Category: Pharmacology & Therapeutics
Keywords: status epilepticus (PubMed Search)
Posted: 3/3/2016 by Bryan Hayes, PharmD
(Updated: 3/5/2016)
Click here to contact Bryan Hayes, PharmD
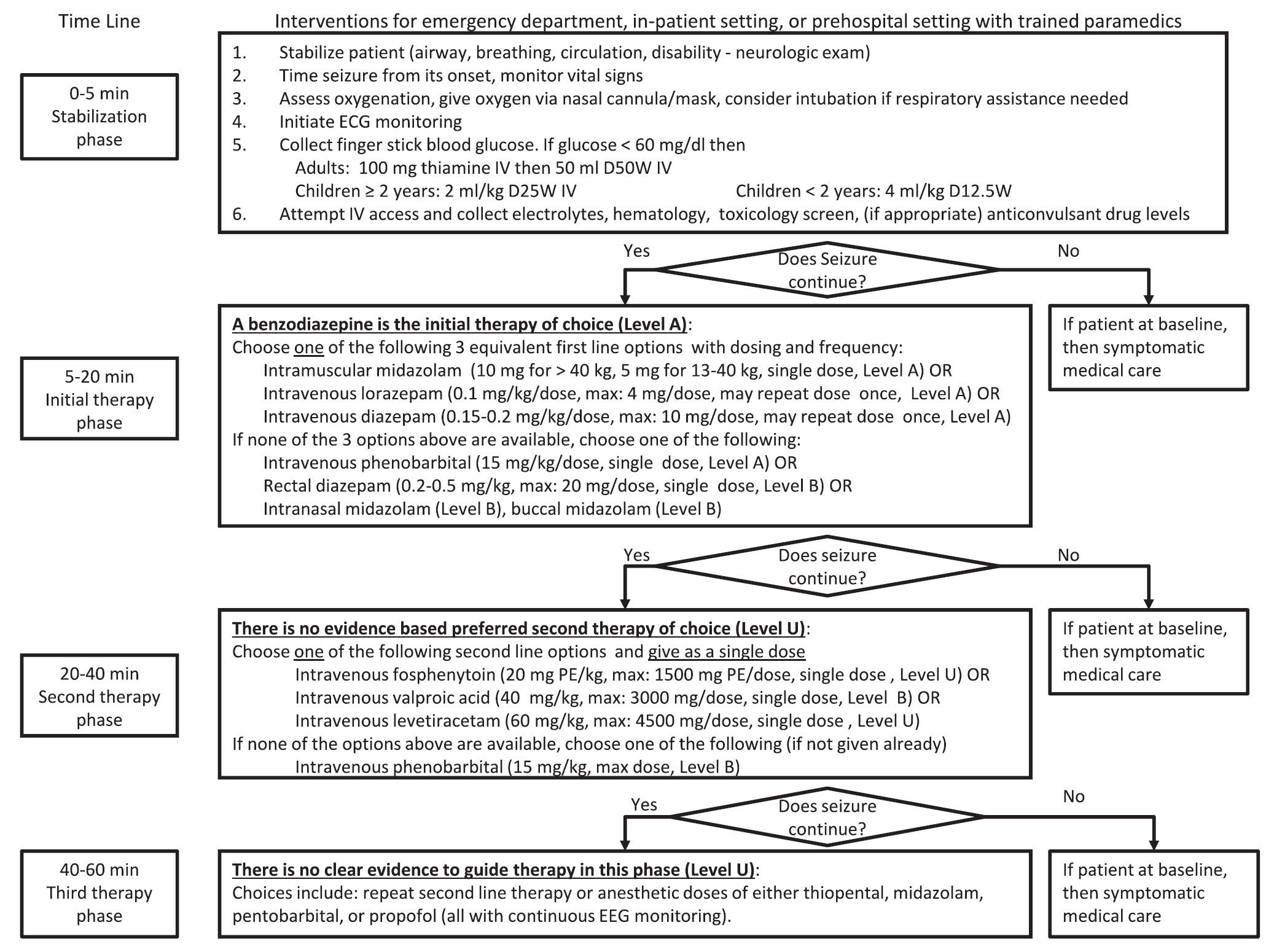
A new guideline for convulsive status epilepticus in adults AND children was recently published. [1] An insightful commentary was published alongside it (both are open access). [2] The proposed algorithm is below. Here are a few additional points to note:
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: succinylcholine, rocuronium, mortality, traumatic brain injury, RSI (PubMed Search)
Posted: 2/4/2016 by Bryan Hayes, PharmD
(Updated: 2/6/2016)
Click here to contact Bryan Hayes, PharmD
An interesting new study was published looking at in-hospital mortality in TBI patients who received succinylcholine or rocuronium for RSI in the ED.
What They Did
What They Found
Application to Clinical Practice
Patanwala AE, et al. Succinylcholine is associated with increased mortality when used for rapid sequence intubation of severely brain injured patients in the emergency department. Pharmacotherapy 2016;36(1):57-63. [PMID 26799349]
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: sugammadex, rocuronium, NMBA, vecuronium (PubMed Search)
Posted: 12/29/2015 by Bryan Hayes, PharmD
(Updated: 1/2/2016)
Click here to contact Bryan Hayes, PharmD
After three failed attempts, the FDA finally granted approval for Merck's non-depolarizing neuromuscular blocker reversal agent sugammadex (Bridion). Though the product has been used in Europe and Asia for several years, hypersensitivity concerns led to the delayed approval in the U.S.
Important points
Application to Clinical Practice
The EM PharmD blog discusses sugammadex's approval in more detail.
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: tramadol, seizure (PubMed Search)
Posted: 12/3/2015 by Bryan Hayes, PharmD
(Updated: 7/6/2016)
Click here to contact Bryan Hayes, PharmD
Tramadol has a reputation for being a safe, non-opioid alternative to opioids. Nothing could be further from the truth. Several blogs have published about the dangers of tramadol:
But what about seizure risk? Previous studies have been unable to confirm an increased seizure risk with therapeutic doses of tramadol (Seizure Risk Associated with Tramadol Use from EM PharmD blog). However, a new study refutes that premise.
22% of first-seizure patients had recent tramadol use!
This was a retrospecitve study without laboratory confirmation of tramadol intake. Nevertheless, it behooves us not to think of tramadol as a safer alternative to opioids. It is an opioid after all, and it comes with significant adverse effects.
Asadi P, et al. Prevalence of Tramadol Consumption in First Seizure patients; a One-Year Cross-sectional Study. Emerg (Tehran) 2015;3(4):159-61. [PMID 26495407]
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: low back pain, opioids, naproxen, oxycodone, cyclobenzaprine (PubMed Search)
Posted: 10/21/2015 by Bryan Hayes, PharmD
(Updated: 11/7/2015)
Click here to contact Bryan Hayes, PharmD
If there weren't enough reasons to avoid opioids, here is another: opioids don't work for low back pain (LBP).
Objective
A well-done, double-blind, randomized controlled trial from JAMA set out to compare functional outcomes and pain at 1 week and 3 months after an ED visit for acute LBP among patients randomized to a 10-day course of (1) naproxen + placebo; (2) naproxen + cyclobenzaprine; or (3) naproxen + oxycodone/acetaminophen.
Intervention
Outcome
Neither oxycodone/acetaminophen nor cyclobenzaprine improved pain or functional outcomes at 1 week compared to placebo, and more adverse effects were noted.
Application to Clinical Practice
Among patients with acute, nontraumatic, nonradicular LBP presenting to the ED, avoid adding opioids or cyclobenzaprine to the standard NSAID therapy.
Friedman BW, et al. Naproxen with Cyclobenzaprine, Oxycodone/Aceaminophen, or Placebo for Treating Acute Low Back Pain: A Randomized Clinical Trial. JAMA 2015;314(15):1572-80.
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: targeted temperature management, drug (PubMed Search)
Posted: 9/27/2015 by Bryan Hayes, PharmD
(Updated: 10/3/2015)
Click here to contact Bryan Hayes, PharmD
An excellent new review article provides a detailed look at how the drugs we give are affected by targeted temperature management. Here is a helpful chart of drug alterations that have data in reduced body temperature states:
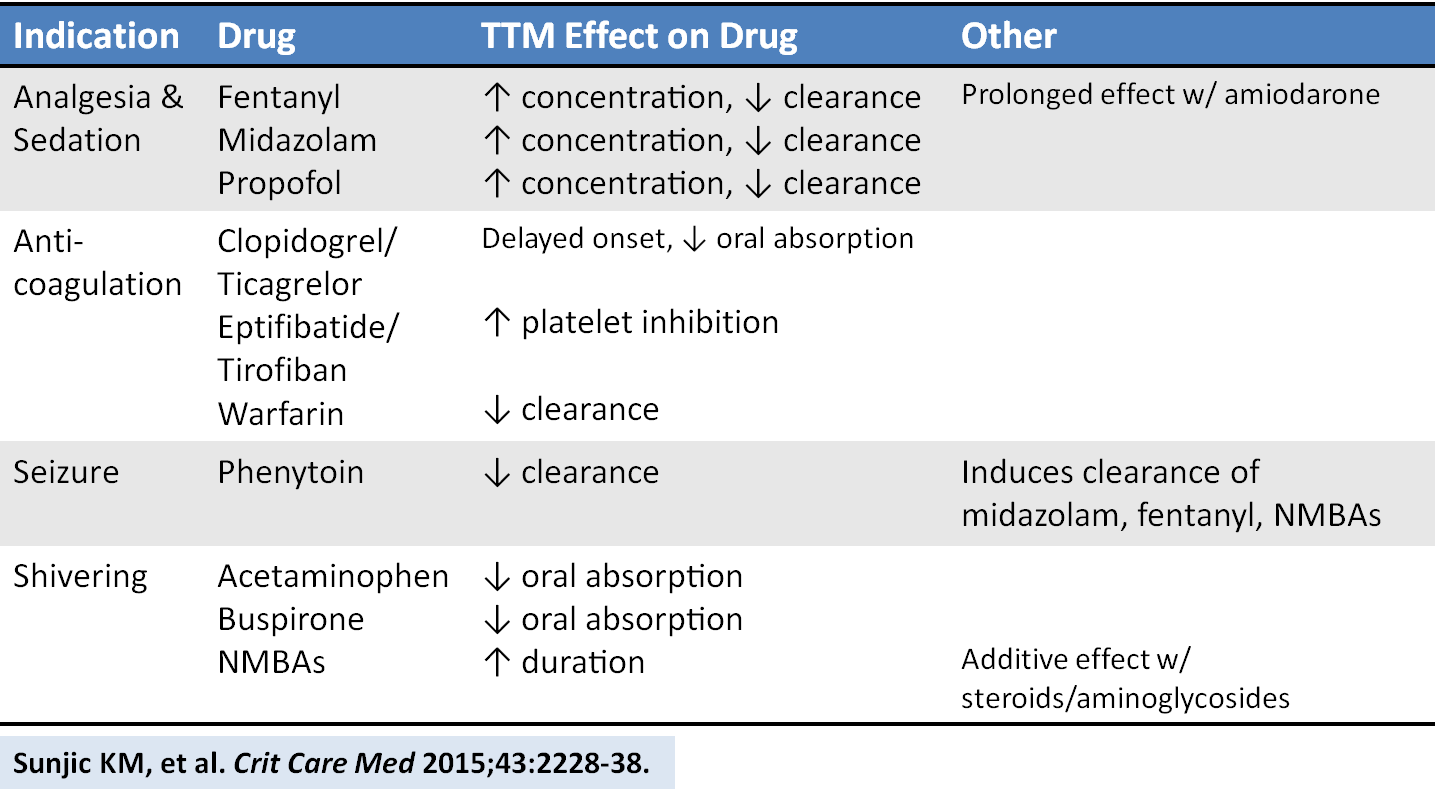
Sunjic KM, et al. Pharmacokinetic and other considerations for drug therapy during targeted temperature management. Crit Care Med 2015;43:2228-38. [PMID 26237312]
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: ketamine, analgesia, morphine, pain (PubMed Search)
Posted: 8/30/2015 by Bryan Hayes, PharmD
(Updated: 9/5/2015)
Click here to contact Bryan Hayes, PharmD
A new prospective, randomized, double-blind trial compared subdissociative ketamine to morphine for acute pain in the ED.
What they did
What they found
Motov S, et al. Intravenous subdissociative-dose ketamine versus morphine for analgesia in the emergency department: a randomized controlled trial. Ann Emerg Med 2015;66:222-9. [PMID 25817884]
Follow me on Twitter (@PharmERToxGuy)
Category: Pharmacology & Therapeutics
Keywords: blood glucose, dextrose, hypoglycemia (PubMed Search)
Posted: 7/26/2015 by Bryan Hayes, PharmD
(Updated: 8/1/2015)
Click here to contact Bryan Hayes, PharmD
How much does the blood glucose concentration increase when dextrose 50% (D50) is administered?
A new study found a median increase of 4 mg/dL (0.2 mmol/L) per gram of D50 administered.
This retrospective study was conducted in critically ill patients who experienced hypoglycemia while receiving an insulin infusion. While it may not directly apply to all Emergency Department patients, an estimation of the expected blood glucose increase from rescue dextrose is helpful. If the blood glucose doesn't respond as anticipated, it can help us troubleshoot possible issues (eg, line access).
Murthy MS, et al. Blood glucose response to rescue dextrose in hypoglycemic, critically ill patients receiving an insulin infusion. Ann Pharmacother 2015;49(8):892-6. [PMID 25986006]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: diabetic ketoacidosis, insulin, glargine, DKA (PubMed Search)
Posted: 6/29/2015 by Bryan Hayes, PharmD
(Updated: 7/4/2015)
Click here to contact Bryan Hayes, PharmD
Transitioning Diabetic Ketoacidosis (DKA) patients off an insulin infusion can be challenging. If a long-acting insulin, such as glargine or levemir, is not administered at the correct time to provide extended coverage, patients can revert back into DKA.
Pilot Study
A prospective, randomized, controlled pilot study in 40 patients evaluated administration of glargine within 2 hours of insulin infusion initiation compared to waiting until the anion gap (AG) had closed.
What they did
What they found
Mean time to closure of AG, mean hospital LOS, incidents of hypoglycemia, rates of ICU admission, and ICU LOS were all similar between the groups.
Application to Clinical Practice
Although just a pilot study (using a convenience sample), early glargine administration seemed to be absorbed adequately (based on time to AG closure) and was not associated with increased risk of hypoglycemia. If confirmed in a larger study, this technique could help optimize care of DKA patients in the ED by eliminating the often-mismanaged transition step later on.
Doshi P, et al. Prospective randomized trial of insulin glargine in acute management of diabetic ketoacidosis in the emergency department: a pilot study. Acad Emerg Med 2015;22(6):657-62. [PMID 26013711]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: obese, vancomycin, loading dose (PubMed Search)
Posted: 5/22/2015 by Bryan Hayes, PharmD
(Updated: 6/6/2015)
Click here to contact Bryan Hayes, PharmD
Vancomycin guidelines recommend an initial dose of 15-20 mg/kg based on actual body weight (25-30 mg/kg in critically ill patients). [1] The MRSA guidelines further recommend a max dose of 2 gm. [2]
But, what dose do you give for an obese patient that would require more than 2 gm?
A new study provides some answers to this question. [3] Obese-specific, divided-load dosing achieved trough concentrations of 10 to 20 g/mL for 89% of obese patients within 12 hours of initial dosing and 97% of obese patients within 24 hours of initial dosing.
Application to Clinical Practice
Caveats
The study used some more specific dosing calculations based on renal function and percentage above IBW. If patient's renal function is abnormal, consultation with a pharmacist is recommended.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: sodium, piperacillin/tazobactam, ampicillin, moxifloxacin, metronidazole (PubMed Search)
Posted: 4/13/2015 by Bryan Hayes, PharmD
(Updated: 5/2/2015)
Click here to contact Bryan Hayes, PharmD
Aside from sodium chloride and sodium bicarbonate, several commonly used emergency department medications (namely IV antibiotics) contain a significant amount of sodium. In patients with heart failure or other conditions requiring sodium restriction, judicious use should be considered.
Notes:
Ampicillin/sulbactam [package insert]. Metronidazole [package insert]. Moxifloxacin [package insert]. Nafcillin [package insert]. Piperacillin/tazobactam [package insert]. Ticarcillin/clavulanate [package insert].
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: clindamycin, SSTI, skin infection, Bactrim, trimethoprim-sulfamethoxazole (PubMed Search)
Posted: 3/20/2015 by Bryan Hayes, PharmD
(Updated: 4/4/2015)
Click here to contact Bryan Hayes, PharmD
For many institutions, clindamycin is not as good as it used to be for methicillin-resistant Staph aureus (MRSA). When treating skin and soft tissue infections (SSTI), this can be challenging. Clindamycin still covers skin strep species very well, but not always the staph. On the other hand, trimethoprim-sulfamethoxazole (TMP-SMX) covers staph really well, but not so much the strep.
What They Did
A new double-blind, multicenter, randomized study in NEJM compared these two antibiotics in 524 patients with uncomplicated skin infections who had cellulitis, abscess larger than 5 cm, or both. All abscesses underwent incision and drainage. The primary outcome was clinical cure rate 7-10 days after the end of treatment.
What They Found
There was no difference in clinical cure rate between the two groups (80.3% for clindamycin, 77.7% for TMP-SMX).
Problems with the Study
Application to Clinical Practice
Unknown. This study seems to suggest TMP-SMX might be ok in uncomplicated cellulitis even though we assume strep species are the causitive organism. However, we already know cephalexin is equivalent to cephalexin + TMP-SMX from the 2013 study by Pallin et al. Why not just use cephalexin which has less adverse effects than TMP-SMX?
With such low clindamycin resistance, even to the staph species, perhaps that is why the two treatments were similar. Also, why did successfully drained abscesses need antibiotics? Finally, there were many exclusion criteria which eliminated many of the patients we see in the ED.
For a different, critical perspective of this NEJM study, Dr. Ryan Radecki gives his thoughts on his EM Lit of Note blog.
Miller LG, et al. Clindamycin vs. Trimethoprim-Sulfamethoxazole for Uncomplicated Skin Infections. N Engl J Med 2015;372(12):1093-103. [PMID 25785967]
Pallin DJ, et al. Clinical Trial: Comparative Effectiveness of Cephalexin Plus Trimethoprim-Sulfamethoxazole Versus Cephalexin Alone for Treatment of Uncomplicated Cellulitis: A Randomized Controlled Trial. Clinical Infectious Diseases 2013;56(12):1754-62. [PMID 23457080]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: ketamine, pain, opioid (PubMed Search)
Posted: 2/24/2015 by Bryan Hayes, PharmD
(Updated: 3/7/2015)
Click here to contact Bryan Hayes, PharmD
Emergency Departments are increasingly searching for alternatives to opioids for acute pain management.
An urban trauma center in California retrospectively evaluated their use of low-dose ketamine for acute pain over a two-year period. [1]
Application to Clinical Practice
There was no comparison group and there was no mention of what other pain medicines were given. Adverse events are often under-reported in retrospective studies. This study seems to demonstrate that low-dose ketamine administration for acute pain management in the ED is feasible with a low rate of adverse effects.
It's worth noting that a new review of 4 randomized controlled trials evaluating subdissociative-dose ketamine found no convincing evidence to support or refute its use in the ED. The 4 included trials had methodologic limitations. [2]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: vancomycin, loading dose (PubMed Search)
Posted: 1/26/2015 by Bryan Hayes, PharmD
(Updated: 2/7/2015)
Click here to contact Bryan Hayes, PharmD
We know vancomycin should be dosed based on weight rather than the default 1 gm dose so many patients receive. A past Academic Life in EM post explores the nuances of proper vancomycin dosing. But do higher loading doses in the ED actually lead to more therapeutic trough levels?
New Data
A new randomized trial compared ED patients receiving 30 mg/kg initial doses vs. 15 mg/kg. [1] There was a significantly greater proportion of patients reaching target trough levels of 15 mg/L at 12 hours among the patients who received a 30 mg/kg loading dose as compared with a traditional 15 mg/kg dose (34% vs 3%, P < 0.01). This study did not use a max dose of 2 gm. They included patients up to 120 kg who received 3.6 gm loading doses! Patients with creatinine clearance < 50 mL/min were excluded. There was no difference in incidence of nephrotoxicity between the groups.
Application to Clinical Practice
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: headache, migraine, metoclopramide, magnesium (PubMed Search)
Posted: 12/31/2014 by Bryan Hayes, PharmD
(Updated: 1/3/2015)
Click here to contact Bryan Hayes, PharmD
Does IV magnesium have a role in the management of acute migraine headache in the ED? A new study says yes. [1]
Intervention
What They Found
Magnesium sulfate was more effective in decreasing pain severity at 20-min (pain scale 5.2 vs. 7.4) and 1-h (2.3 vs. 6.0) and 2-h (1.3 vs. 2.5) intervals after treatment (p < 0.0001) compared to treatment with dexamethasone/metoclopramide.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: antibiotic, IV, diarrhea (PubMed Search)
Posted: 11/25/2014 by Bryan Hayes, PharmD
(Updated: 12/6/2014)
Click here to contact Bryan Hayes, PharmD
Many of the oral antibiotics prescribed in the ED have good bioavailability. So, a one-time IV dose before discharge generally won't provide much benefit.
In fact, a new prospective study found that a one-time IV antibiotic dose before ED discharge was associated with higher rates of antibiotic-associated diarrhea and Clostridium difficile infection. [1] One-time doses of vancomycin for SSTI before ED discharge are also not recommended (see Academic Life in EM post).
Bottom Line
Though there are a few exceptions, if a patient has a working gut, an IV dose of antibiotics before ED discharge is generally not recommended and may cause increased adverse effects. An oral dose is just fine.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: penicillin, cephalosporin, allergy, cross-reactivity (PubMed Search)
Posted: 10/7/2014 by Bryan Hayes, PharmD
(Updated: 11/4/2014)
Click here to contact Bryan Hayes, PharmD
The cross-reactivity between cephalosporins and penicillins is significantly lower than the 10% figure many of us learned. In fact, the beta-lactam ring is rarely involved. So, when the warning pops up next time you order ceftriaxone in a penicillin-allergic patient, what should you do?
In a patient with a documented penicillin allergy, here is a simple chart to help determine when a cephalosporin is ok to use:
Common penicillins and cephalosporins with similar side chains include ampicillin/amoxicillin and cephalexin, cefaclor, cephadroxil, and cefprozil.
Campagna JD, et al. The use of cephalosporins in penicillin-allergic patients: a literature review. J Emerg Med 2012;42(5):612-20. [PMID 21742459]
Pichichero ME, et al. Penicillin and cephalosporin allergy. Ann Allergy Asthma Immunol 2014;112:404-12. [PMID 24767695]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: beta-lactam, piperacillin/tazobactam, critically ill (PubMed Search)
Posted: 9/27/2014 by Bryan Hayes, PharmD
(Updated: 10/4/2014)
Click here to contact Bryan Hayes, PharmD
Beta-lactam antimicrobials (penicillins, cephalosporins, and carbapenems) are frequently used for empiric and targeted therapy in critically ill patients. They display time-dependent killing, meaning the time the antibiotic concentration is above the minimin inhibitory concentration (MIC) is associated with improved efficacy.
Two new pharmacodynamic/pharmacokinetic studies suggest that current beta-lactam antimicrobial dosing regimens may be inadequate.
Antimicrobial dosing in critically ill patients is complex. Current dosing of beta-lactams may be inadequate and needs to be studied further with relation to clinical outcomes.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: HIV, Pre-Exposure Prophylaxis, PrEP (PubMed Search)
Posted: 8/30/2014 by Bryan Hayes, PharmD
(Updated: 9/6/2014)
Click here to contact Bryan Hayes, PharmD
In May 2014, the U.S. Public Health Service released the first comprehensive clinical practice guidelines for PrEP.
Pre-Exposure Prophylaxis (PrEP) has been shown to decrease the risk of HIV infection in people who are at high risk by up to 92%, if taken consistently.
How this applies to the ED patient:
For more information, the CDC has a comprehensive website dedicated to PrEP.
Centers for Disease Control and Prevention. (2014). Pre-Exposure Prophylaxis (PrEP). Retrieved from http://www.cdc.gov/hiv/prevention/research/prep/.
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
Category: Pharmacology & Therapeutics
Keywords: oseltamivir, critically ill, high-dose, influenza, Tamiflu (PubMed Search)
Posted: 7/28/2014 by Bryan Hayes, PharmD
(Updated: 8/2/2014)
Click here to contact Bryan Hayes, PharmD
Despite the lack of strong evidence to support the recommendation, the severity of the 2009 influenza pandemic prompted the World Health Organization (WHO) to advise that higher doses of oseltamivir (150 mg twice daily) and longer treatment regimens (> 5 days) should be considered when treating severe or progressive illness.
So, does the data support higher dosing in critically ill influenza patients?
A new systematic review concluded that "the small body of literature available in humans does not support routine use of high-dose oseltamivir in critically ill patients."
Flannery AH, et al. Oseltamivir dosing in critically ill patients with severe influenza. Ann Pharmacother 2014;48(8):1011-8. [PMID 24816209]
Follow me on Twitter (@PharmERToxGuy) or Google Plus (+bryanhayes13)
