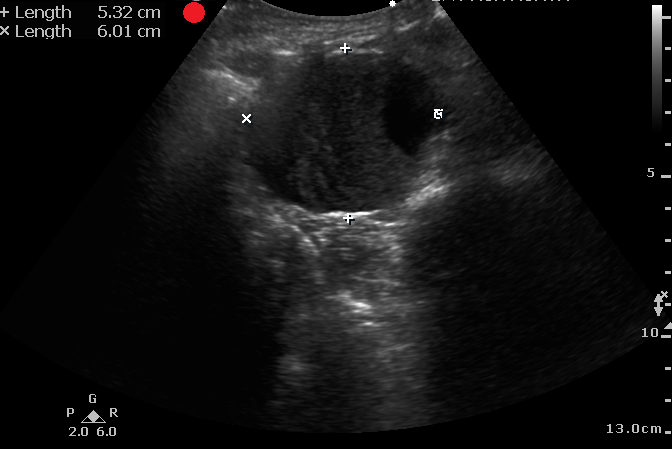
Fernando SM, Tran A, Cheng W, Rochwerg B, Strauss SA, Mutter E, McIsaac DI, Kyeremanteng K, Kubelik D, Jetty P, Nagpal SK, Thiruganasambandamoorthy V, Roberts DJ, Perry JJ. Accuracy of presenting symptoms, physical examination, and imaging for diagnosis of ruptured abdominal aortic aneurysm: Systematic review and meta-analysis. Acad Emerg Med. 2022 Apr;29(4):486-496. doi: 10.1111/acem.14475.
Category: Ophthamology
Keywords: corneal perforation (PubMed Search)
Posted: 6/16/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD

What is this called? What does it indicate?
Seidel Sign. Assoicated with corneal perforation.
https://webeye.ophth.uiowa.edu/eyeforum/atlas/pages/corneal-perforation-seidel-posative-.html
Category: Trauma
Keywords: spinal trauma, injury, spine (PubMed Search)
Posted: 6/18/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
Category: Pediatrics
Keywords: neonatal fever, cellulitis, bacteremia (PubMed Search)
Posted: 6/16/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Kaplin, Ron. Clinical Presentation and Approach to Evaluation and Management. Pediatric Emergency Care 2023; 39(3):188-189.
Category: Toxicology
Keywords: Lithium, Lab error, Toxicity (PubMed Search)
Posted: 6/15/2023 by Natasha Tobarran, DO
(Updated: 2/8/2026)
Click here to contact Natasha Tobarran, DO
Lithium toxicity can present acutely with gastrointestinal symptoms and chronically with neurologic symptoms such as tremor and ataxia. Diagnosis and treatment with normal saline hydration and/or dialysis depends on lithium levels in conjunction with signs and symptoms.
Lithium levels can be falsely elevated when blood samples are collected in green top tubes which contain lithium heparin, or if the blood collection volume is too small. Not recognizing that a lithium level may be falsely elevated can lead to misdiagnosis as well as unnecessary hospitalizations and treatments. The study by Wills et al found lithium levels as high as 4 mmol/L (therapeutic range 0.6-1.2 mmol/L) in lithium naïve volunteers collected in the wrong tube and with small blood volumes. If a patient has an elevated lithium level in the absence of lithium toxicity symptoms, consider a falsely elevated level and redraw using the appropriate tube and sample size.
In summary:
Wills BK, Mycyk MB, Mazor S, Zell-Kanter M, Brace L, Erickson T. Factitious lithium toxicity secondary to lithium heparin-containing blood tubes. J Med Toxicol. 2006 Jun;2(2):61-3. doi: 10.1007/BF03161172. PMID: 18072115; PMCID: PMC3550057.
Category: Administration
Keywords: STEMI, pericarditis, (PubMed Search)
Posted: 6/11/2023 by Leen Alblaihed, MBBS, MHA
Click here to contact Leen Alblaihed, MBBS, MHA
a 37 year old patient comes in with chest pain, you obtain the following ECG. Is this a STEMI or Pericarditis?
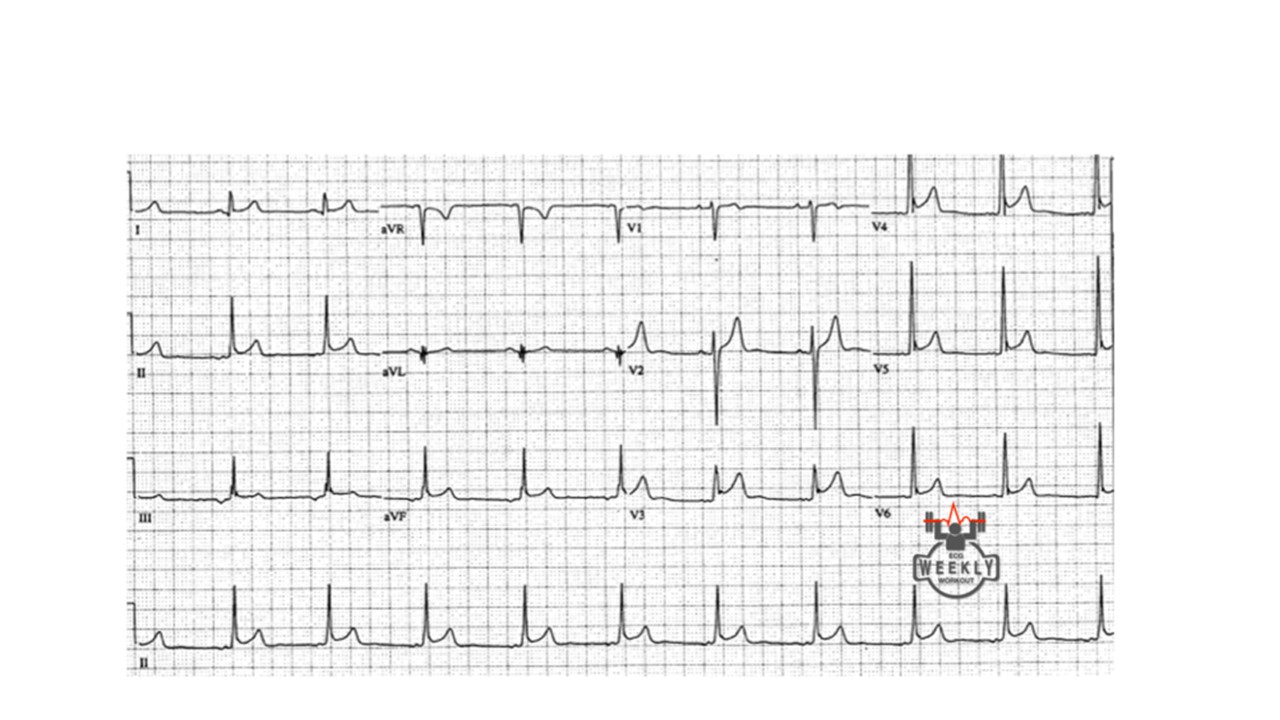
How can you tell? well, you follow the algorithm Dr. Mattu taught us....
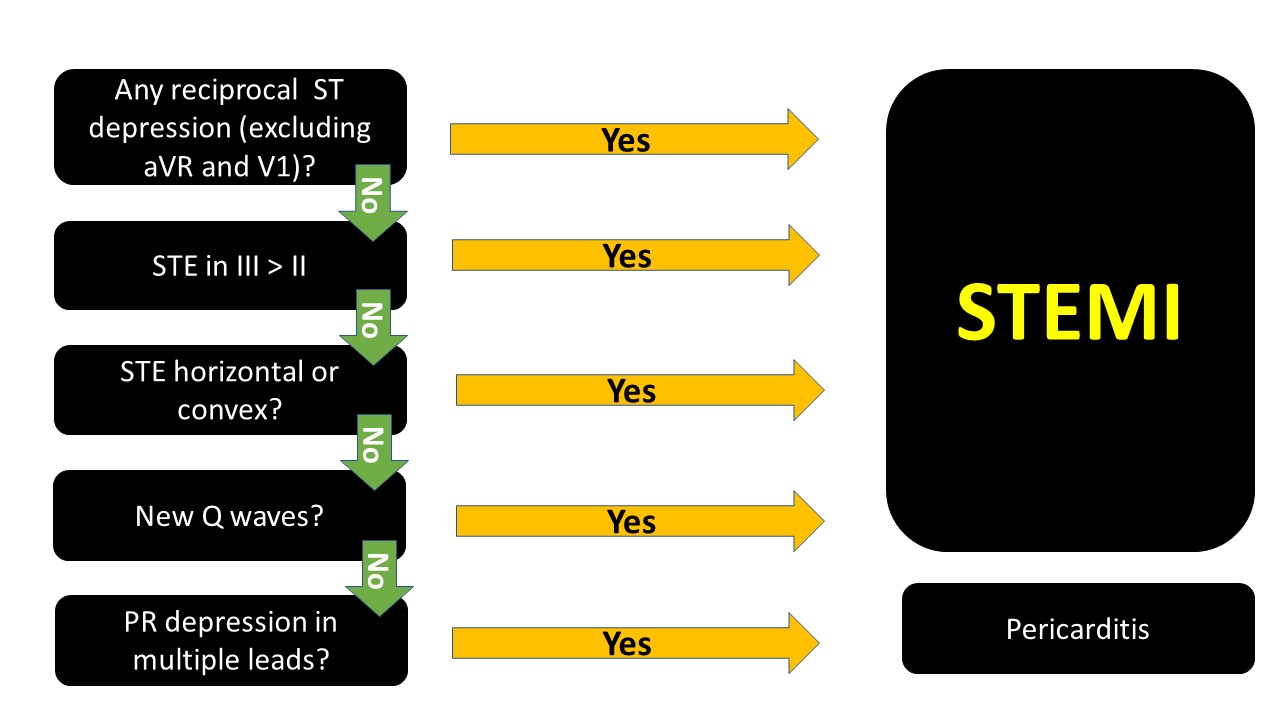
The ECG above, if you go through the algorithm you will see that it is most likely pericarditis.
note that PR depression can be transient and you might not see them.
When in doubt, it is not wrong to consult cardiology. Getting serial ECGs also is important, STEMIs will usually evolve.
Category: Trauma
Keywords: thoracotomy, survival, prognosis (PubMed Search)
Posted: 6/9/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
Recognizing that the studies discussing emergency department thoracotomy (ERT) in traumatic injuries are performed at large institutions where surgical back-up is available, emergency physicians should be familiar with the indications of emergency department thoracotomy in the setting of trauma. An informed decision should be made based on resources available along with the limited literature available to make the best decision for the patient and staff present.
Adding to last week’s pearl of no cardiac activity and no pericardial fluid on FAST exam, what else prognosticates intact survival? A 2020 paper concluded “ERT had the highest survival rates in patients younger than 60 years who present with signs of life after penetrating trauma. None of the patients with blunt trauma who presented with no signs of life survived.” 1A review in Trauma last month recommended: “Based on our scoping review of existing literature, we can conclude three major findings in the context of RT: (1) Resuscitative Thoracotomies (RT) performed in the setting of blunt trauma have a worse prognosis compared to patients undergoing RT for penetrating injuries, (2) procedures that have the potential to delay patient transport to hospital, such as intubation, may significantly increase the risk of mortality and (3) the presence of signs of life or hemodynamic stability in the prehospital or in-hospital setting are positive survival predictors in the setting of RT” 2 The best outcome is in patients brought immediately to an ED (preferably a trauma center) with limited on scene time. Police transport had a major association with survival in these patients. Stab wounds have the highest rate of intact survival.
For those at non-trauma centers, have a conversation within your ED group as well as with general surgeons (if available) to decide ahead of time if this procedure will be utilized in the setting of traumatic cardiac arrest and in which patient population.
1. Vahe S Panossian , Charlie J Nederpelt , Majed W El Hechi , David C Chang , April E Mendoza , Noelle N Saillant , George C Velmahos Haytham M A Kaafarani Emergency Resuscitative Thoracotomy: A Nationwide Analysis of Outcomes and Predictors of Futility J Surg Res. 2020 Nov;255:486-494. doi: 10.1016/j.jss.2020.05.048. Epub 2020 Jul 1.
2. Radulovic N, Wu R, Nolan B. Predictors of survival in trauma patients requiring resuscitative thoracotomy: A scoping review. Trauma. 2023;0(0). doi:10.1177/14604086231156265
Category: Orthopedics
Keywords: shoulder, Adhesive capsulitis (PubMed Search)
Posted: 6/10/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Adhesive capsulitis aka frozen shoulder
Definition: Gradual development of global limitation of both active and passive shoulder motion, characterized by severe pain and lack of radiographic findings
Idiopathic loss of BOTH active and passive motion (significant reduction of at least 50%)
Motion is stiff and painful especially at the extremes.
Occurs due to thickening and contracture of the shoulder capsule.
Affects up to 8-10% of people of working age.
Affects patients between the ages of 40 and 60.
Peak age mid 50s
Onset before 40 is rare (consider other diagnosis).
Affects women more than men.
Diabetes is the most common risk factor.
Patients with DM, suffer a more prolonged course and are more resistant to therapy
Also associated with thyroid disease and prolonged immobilization
Increased risk following trauma to shoulder region (rotator cuff tear, following shoulder surgery, fracture of proximal humerus)
Presents unilaterally (other shoulder may become involved in next 5 years)
Slight increased risk of non-dominant shoulder
Category: Airway Management
Keywords: hypotension, pharmacology, RSI (PubMed Search)
Posted: 6/9/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Take away: Be prepared (with blood products and/or vasopressors) for hypotension in trauma patients post-intubation particularly the elderly and severely injured. Pre-intubation tachycardia predicts post-intubation hypotension. Resuscitation with saline in traumatically injured patients is inferior to blood products or permissive hypotension.
A UK study retrospectively looked at trauma patients undergoing helicopter based emergency medicine intubation using induction agents of fentanyl, ketamine, and rocuronium for hypotensive episodes. “This study demonstrates that more than one in five patients who undergo PHEA have a new episode of significant hypotension within the first ten minutes of induction. Increasing patient age, multi-system injuries, a higher baseline heart rate, and intravenous crystalloid administration by the ambulance service before HEMS arrival were all significantly associated with PIH, whereas the addition of fentanyl to the induction drug regime was not.”
Price, J., Moncur, L., Lachowycz, K. et al. Predictors of post-intubation hypotension in trauma patients following prehospital emergency anaesthesia: a multi-centre observational study. Scand J Trauma Resusc Emerg Med 31, 26 (2023). https://doi.org/10.1186/s13049-023-01091-z
Category: Pharmacology & Therapeutics
Keywords: nitroglycerin, administration set, drug sorption, PVC tubing, polyethylene, SCAPE (PubMed Search)
Posted: 6/8/2023 by Matthew Poremba
(Updated: 2/8/2026)
Click here to contact Matthew Poremba
Nitroglycerin easily migrates into polyvinyl chloride (PVC), a plastic commonly used in intravenous tubing due to its flexibility and low cost. A slow rate of flow and long tubing length increase the loss of nitroglycerin. While using less absorptive tubing (i.e. polyethylene or polypropylene) when administering nitroglycerin is recommended, most published clinical studies looking at nitroglycerin have used PVC tubing.
A 1989 study compared nitroglycerin delivery through PVC tubing and low sorbing tubing at various concentrations and flow rates.1 Samples were obtained from the nitroglycerin bottle and the distal end of the tubing at several time points.
A 2018 study enrolled 8 volunteers to receive nitroglycerin infusions through PVC tubing and low sorbing polyolefin tubing.2
Bottom Line: Most studies evaluating nitroglycerin use in various clinical scenarios have used PVC tubing. Doses based on use with PVC tubing may be too high when using less absorptive tubing. Employing more conservative dosing strategies when using low sorbing tubing can help mitigate the risk of adverse effects (i.e. hypotension, headache).
Category: Critical Care
Keywords: Upper GI Hemorrhage, Cirrhosis, Antibiotic Prophylaxis, SBP, ceftriaxone (PubMed Search)
Posted: 6/6/2023 by Zach Rogers, MD
(Updated: 2/8/2026)
Click here to contact Zach Rogers, MD
Prophylactic antibiotic use in cirrhotic patients with an upper GI bleed has been demonstrated to have a mortality benefit in multiple randomized clinical trials. Some trials as well demonstrated a decreased risk of rebleeding as well as a shorter hospital length of stay (1,2).
The exact means of protection is not entirely clear and its benefit is seen in both variceal and nonvariceal hemorrhages as well as in cirrhotic patient both with and without ascites.
There does appears to be a close interplay between cirrhosis bleeding risk and infection, with infection being a common precipitating factor for upper GI bleed.
The antibiotic of choice is ceftriaxone 1 gram IV daily for seven days. Although in case of allergy/intolerance, fluoroquinolones or aminoglycosides may be used as alternatives (3).
Bottom line:
All forms of upper GI hemorrhage in cirrhotic patients warrant prophylactic antibiotic use (regardless of the presence of ascites) as well as a diligent search and exclusion of possible infectious sources.
1. Chavez-Tapia NC, Barrientos-Gutierrez T, Tellez-Avila FI, Soares-Weiser K, Uribe M. Antibiotic prophylaxis for cirrhotic patients with upper gastrointestinal bleeding. Cochrane Database Syst Rev. 2010 Sep 8;2010(9):CD002907. doi: 10.1002/14651858.CD002907.pub2. PMID: 20824832; PMCID: PMC7138054.
2. Wong YJ, Tan CK, Yii YL, et al. Antibiotic prophylaxis in cirrhosis patients with upper gastrointestinal bleeding: An updated systematic review and meta?analysis. Portal Hypertension & Cirrhosis. 2022;1(3):167-177. doi:10.1002/poh2.35
3. Sanchez?Jimenez B, Chavez?Tapia NC, Jakobsen JC, Nikolova D, Gluud C. Antibiotic prophylaxis for people with cirrhosis and variceal bleeding. Cochrane Database Syst Rev. 2018 Dec 4;2018(12):CD013214. doi: 10.1002/14651858.CD013214. PMCID: PMC6517118.
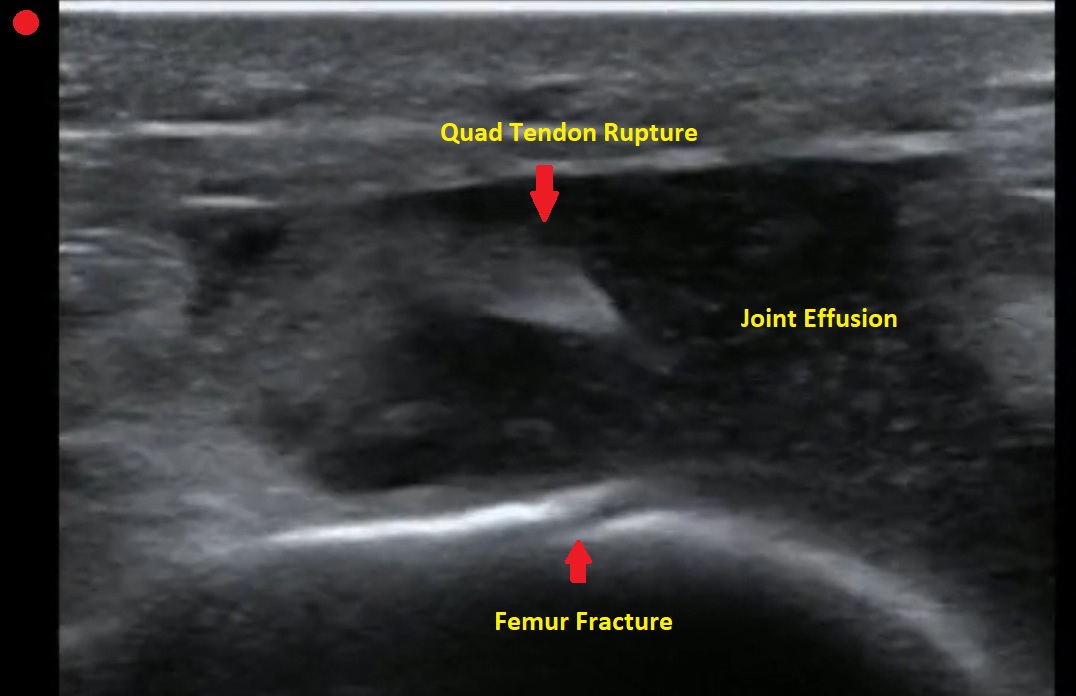
Category: Orthopedics
Keywords: POCUS, Knee Pain, Tendon Rupture (PubMed Search)
Posted: 6/5/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Pt presents to the emergency department with knee pain.
You decide to ultrasound the proximal knee. You place your ultrasound probe in the midline of the knee with your probe marker towards the patient's head.
What is the diagnosis?
-
--
---
--
-
The answer is a quadriceps tendon rupture with femur fracture.
Category: Trauma
Keywords: thoracotomy, REBOA, FAST, survival (PubMed Search)
Posted: 6/4/2023 by Robert Flint, MD
(Updated: 2/8/2026)
Click here to contact Robert Flint, MD
Bottom Line: Lack of pericardial fluid or cardiac motion on FAST exam leads to no intact survivors for ED RT for trauma.
Zone 1 REBOA may be as good or better than ED RT for those requiring aortic occlusion after trauma.
Intact neurologic survival after emergency department resuscitative thoracotomy (ED RT) for trauma is low. Best outcomes have been shown for stab wounds to the chest with loss of vital signs in the ED or just prior to ED arrival. Worst outcomes are for blunt trauma with loss of vital signs in the field.
Two studies help us further evaluate the use of emergency department resuscitative thoracotomy. Inaba et al. illustrate in patients undergoing a FAST exam prior to or concomitant with ED RT “The likelihood of survival if pericardial fluid and cardiac motion were both absent was zero.” Cralley et al. compared survival after ED RT to Resuscitative Endovascular Balloon Occlusion of the Artery (REBOA) zone 1 (above celiac axis) and found REBOA was as good or better when used in centers with experience with both procedures. They advocate for a randomized trial to compare the two procedures further.
Inaba, Kenji MD*; Chouliaras, Konstantinos MD*; Zakaluzny, Scott MD*; Swadron, Stuart MD†; Mailhot, Thomas MD†; Seif, Dina MD†; Teixeira, Pedro MD*; Sivrikoz, Emre MD*; Ives, Crystal MD*; Barmparas, Galinos MD*; Koronakis, Nikolaos MD*; Demetriades, Demetrios MD*. FAST Ultrasound Examination as a Predictor of Outcomes After Resuscitative Thoracotomy: A Prospective Evaluation. Annals of Surgery 262(3):p 512-518, September 2015. | DOI: 10.1097/SLA.0000000000001421
Alexis L. Cralley, MD1; Navin Vigneshwar, MD, MPH1; Ernest E. Moore, MD1,2; et al
Zone 1 Endovascular Balloon Occlusion of the Aorta vs Resuscitative Thoracotomy for Patient Resuscitation After Severe Hemorrhagic Shock JAMA Surg. 2023;158(2):140-150. doi:10.1001/jamasurg.2022.6393
Category: Quality Assurance/Quality Improvement
Keywords: Emergency Department Boarding, Emergency Department Crowding (PubMed Search)
Posted: 6/3/2023 by Brent King, MD
Click here to contact Brent King, MD
The authors of this study retrospectively compared the 10-day mortality rates of patients who were triaged to levels 3-5 on the Scandinavian Rapid Emergency Triage and Treatment System (RETTS) during times of ED crowding (as measured by length of stay and percentage bed occupancy) with those who came to the ED at other times.
Patients were divided into four quartiles, corresponding with 2-hour length of stay blocks with quartile one having a length of stay of 2 or fewer hours and quartile four having a length of greater than 8 hours
Results: 705,076 patients were seen in one of two EDs from 2009 to 2016. The 10-day mortality rate was 0.09% (n = 623). The authors found an increased 10-day mortality for patients in quartile four as compared to those in quartile one “(adjusted odds ratio 5.86; 95% confidence interval [CI] 2.15 to 15.94)” This was also true for times when the ED occupancy ratio was greater than one (more than one patient in the ED per available bed). “Adjusted odds ratios for ED occupancy ratio quartiles 2, 3, and 4 versus quartile 1 were 1.48 (95% CI 1.14 to 1.92), 1.63 (95% CI 1.24 to 2.14), and 1.53 (95% CI 1.15 to 2.03), respectively”
Older patients and those with co-morbidities were at greatest risk but lower-acuity patients in all age and morbidity classes had an increased risk of death within 10 days if they came to the ED when it was crowded.
The RETTS Triage System as Described by the Authors:
A “ 5-level triage scale descending from red (1) to blue (5), in which red represents the most urgent level. RETTS is based on one main principle: whether the patient is assessed as unstable or stable during triage. Unstable patients are experiencing potentially life-threatening conditions and are allocated to 1 of the 2 highest triage levels (1 to 2), whereas stable patients are allocated to 1 of the 3 lowest triage levels (3 to 5). Stable patients need medical attention but are considered able to wait because they are not at any obvious medical risk. RETTS uses a combination of vital signs and 59 chief complaint algorithms to allocate the triage level. The vital signs have cutoff levels for each triage level, and the chief complaint algorithms are known as emergency symptoms and signs for emergency care. Each emergency symptom and sign includes one or more chief complaints and is classified according to the International Statistical Classification of Diseases and Related Health Problems, 10th Revision, 2007 (ICD-10), and a logistic process is attached to each algorithm”
The authors state that the RETTS system cannot be directly compared to the ESI system used in much of the US but they believe that RETTS levels 3-5 roughly correspond to levels 4 and 5 in the Canadian Triage and Acuity Scale.
Berg LM, Ehrenberg A, Florin J, et al. Associations Between Crowding and Ten-Day Mortality Among Patients Allocated Lower Triage Acuity Levels Without Need of Acute Hospital Care on Departure From the Emergency Department Ann Emerg Med. 2019;74:345-356.
