Category: Orthopedics
Posted: 3/23/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
The OPAL trial attempted to investigate the effectiveness of opioids in the acute management of neck and back pain.
346 adults presenting to the Emergency department or primary care provider with 12 weeks or less of lower back pain, neck pain or both (of at least moderate intensity).
51% male. 49% female.
Location: Sydney, Australia
All participants received guideline care (advice to stay active, reassurance of a positive prognosis, avoidance of bed rest, and, if required, other non-opioid analgesics).
Patients were then randomly assigned to an opioid (oxycodone, up to 20 mg PO qD) or and an identical placebo, for up to 6 weeks*.
*Trial used a combination oxycodone/naloxone to reduce risk of opioid induced constipation and assist with blinding.
*Trial used a modified release formulation that could be dosed q12h rather than q4-6h to increase adherence.
*Recommended regimen was oxycodone 5mg every 12 hours, with titration as necessary, max dose 20mg total per day.
*Trial physicians were able to individualize the prescription to suit the patient’s needs.
* Mean prescribed dose was approx. oxycodone 10mg total daily.
*Most patients only treated for 2 weeks
Primary outcome: Pain severity at 6 weeks
Results: Mean pain score at 6 weeks was identical between groups.
Trend towards faster recovery in the placebo group in the first 2 weeks.
Take home: Consider the likely benefit vs harm of prescribing opioids for acute back and neck pain in the ED.
Friedman BW, Irizarry E, Chertoff A, Feliciano C, Solorzano C, Zias E, Gallagher EJ. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department-based Randomized Study. Acad Emerg Med. 2020 Mar;27(3):229-235.
Category: Orthopedics
Posted: 3/8/2024 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Acetaminophen and low back pain.
Acetaminophen has been a traditionally recommended first line intervention for acute low back pain.
Cochrane reviews in 2016 and 2023 found that acetaminophen showed no benefit compared to placebo in patients with acute low back pain.
A 2020 study investigated whether the addition of acetaminophen to short term NSAID therapy was beneficial.
A randomized double-blind study conducted in two urban emergency departments.
Patients randomized to a 1-week course of ibuprofen plus acetaminophen versus ibuprofen plus placebo.
Population: patients presenting with acute, non-radicular, non-traumatic lower back pain of fewer than two weeks duration.
Authors compared pain and functional outcomes at one week following discharge.
Conclusion: there was no outcome benefit from the addition of acetaminophen to ibuprofen.
Friedman BW, et al. Ibuprofen Plus Acetaminophen Versus Ibuprofen Alone for Acute Low Back Pain: An Emergency Department-based Randomized Study. Acad Emerg Med. 2020 Mar;27(3):229-235.
Category: Orthopedics
Keywords: neck pain, radiculopathy (PubMed Search)
Posted: 2/24/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Axial neck pain is a dull aching “soreness” pain from the posterior neck muscles with radiation to the occiput, periscapular and shoulder regions.
Associated with headaches, stiffness and muscle spasm.
Patients with cervical radiculopathy, however, usually present with unilateral pain discomfort.
Patients may complain of pain radiation into the ipsilateral arm. Though frequently difficult to describe, this may be in a dermatomal distribution. Patients may also report decreased sensation in a dermatomal distribution or weakness along the corresponding myotome.
The most affected nerve roots are C7 (C6-7 herniation), followed by C6 (C5-6 herniation) and C8 (C7-T1 herniation).
Cervical Spondylosis (degenerative change) is the most common ideology.
As discs breakdown with age and lose height, increased force loads are transmitted to bony regions of the spinal segment leading to bone hypertrophy which creates foraminal stenosis and resultant radiculopathy.
Cervical radiculopathy, like lumbar radiculopathy, is largely a self-limited condition. Several older studies following this diagnosis revealed that a majority of patients were either asymptomatic or mildly symptomatic at time of follow-up.
Improvement is seen over the initial four to six months following diagnosis.
Category: Orthopedics
Posted: 1/27/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: a cluster randomised controlled trial
Intro: Musculoskeletal injuries and concussion are prominent reasons for time loss from sport for adolescent rugby players.
Injury patterns in rugby differ from other team sports,
-Greater frequency of concussion, upper body and contact-related injuries
Increased concussion risk is associated with lower neck strength, highlighting this characteristic as a potentially modifiable risk factor.
Enhancing neck muscle strength may prevent concussion by improving the dissipation of impact forces transmitted to the brain.
The aim of study was to determine the efficacy of a movement control exercise program in reducing injuries in youth rugby players.
Methods: In a cluster-randomized controlled trial, 40 independent schools (118 teams, 3188 players aged 14-18 years) were allocated to receive either the intervention or a reference program, both of which were to be delivered by school coaches.
The intervention comprised balance training, whole-body resistance training, plyometric training, and controlled rehearsal of landing and cutting maneuvers. This also included a neck strengthening component.
Time-loss (>24 hours) injuries arising from school rugby matches were recorded by coaches and medical staff.
Results: When trial arm comparisons were limited to teams who had completed three or more weekly program sessions on average, clear reductions in overall match injury incidence (RR=0.28) and concussion incidence (RR=0.41) were noted in the intervention group.
Conclusion:
Hislop MD, et al. Reducing musculoskeletal injury and concussion risk in schoolboy rugby players with a pre-activity movement control exercise programme: a cluster randomised controlled trial. Br J Sports Med. 2017 Aug;51(15):1140-1146.
Category: Orthopedics
Posted: 1/13/2024 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Wrist pain in golfers
70% of amateur golfers will experience a sport related injury in their lifetime.
The hand/wrist is the third most common body area injured by golfers after the back and elbow.
Studies fail to include multi trauma from golf cart accidents:)
Wrist injuries are 3x more frequent than hand injuries.
Wrist injury affects 13 to 20 percent of amateur golfers.
Injury is most likely to occur at the point of ball impact.
Injury most commonly affects the lead wrist rather than the trail wrist.
The lead wrist is left sided for right-handed players and right sided for lefties
Due to many differences in grip and wrist position there are several injury patterns.
Most causes of wrist pain in golfers are tendinopathies.
Due to impact stress and repetitive swinging movements
If pain is primarily radial, consider DeQuervain's tenosynovitis
Poor swing mechanics such as premature wrist uncocking in the early downswing places the wrist in ulnar deviation thereby stressing the first dorsal compartment.
Significant ulnar deviation of the lead wrist at time of ball impact may also stress the tendons of the first dorsal compartment.
If pain is primarily ulnar consider Extensor Carpi Ulnaris tendonitis & subluxation
A strong golf grip (more knuckle’s visible) is associated with greater ECU stress during the swing
The height of hand position can also stress the ECU tendon
Differential diagnosis:
TFCC injury
Hook of hamate fracture
Carpal Tunnel Syndrome
Ulnar Tunnel Syndrome
Category: Orthopedics
Posted: 12/23/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Estimating the size of knee effusions
While this size range is typically easily detectable on exam. This may not apply to patients who are either very muscular or obese.
If the detection of a small to moderate sized effusion would change patient management
Consider ultrasound:
As compared to MRI (sensitivity of 81.3 % and a specificity of 100 %)
Draghi F, Urciuoli L, Alessandrino F, Corti R, Scudeller L, Grassi R. Joint effusion of the knee: potentialities and limitations of ultrasonography. J Ultrasound. 2015 Sep 18;18(4):361-71.
Category: Orthopedics
Keywords: foot injury (PubMed Search)
Posted: 11/25/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
The fleck sign of the foot is a small bony fragment seen in the Lisfranc joint space.
The space between the bases of the first and second metatarsal
This finding is associated with an avulsion of the Lisfranc ligament
Lisfranc Injuries
Category: Orthopedics
Posted: 11/11/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
https://prod-images-static.radiopaedia.org/images/626179/d58f35a8aa4a0a6750a6adce4087a4_gallery.jpg
"I was kicked in the inside of my knee while it was straight (extended). Look at the x-ray and tell me if its bad"
The arcuate sign
Avulsion fracture of the styloid of the proximal fibula. The fragment is usually small (less than 1 cm) and displaced superiorly and medially. This fracture pattern is pathognomonic for posterolateral corner (PLC) injury.
Treatment in ED is knee immobilization in full extension. Refer to orthopedics for PCL reconstruction.
Category: Orthopedics
Keywords: Race day event, medical tent, endurance athlete (PubMed Search)
Posted: 10/28/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
The objective of a recent study was to analyze the injury and illness characteristics in Iron Man distance triathletes. This information is important for emergency providers who may be asked to directly assist or help coordinate race day medical care.
Intro: The Iron Man distance triathlon is one of the most challenging ultra endurance competitions in the world. 80,000 Iron Man triathletes compete internationally each year to qualify for the Ironman world championship. The race totals 140.6 miles across three legs, beginning with a 2.4 mile swim, followed by a 112 mile cycle, and is completed with a 26.2 mile run.
Retrospective cross-sectional study of medical records from Iron Man distance championship races across a 30-year period (1989-2019). The study population (10,533) consisted of all triathletes treated at mobile medical units along the race route or who presented to the medical tent for evaluation during and immediately after the event.
Mean population age of 37 with a range of 18 to 87 years.
Results: Female athletes were found to present to the medical tent more than males (P < 0.001).
The total incidence of medical encounters by age was found to be higher in both younger athletes (18 to 34 years old) and older athletes (greater than 70 years old) versus middle-aged athletes (35-69 years old) (P < 0.001).
Professional athletes have similar overall medical encounters compared with other athletes.
The busiest hours of the medical tent were between approximately 9 and 14 hours after start time (afternoon and early evening) in which approximately 73% of athletes presented for evaluation and treatment.
Once inside the medical tent 71% of athletes were discharged within an hour and 87% were discharged within 1.5 hours. Athletes were dispatched to the hospital from the medical tent area at a rate of 17.1/1000 athletes (most athletes presenting to the medical tent finished the race and few required hospital transfer).
The most common medical complaints were dehydration and nausea followed by dizziness, exhaustion, muscle cramps, and vomiting.
Blood work was collected for 30% of athletes who entered the medical tent. Of these athletes, hyponatremia was the most prevalent diagnosis and most of whom were symptomatic with symptoms such as confusion, stupor, gait disturbance, muscle weakness, headache, dizziness, fatigue, nausea and vomiting.
Beyond basic medical care, intravenous fluids were the most common medical treatment.
Conclusion: Medical events were more frequent among female athletes as well as both younger and older age categories. Gastrointestinal and exertional related symptoms were the most common complaints in the medical tent. Besides basic medical care, IV infusions were the most common treatment. Most athletes presenting to the medical tent finished the race and only a small percentage were transferred to the hospital.
Nilssen PK, Connolly CP, Johnson KB, Cho SP, Cohoe BH, Miller TK, Laird RH, Sallis RE, Hiller WDB. Medical Encounters and Treatment Outcomes in Ironman-Distance Triathlon. Med Sci Sports Exerc. 2023 Nov 1;55(11):1968-1976.
Nilssen PK, Connolly CP, Johnson KB, Cho SP, Cohoe BH, Miller TK, Laird RH, Sallis RE, Hiller WDB. Medical Encounters and Treatment Outcomes in Ironman-Distance Triathlon. Med Sci Sports Exerc. 2023 Nov 1;55(11):1968-1976.
Category: Orthopedics
Keywords: asthma, reactive airway disease, lung function (PubMed Search)
Posted: 9/24/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
The role of exercise in patients with asthma is complicated.
Asthma symptoms can worsen or be triggered by physical activity. This can lead to avoidance response. Patients with asthma are less physically active than their matched controls.
Recently, however, the role of exercise and physical activity as an adjunct therapy for asthma management has received considerable attention. There is an emerging and promising role of physical activity as a non-pharmacologic treatment for asthma. Exercise reduces inflammatory cytokines and increases anti-inflammatory cytokines thereby reducing chronic airway inflammation.
Physical activity can help improve lung function and boost quality of life. As fitness improves, asthma patients report better sleep, reduced stress, improved weight control, and more days without symptoms.
The Global Initiative for Asthma recommends twice-weekly cardio and strength training. Strength training requires short periods of exertion allowing for periods of rest and recovery. High-intensity interval training (HIIT) is a promising option for people with asthma. These types of workouts allow ventilation to recover intermittently vs conventional cardio exercises.
A 2021 study in adults with mild-to-moderate asthma found that low volume HIIT classes (three 20-minute bouts/week) significantly improved asthma control. Patients also had improved exertional dyspnea and enjoyment of exercise which will, in turn, increase the odds of further exercise.
A 2022 study compared constant-load exercise versus HIIT in adults with moderate-to-severe asthma. Exercise training lasted 12 weeks (twice/week, 40 minutes/session). Both groups showed similar improvements in aerobic fitness however the HIIT group reported lower dyspnea and fatigue perception scores and higher physical activity levels.
Conclusion: Patients with asthma should be encouraged to safely incorporate exercise in their daily lives bother for overall health benefits but also as an effective non-pharmacologic asthma treatment.
1. O'Neill C, Dogra S. Low volume high intensity interval training leads to improved asthma control in adults. J Asthma. 2021 Sep;58(9):1256-1260.
2. Aparecido da Silva R, Leite Rocco PG, Stelmach R, Mara da Silva Oliveira L, Sato MN, Cukier A, Carvalho CRF. Constant-Load Exercise Versus High-Intensity Interval Training on Aerobic Fitness in Moderate-to-Severe Asthma: A Randomized Controlled Trial. J Allergy Clin Immunol Pract. 2022 Oct;10(10):2596-2604
Category: Orthopedics
Keywords: concussion, sports, head injury (PubMed Search)
Posted: 9/10/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Sport related concussion has been estimated to affect almost 2 million children and adolescents in the United states annually
Patients who take longer than four weeks to recover are considered to have persistent post concussive symptoms
This diagnosis is associated with poor educational, social and developmental outcomes in pediatric patients
Following sport related concussion, patients are recommended to have an individualized aerobic exercise program
Prior studies have found that sub symptom threshold aerobic exercise safely and significantly speeds recovery from sport related concussion.
Purpose: This study attempted to answer whether there is a direct relationship between adherence to a personalized exercise prescription and recovery or if initial symptom burden effects adherence to the prescription.
Design: Male and female adolescents aged 13 to 18 years old presenting within 10 days of injury and diagnosed with sport related concussion.
Almost all participants (94%) sustained concussion during interscholastic games or practices.
As it is known that physician encouragement can influence patient adherence to medical interventions, treating physicians in the study were blinded to study arm assignment.
Patients were given aerobic exercise prescriptions based on their heart rate threshold at the point of exercise intolerance on a graded treadmill test
Adherence to prescription was determined objectively with heart rate monitors. No participants exercised above their prescribed heart rate intensity.
Patients who completed at least 2/3 of their aerobic exercise prescription were considered to be adherent
Results: 61% of adolescents met the adherence criterion
Adherent patients were more symptomatic and were more exercise intolerant (worse initial exercise tolerance) at their initial visit.
These patients were also more adherent than those with fewer symptoms and with better exercise tolerance. This likely indicates a stronger motivation for those more symptomatic patients to engage in a potentially effective intervention.
Adherent patients recovered faster than those who were not adherent (median recovery time 12 days versus 21.5 days (P = 0.016)
Adherence during week one was inversely related to recovery time and to initial exercise tolerance but not to initial symptom severity
Conclusion: Adherence to individualized sub symptom threshold aerobic exercise within the first week of sport related concussion is associated with faster recovery. The initial degree of exercise intolerance (but not initial symptom severity) affects adherence to aerobic exercise prescription in an adolescent population with sport related concussion
Chizuk HM, et al. Adolescents with Sport-Related Concussion Who Adhere to Aerobic Exercise Prescriptions Recover Faster. Med Sci Sports Exerc. 2022 Sep 1;54(9):1410-1416.
Category: Orthopedics
Keywords: elbow, UCL, throwing injury (PubMed Search)
Posted: 8/26/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
29 yo baseball pitcher presents with right medial elbow pain. He felt a painful “pop” and could not continue to throw (due to loss of speed and control). Also notes mild paresthesias in 4th and 5th digits.
Ulnar collateral ligament (UCL) injury
Sprain of the UCL of the elbow can occur either as an acute injury or as the result of chronic excessive valgus stress due to throwing. This injury is seen in javelin throwers and baseball pitchers. Most recently, Angels superstar Shohei Ohtani suffered a torn UCL.
While traditionally this injury pattern was thought to occur in older, high-level pitchers (high velocity throwing), we are increasingly seeing this in younger athletes.
The repeated valgus stress of pitching leads to micro tearing and inflammation of the ligament. Over time, this leads to scarring and calcification and then ligament rupture.
This injury is more likely to happen in pitchers who “open up too soon” in their throwing motion. Fatigue related changes seen first in leg and core mechanics cause pitchers to open up earlier, increasing stress to the shoulder and the UCL of the elbow. Other risk factors include high velocity pitching, insufficient recovery time, and chronic overuse. The importance of proper pitching mechanics is very important as players whose pitching motion produces greater elbow valgus loads and shoulder external rotation torque are at increased risk for UCL tears.
Approximately one half of the torque generated during a fastball pitch is transmitted to the UCL. Well developed muscles about the elbow can dissipate enough energy that acute tearing is rare.
The athlete with a UCL sprain will complain of medial elbow pain that increases during the acceleration phase of throwing.
On examination, there is localized tenderness directly over the UCL:
http://www.texasshouldersurgeon.com/uploads/6/3/5/8/63580047/1446137856.png
Stress testing of the UCL causes both pain and demonstrates laxity.
Moving Valgus Stress Test:
Place elbow in the “90/90” position. Apply a valgus stress while ranging elbow through full arc of flexion and extension. A positive test will reproduce apprehension, pain or instability at the UCL origin between 70 and 120 degrees.
https://www.youtube.com/watch?v=OnkkHpG3Dqg&ab_channel=RussHoff
Category: Orthopedics
Keywords: Ortho, bohler angle, fracture. (PubMed Search)
Posted: 7/27/2023 by Robert Flint, MD
Click here to contact Robert Flint, MD
"The normal value for the Böhler angle is between 25° and 40° 1. Although there is wide variation between individuals, there is relatively little variation between the left and right feet of a single individual 2. A reduced Böhler angle can be seen in displaced intra-articular calcaneal fractures. The degree of reduction in the Böhler angle is an indicator of the severity of calcaneal injury, and the degree to which the Böhler angle is restored at surgery is correlated with functional outcome 3."
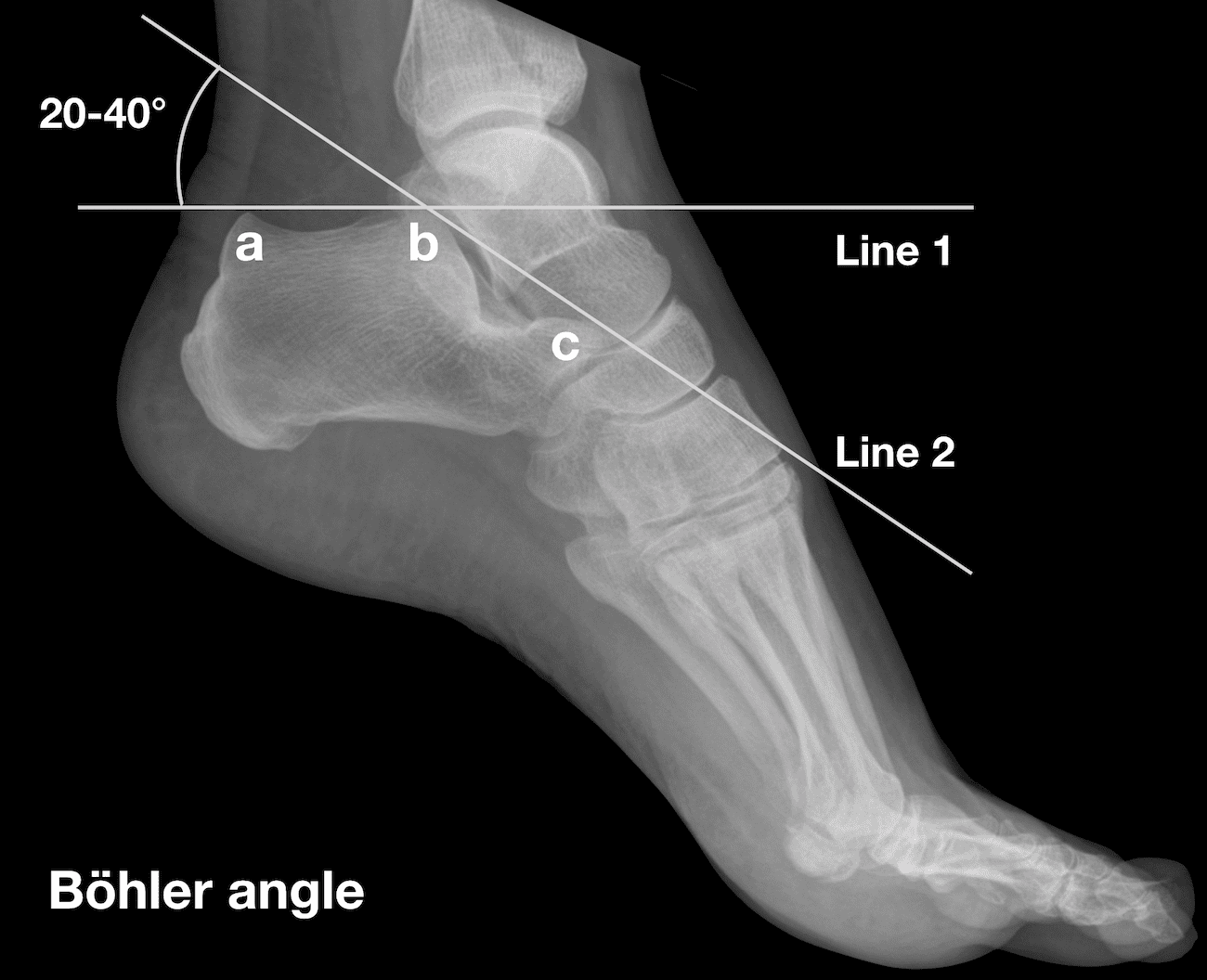
Amini B, Worsley C, Weerakkody Y, et al. Böhler angle. Reference article, Radiopaedia.org (Accessed on 27 Jul 2023) https://doi.org/10.53347/rID-1002
Category: Orthopedics
Keywords: shoulder pain, labrum tear (PubMed Search)
Posted: 7/22/2023 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
SLAP tear/lesion – Superior labral tear oriented anterior to posterior
Glenoid labrum – A rim of fibrocartilaginous tissue surrounding the glenoid rim, deepening the “socket” joint.
Integral to shoulder stability.
https://aosm.in/storage/2019/05/ch-shoulder-slap.jpg
O’Brien’s test aka active compression test for superior labral pathology.
2 parts – generally performed with the patient standing.
The patient’s shoulder is raised to 90 degrees with full elbow extension and approximately 30 degrees of adduction across the midline.
Resistance is applied, using an isometric hold.
Test in both full internal and external rotation
-This alters the position and rotation of the humerus against the glenoid
A positive test is when pain is elicited when the shoulder is in internal rotation with forearm pronation (thumb to floor) and much less or no pain when in external rotation (supination).
Note: AC joint pain may test similarly but will localize to different area of shoulder
The presence of similar, reproducible deep and diffuse glenohumeral joint pain is most indicative of a true positive test.
https://i0.wp.com/musculoskeletalkey.com/wp-content/uploads/2020/03/f50-02-9780323287845.jpg?w=960
Category: Orthopedics
Keywords: blurry vision, head trauma (PubMed Search)
Posted: 7/8/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Multiple vision disorders may occur after concussion including injury to the systems that control binocular vision including: Convergence insufficiency and Accommodation insufficiency
In order to obtain a single binocular vision, simultaneous movement of both eyes in opposite directions is required.
To look at an object close by such as when reading, the eyes must rotate towards each other (convergence).
Convergence insufficiency is the reduced ability to converge enough for near vision and is a common visual dysfunction seen after concussion.
One of both eyes may also turn outward.
May lead to complaints with reading such as diplopia, blurry vision, eyestrain, and skipping words or losing one's place.
Patient or parent may also report other difficulties such as becoming more easily fatigued when reading, needing to squint and/or having disinterest in reading.
Take home: consider testing convergence in patients with some of these complaints in setting of acute or subacute head trauma.
Master CL, Bacal D, Grady MF, Hertle R, Shah AS, Strominger M, Whitecross S, Bradford GE, Lum F, Donahue SP; AAP SECTION ON OPHTHALMOLOGY; AMERICAN ACADEMY OF OPHTHALMOLOGY; AMERICAN ASSOCIATION FOR PEDIATRIC OPHTHALMOLOGY AND STRABISMUS; and AMERICAN ASSOCIATION OF CERTIFIED ORTHOPTISTS. Vision and Concussion: Symptoms, Signs, Evaluation, and Treatment. Pediatrics. 2022 Aug 1;150(2):e2021056047.
Category: Orthopedics
Keywords: POCUS, Hip Fractures, Nerve Blocks, Administration (PubMed Search)
Posted: 6/26/2023 by Alexis Salerno Rubeling, MD
(Updated: 2/8/2026)
Click here to contact Alexis Salerno Rubeling, MD
The use of a fascia iliaca compartment block has been shown to reduce pain, decrease length of stay and decrease the opiate requirements for patients with hip fractures.
Check out this page on how to perform this procedure.
Fascia iliac blocks can be challenging to implement routinely in the emergency department. Studies show that 2.5% of eligible patients, despite departmental implementation, receive a block.
One recently published article showed that large scale multi-disciplinary implementation can increase the use of fascia iliac blocks. After implementation, the study team found that 54% of eligible patients received a fascia iliac block.
This article is interesting as it provides helpful resources including physician and nursing protocols for performing this block.
Downs T, Jacquet J, Disch J, Kolodychuk N, Talmage L, Krizo J, Simon EL, Meehan A, Stenberg R. Large-scale Implementation of Fascia Iliaca Compartment Blocks in an Emergency Department. West J Emerg Med. 2023 May 3;24(3):384-389. doi: 10.5811/westjem.58793. PMID: 37278790; PMCID: PMC10284502.
Category: Orthopedics
Keywords: shoulder, Adhesive capsulitis (PubMed Search)
Posted: 6/10/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Adhesive capsulitis aka frozen shoulder
Definition: Gradual development of global limitation of both active and passive shoulder motion, characterized by severe pain and lack of radiographic findings
Idiopathic loss of BOTH active and passive motion (significant reduction of at least 50%)
Motion is stiff and painful especially at the extremes.
Occurs due to thickening and contracture of the shoulder capsule.
Affects up to 8-10% of people of working age.
Affects patients between the ages of 40 and 60.
Peak age mid 50s
Onset before 40 is rare (consider other diagnosis).
Affects women more than men.
Diabetes is the most common risk factor.
Patients with DM, suffer a more prolonged course and are more resistant to therapy
Also associated with thyroid disease and prolonged immobilization
Increased risk following trauma to shoulder region (rotator cuff tear, following shoulder surgery, fracture of proximal humerus)
Presents unilaterally (other shoulder may become involved in next 5 years)
Slight increased risk of non-dominant shoulder
Category: Orthopedics
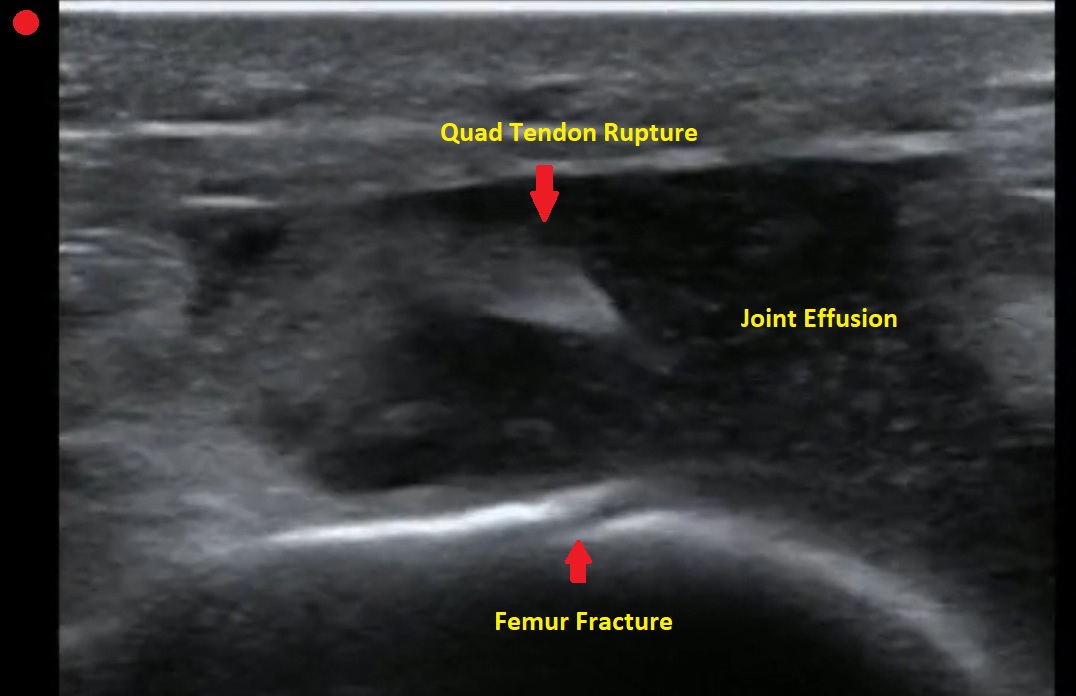
Keywords: POCUS, Knee Pain, Tendon Rupture (PubMed Search)
Posted: 6/5/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Pt presents to the emergency department with knee pain.
You decide to ultrasound the proximal knee. You place your ultrasound probe in the midline of the knee with your probe marker towards the patient's head.
What is the diagnosis?
-
--
---
--
-
The answer is a quadriceps tendon rupture with femur fracture.
Category: Orthopedics
Keywords: overuse injury, wrist (PubMed Search)
Posted: 5/25/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Intersection syndrome
Intersection syndrome is an overuse injury of the forearm.
Pain is located approximately 2 finger breaths (4cm) proximal to the wrist joint.
https://www.sportsmedreview.com/wp-content/uploads/2020/11/intersectionsyndrome.png
Mechanism: friction is caused by repetitive wrist extension activities
Commonly: Rowing, skiing, tennis, canoeing and weightlifting
Friction may cause crepitus with finger/wrist extension.
Tenderness, mild swelling may be present
Category: Orthopedics
Keywords: Baker's cyst, knee, effusion (PubMed Search)
Posted: 5/13/2023 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
A Baker's cyst is a common incidental finding on ultrasound reports and bedside physical exam.
Clinically, these cysts are commonly found in association with intra-articular knee disorders. Most commonly: osteoarthritis, RA and tears of the meniscus.
Sometimes Baker's cysts are a source of posterior knee pain.
In an orthopedic clinic setting, Baker’s cysts are frequently discovered on routine MRI in patients with symptomatic knee pain. They tend to occur in adults from ages 35 to 70.
Over 90% of Baker’s cysts are associated with an intraarticular knee disorder. While most frequently associated with OA and meniscal tears, other knee pathologies that have been associated include inflammatory arthritis and tears of the anterior cruciate ligament.
DDX: DVT, cystic masses (synovial cyst), solid masses (sarcoma) and popliteal artery aneurysms.
Based on cadaveric studies, a valvular opening of the posterior capsule, proximal/medial and deep to the medial head of the gastrocnemius is present in approximately 50% of healthy adult knees.
Fluid flows in one way from knee joint to cyst and not in reverse. This valve allows flow only during knee flexion as it is compressed shut during extension due to muscle tension.
Most common patient complaint is that of the primary pathology, meniscal pain for example. At times, symptoms related to the cyst are likely due to increasing size as they may report fullness, achiness, stiffness.
In one small study, the most common symptoms were 1) popliteal swelling and 2) posterior aching. Patients may complain of loss of knee flexion from an enlarged cyst that can mechanically block full flexion.
If the Baker cyst is large enough the clinician will feel posterior medial fullness and mild tenderness to palpation. The cyst will be firm and full knee extension and softer during the flexion (Foucher’s sign).
This may help with differentiation from other popliteal masses (hematoma, soft tissue tumor, popliteal artery aneurysm).
With cyst rupture, severe pain can simulate thrombosis or calf muscle rupture, (warmth, tenderness, and erythema). A ruptured cyst can also produce bruising, which may involve the posterior calf starting from the popliteal fossa and extending distally towards the ankle.
Treatment: initial treatment for symptomatic Baker cysts is nonoperative unless vascular or neural compression is present (very unlikely)
Treatment involves physical therapy to maintain knee flexibility. A sports medicine physician may perform an intraarticular knee corticosteroid injection as this has been found to decrease size and symptoms of cysts in two-thirds of patients.
For patients that fail above, refer for surgical evaluation. Inform patients that they are not undergoing ED drainage of this symptomatic cyst due to the extremely high rate of recurrence which, as a result of the ongoing presence of the untreated intraarticular pathology, results in the recurrent effusion.
