Category: Trauma
Keywords: trauma, hyperopia, oxygen, length of stay (PubMed Search)
Posted: 8/29/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This retrospective study of Swiss trauma patients looked at blood gas oxygen levels within 3 hours of arrival to the trauma bay in severely injured patients over age 16. When comparing hypoxic, hyperoxic and normo-oxic patients there was no difference in 28 day mortality. Those with above normal oxygen levels tended toward longer hospital stays. The above normal oxygen cohort also were more likely to be intubated in the field.
This study fits with others showing around 20% of trauma patients arrive to our trauma bays over oxygenated. More research is needed to see the impact this has on care. Be mindful of over oxygenation especially in intubated trauma patients.
Iten, M., Pietsch, U., Knapp, J. et al. Hyperoxaemia in acute trauma is common and associated with a longer hospital stay: a multicentre retrospective cohort study. Scand J Trauma Resusc Emerg Med 32, 75 (2024). https://doi.org/10.1186/s13049-024-01247-5
Category: Trauma
Keywords: Head injury, decision tools (PubMed Search)
Posted: 8/18/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
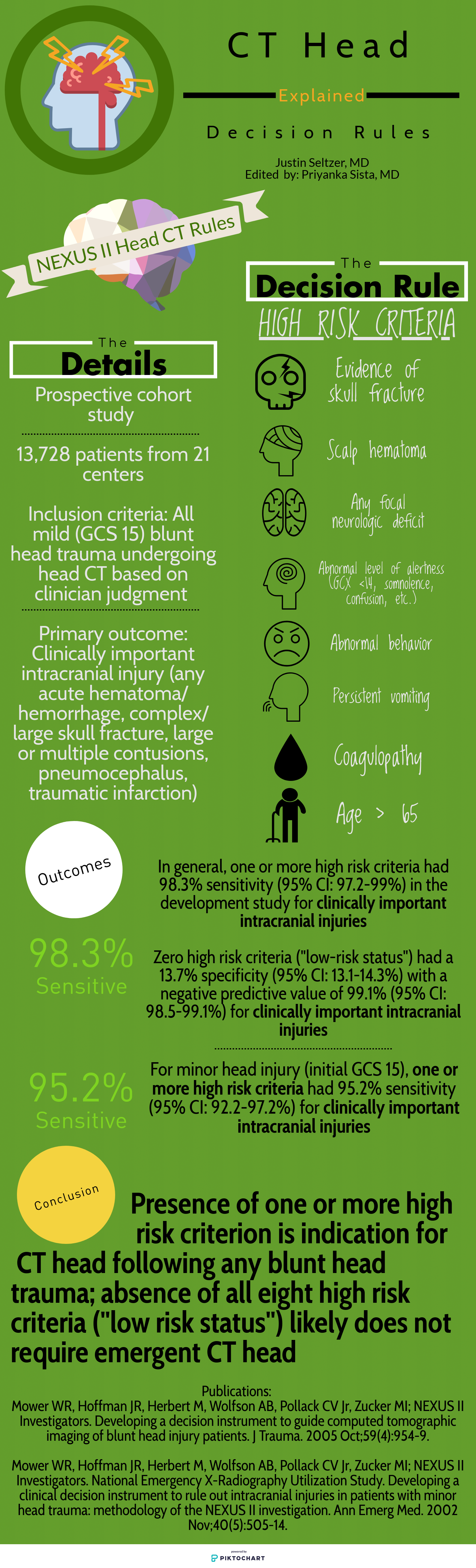
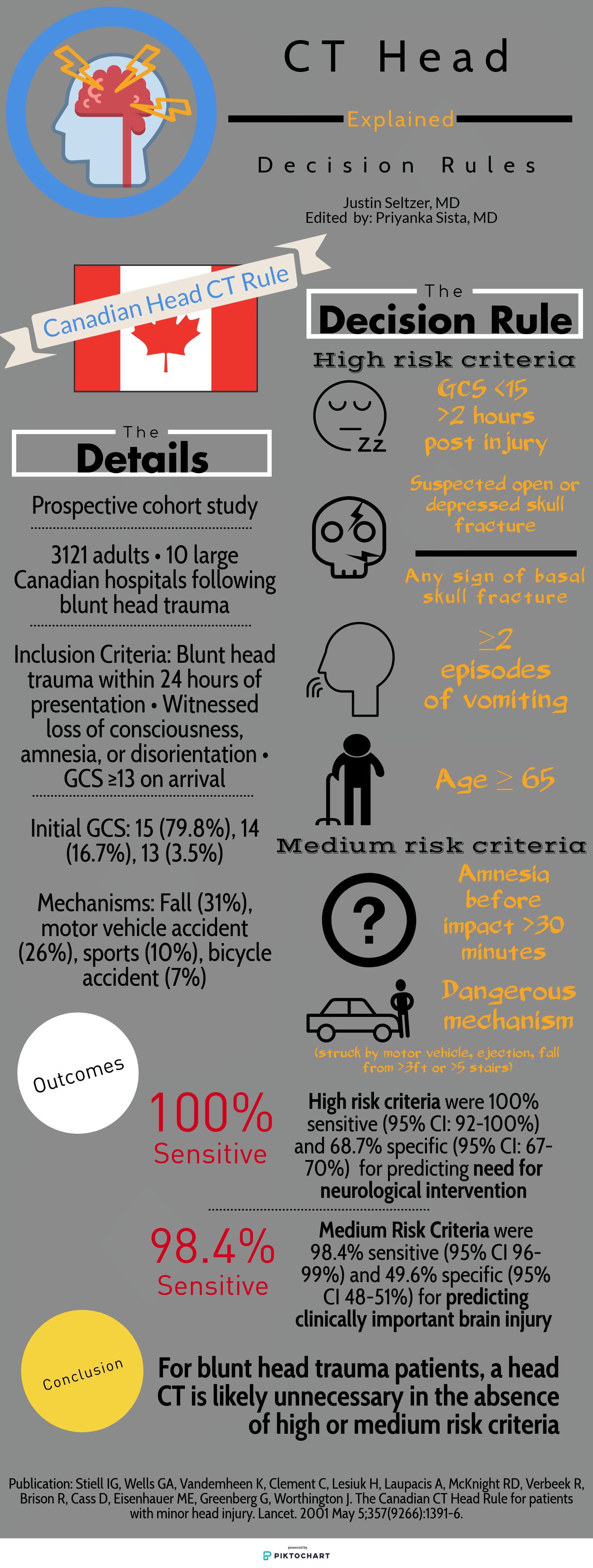
Deciding who needs exposure to radiation after blunt head injury has been looked at by both the Canadian Head Injury Guidelines as well as NEXUS. This website has excellent graphics outlining the rules. Note age over 65 alone is predictive of significant intracranial injury. All recent studies indicate age over 65 even with a low suspicion mechanism such as fall from standing is still a significant risk for intracranial pathology.
Category: Trauma
Keywords: Fall, alcohol, geriatric, head injury (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/15/2024)
Click here to contact Robert Flint, MD
A study looking at patients over age 65 with head injuries from falls assessed the association of alcohol use with severity of injury. The alcohol use was self-reported which does limit the findings. The study found “Of 3128 study participants, 18.2% (n = 567) reported alcohol use: 10.3% with occasional use, 1.9% with weekly use, and 6.0% with daily use.” Those daily drinkers had a higher incidence of intercranial injuries.
The authors concluded: “Alcohol use in older adult emergency department patients with head trauma is relatively common. Self-reported alcohol use appears to be associated with a higher risk of ICH in a dose-dependent fashion. Fall prevention strategies may need to consider alcohol mitigation as a modifiable risk factor.”
Zirulnik A, Liu S, Wells M, et al. Alcohol use is associated with intracranial hemorrhage in older emergency department head trauma patients. JACEP Open. 2024; 5:e13245. https://doi.org/10.1002/emp2.13245
Category: Trauma
Keywords: Cspine, nexus, Canadian, rule (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/12/2024)
Click here to contact Robert Flint, MD
A reminder of two validated tools used to determine the need for cervical spine imaging in adult blunt trauma patients. A recent meta analysis concluded:
“Based on studies, both CCR and NEXUS were sensitive rules that have the potential to reduce unnecessary imaging in cervical spine trauma patients. However, the low specificity and false-positive results of both of these tools indicate that many people will continue to undergo unnecessary imaging after screening of cervical SCI using these tools. In this meta-analysis, CCR appeared to have better screening accuracy.”
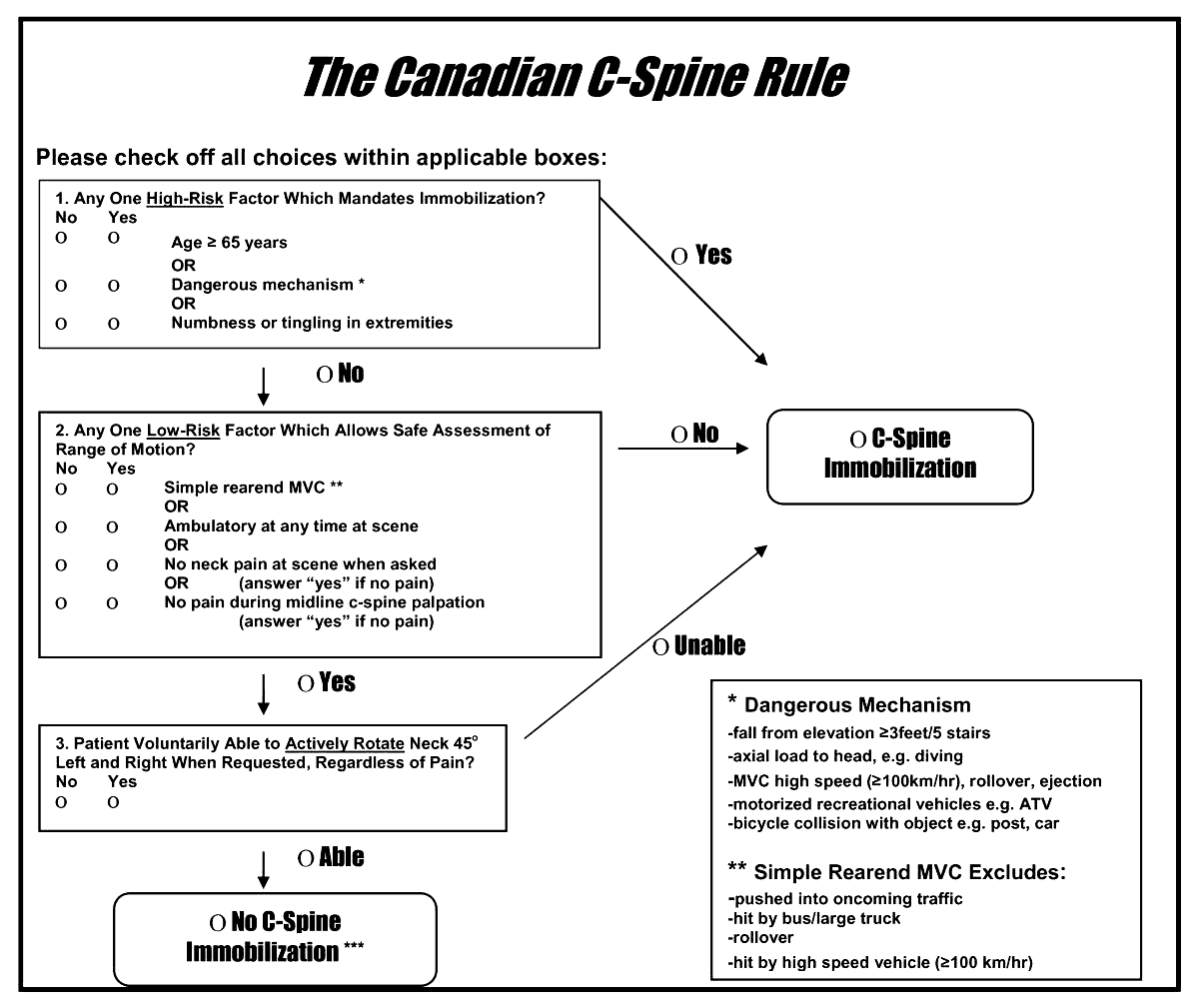
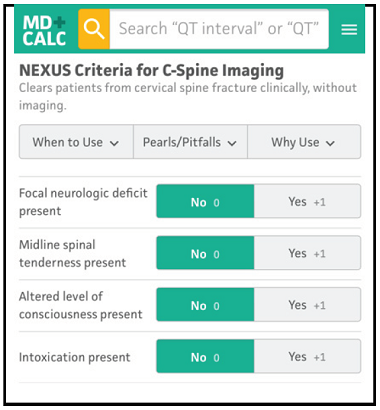
Arch Acad Emerg Med. 2023; 11(1): e5.
Published online 2023 Jan 1. doi: 10.22037/aaem.v11i1.1833
PMCID: PMC9807951
PMID: 36620739
Canadian C-spine Rule versus NEXUS in Screening of Clinically Important Traumatic Cervical Spine Injuries; a systematic review and meta-analysis
Category: Trauma
Keywords: Cspine, pecarn, rule, injury (PubMed Search)
Posted: 8/9/2024 by Robert Flint, MD
(Updated: 8/11/2024)
Click here to contact Robert Flint, MD
A just released study published in the Lancet gives us guidance on which pediatric blunt trauma patients need cervical spine imaging. Age range was 0-17 years.
“Out of 22,430 children included in the study, 433 (1.9%) were found to have Cervical spine injury (CSI). The study identified 4 high risk factors for CSI to be used to triage children to CT (12% risk for a cervical spine injury):
In children without high-risk findings, 5 additional findings identified children with intermediate, non-negligible risk of CSI (3.6% risk of a cervical spine injury):
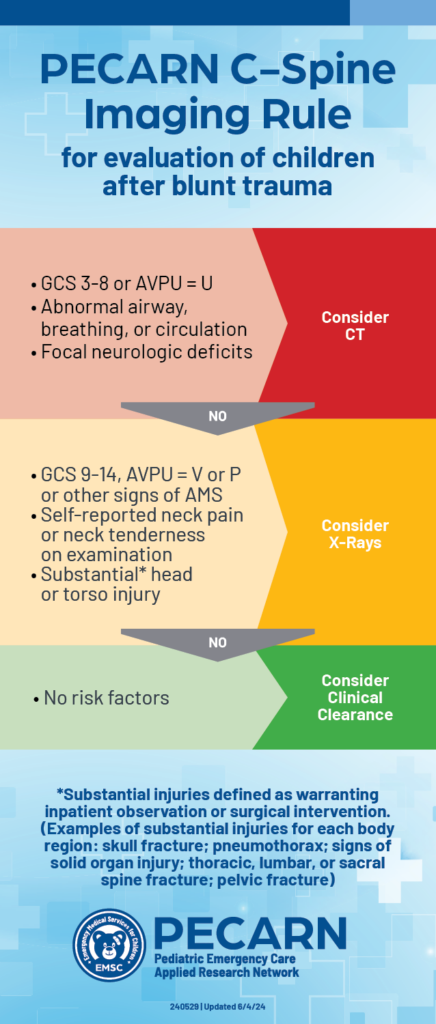
PECARN prediction rule for cervical spine imaging of children presenting to the emergency department with blunt trauma: a multicentre prospective observational study
Prof Julie C Leonard, MD Monica Harding, MS Prof Lawrence J Cook, PhD Prof Jeffrey R Leonard, MD
Prof Kathleen M Adelgais, MD Fahd A Ahmad, MD et al.
Published:June 03, 2024DOI:https://doi.org/10.1016/S2352-4642(24)00104-4
2. https://pecarn.org/pecarn_news/clinical-decision-rule-cervical-spine/
Category: Cardiology
Keywords: Hypertension, treatment, asymptomatic (PubMed Search)
Posted: 8/4/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This article from JAMA is targeted at inpatient management of asymptomatic hypertension, however, it’s a great reminder that “hypertensive urgency” is not an entity. We should be treating the patient and not the numbers. Gradual, out patient lowering of asymptomatic hypertension is the safe and proper way to approach this. Spread the word to your friends in primary care, urgent care, dental, and other office based practices.
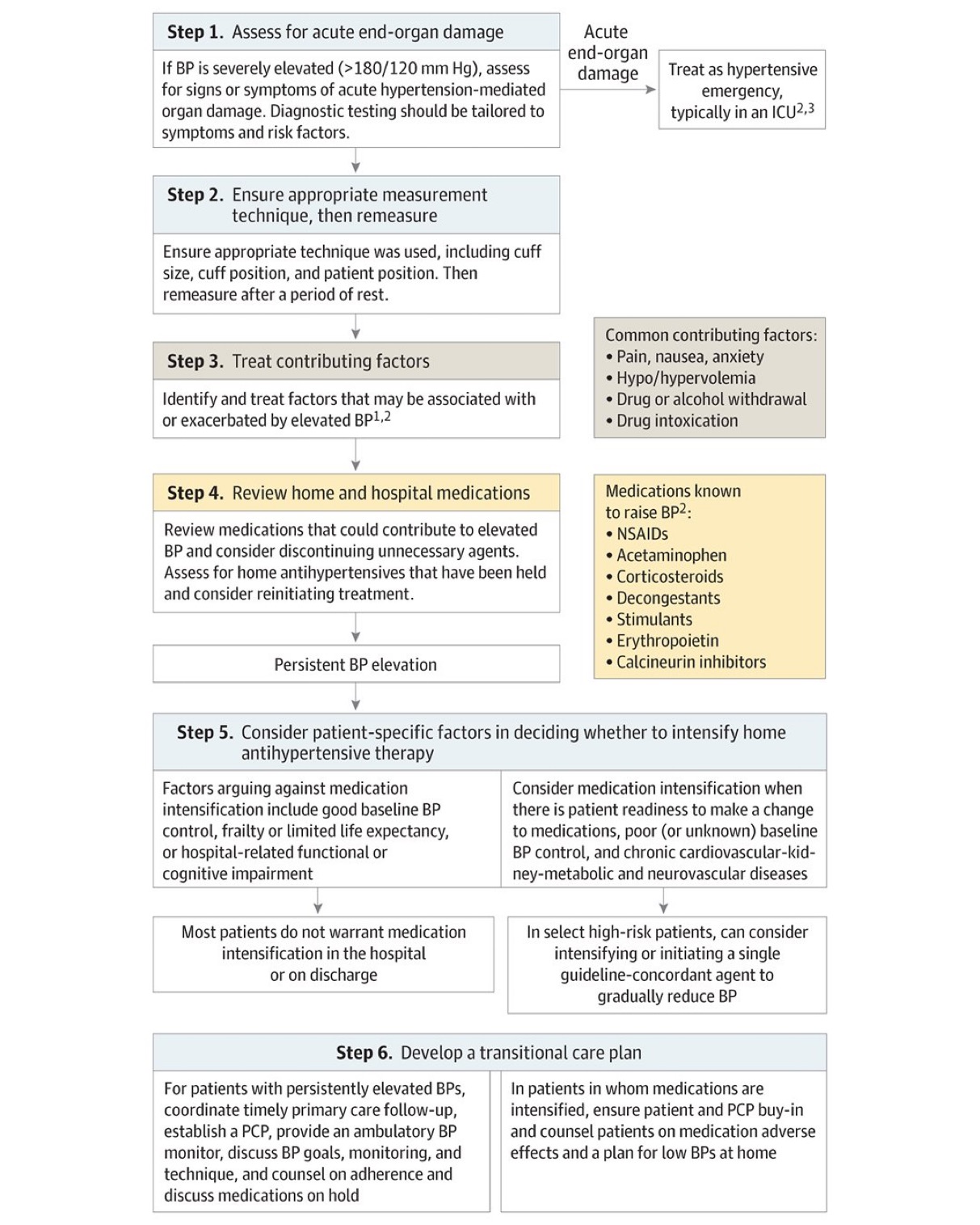
Jacobs ZG, Anderson TS. Management of Elevated Blood Pressure in the Hospital—Rethinking Current Practice. JAMA Intern Med. Published online July 22, 2024. doi:10.1001/jamainternmed.2024.3279
Category: Geriatrics
Keywords: Geriatrics, high risk medications, pharmacy (PubMed Search)
Posted: 8/3/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This article serves as a great reminder that our older patients are on a significant amount of medications and many of these medications effect cognition. Cognitively impaired patients are at risk of medication errors. High risk medications in older patients include anticoagulants, opioids, anticholinergics, hypoglycemic/insulin and sedating medications. The authors found:
It is important to ask how the patient takes (or doesn’t take) their medications as well as other social determinate of health such as living alone.
Journal of the American Geriatrics SocietyEarly View
CLINICAL INVESTIGATION
High-risk medication use among older adults with cognitive impairment living alone in the United States
Matthew E. Growdon MD, MPH, Bocheng Jing MS, Kristine Yaffe MD, Leah S. Karliner MD, MAS, Katherine L. Possin PhD, Elena Portacolone MBA, MPH, PhD, W. John Boscardin PhD, Krista L. Harrison PhD, Michael A. Steinman MD
First published: 26 July 2024
Category: Trauma
Keywords: Pneumothorax, chest X-ray, 38 mm, observation (PubMed Search)
Posted: 7/29/2024 by Robert Flint, MD
(Updated: 7/31/2024)
Click here to contact Robert Flint, MD
A cut-off of 35mm on CT scan has been shown to be predictive of which traumatic pneumothoracies require thoracostomy tube placement vs. safety of observation. This retrospective study looked at chest X-ray findings to see if there was a similar size cut-off where patients could be safely observed rather than undergo this invasive procedure. They found 38mm was the size over which observation failed. Of note, lactic acidosis and need for supplemental oxygen also predicted the need for chest tube placement
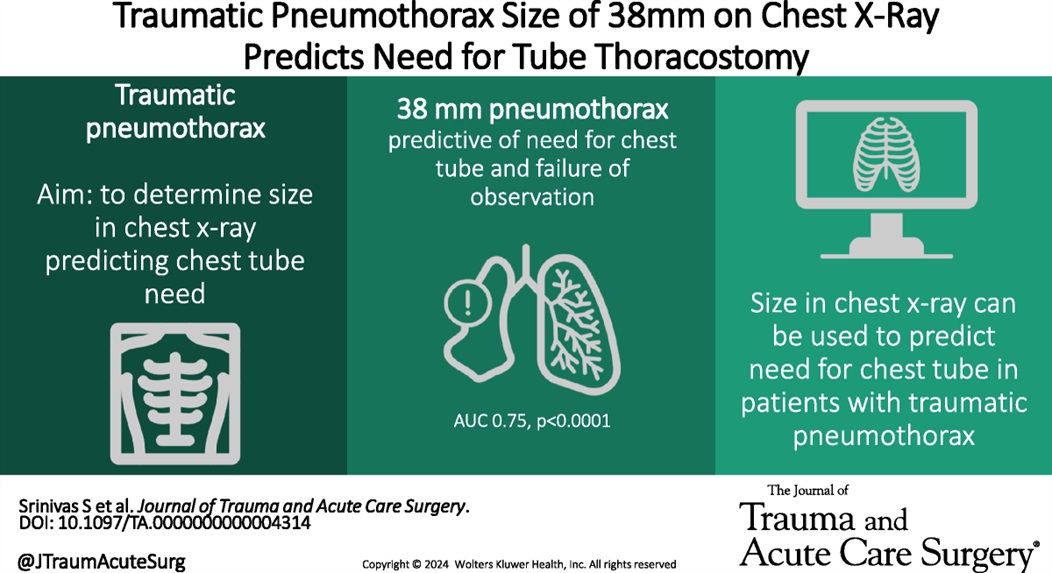
Using chest X-ray to predict tube thoracostomy in traumatic pneumothorax: A single-institution retrospective review
Srinivas, Shruthi MD; Henderson, Katelyn BS; Bergus, Katherine C. MD; Jacobs, Ayanna MD; Baselice, Holly MPH; Donnelly, Edwin MD, PhD; Valdez, Carrie MD; Tracy, Brett M. MD; Coleman, Julia R. MD, MPH
Journal of Trauma and Acute Care Surgery 97(1):p 82-89, July 2024. | DOI: 10.1097/TA.0000000000004314
Category: Trauma
Keywords: TBI, hypotension, vasopressors (PubMed Search)
Posted: 7/29/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
In this prospective, observational study of trauma patients with isolated head trauma, 62% of patients developed post-intubation hypotension. Comparing patients receiving hypertonic saline, vasopressors, crystalloid, or blood those receiving hypertonic saline and vasopressors had less post-intubation hypotension.
TBI patients who develop hypotension have worse outcomes. This study reminds us the use of vasopressors in trauma patients to maintain blood pressure is appropriate in the correct circumstances.
Anand, Tanya MD, MPH, MT(ASCP); Hejazi, Omar MD; Conant, Madolyn BS; Joule, Dylan BS; Lundy, Megan MD; Colosimo, Christina DO, MS; Spencer, Audrey MD; Nelson, Adam MD; Magnotti, Lou MD; Joseph, Bellal MD
Journal of Trauma and Acute Care Surgery 97(1):p 112-118, July 2024. | DOI: 10.1097/TA.0000000000004306
Category: Infectious Disease
Keywords: Idea, cystitis, aminoglycosides, single dose (PubMed Search)
Posted: 7/27/2024 by Robert Flint, MD
(Updated: 7/28/2024)
Click here to contact Robert Flint, MD
The Infectious Disease Society of America in 2023 recommended a single dose of an aminoglycoside for uncomplicated cystitis treatment in those with resistance or other contraindications to first line oral agents who were otherwise well enough to be discharged. This very small study (13 participants) suggest this strategy works for complicated (“male sex, urinary flow obstruction, renal failure or transplantation, urinary retention, or indwelling catheters”) cystitis patients who could otherwise be discharged home.
Academic Emergency MedicineVolume 31, Issue 7 p. 649-655
Jordan E. Jenrette PharmD, Kyle Coronato PharmD, Matthew A. Miller PharmD, Kyle C. Molina PharmD, Alexander Quinones MD, Gabrielle Jacknin PharmD
First published: 07 March 2024
Category: Trauma
Keywords: Txa, TBI, seizure, risk (PubMed Search)
Posted: 7/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
According to this study, no TXA 2g bolus was not found to increase the number of seizures in TBI pts.
TXA has been shown to improve mortality in inter cranial hemorrhage trauma patients if given within 2 hours. TXA is also known to lower seizure threshold. This study was a secondary analysis of a larger study comparing placebo to 1 g TXA bolus plus 8 hour infusion or 2g bolus TXA in the prehospital setting. There was no difference in the number of pts experiencing seizure or outcome in those receiving the 2g bolus of TXA.
The Association Between Tranexamic Acid and Seizures in Moderate or Severe Traumatic Brain Injury
David V. Deshpande BS a, W. Ian McKinley MD, MS b, Andrew J. Benjamin MD, MS c, Martin A. Schreiber MD, FACS, FCCM d, Susan E. Rowell MD, MBA, MCR
Volume 301, September 2024, Pages 359-364 https://doi.org/10.1016/j.jss.2024.06.035
Category: Pulmonary
Keywords: pulmonary embolism, intervention, scoring, out come (PubMed Search)
Posted: 7/18/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Deciding which pulmonary embolism patient needs thrombolytics/catheter based intervention is a shared decision among emergency physicians, intensivists, interventionalists, hospitalists, and the patient/family. This article provides evidence to help guide this decision. Keep in mind “The use of either CDL or catheter-based embolectomy in patients with intermediate-risk PE has, thus far, been correlated only with more rapid improvement of RV dysfunction than anticoagulation alone, not short- or long-term clinical or functional outcomes.”
"1. Massive (AHA) or high risk (ESC): Hypotension, defined as a systolic blood pressure <90 mm?Hg, a drop of >40 mm?Hg for at least 15 minutes (this latter criterion may be difficult to ascertain in some clinical circumstances), or need for vasopressor support, identifies these patients. They account for ?5% of hospitalized patients with PE and have an average mortality of ?30% within 1 month.
2.Submassive (AHA) or intermediate risk (ESC): RV strain without hypotension (see above) primarily identifies these patients. RV strain includes RV dysfunction on computed tomography pulmonary angiography or echocardiography (RV/left ventricular [LV] ratio >0.9)6,7 or RV injury and pressure overload detected by an increase in cardiac biomarkers such as troponins or brain natriuretic hormone.
3.Low risk (ESC and AHA): These patients do not meet criteria for submassive (AHA) or intermediate-risk (ESC) PE"
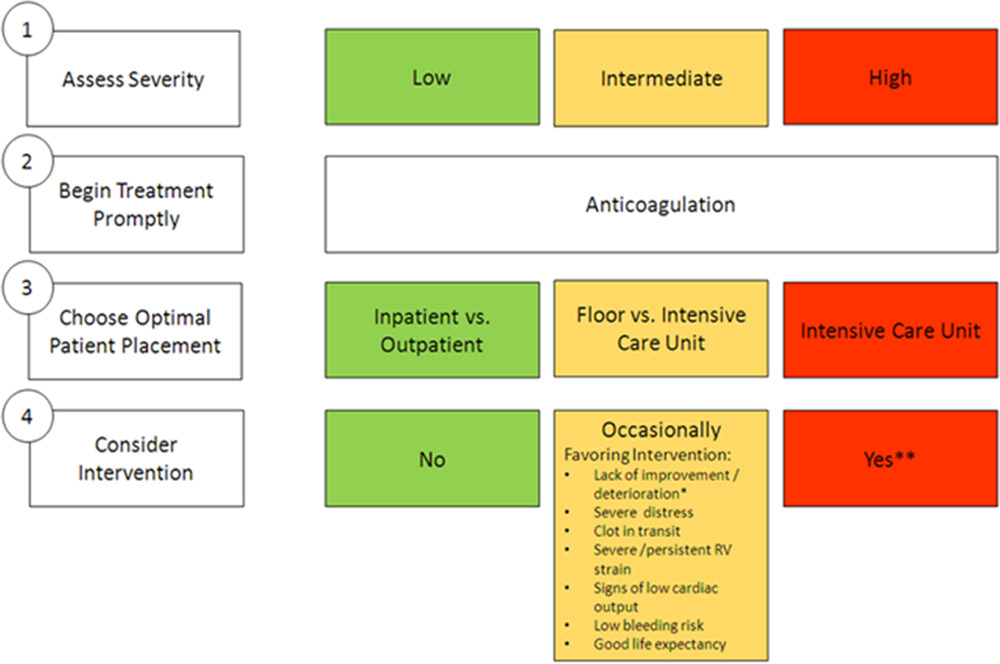
Interventional Therapies for Acute Pulmonary Embolism: Current Status and Principles for the Development of Novel Evidence: A Scientific Statement From the American Heart Association
Jay Giri, MD, MPH, FAHA, Chair, Akhilesh K. Sista, MD, FAHA, Vice Chair, Ido Weinberg, MD, MSc, Clive Kearon, MB, PhD, Dharam J. Kumbhani, MD, FAHA, Nimesh D. Desai, MD, PhD, Gregory Piazza, MD, MS, FAHA, Mark T. Gladwin, MD, FAHA, Saurav Chatterjee, MD, Taisei Kobayashi, MD, Christopher Kabrhel, MD, MPH, and Geoffrey D. Barnes, MD, MSc, FAHAAUTHOR INFO & AFFILIATIONS
Circulation
Category: Pulmonary
Keywords: pulmonary embolism, BOVA Sscore, intervention (PubMed Search)
Posted: 7/11/2024 by Robert Flint, MD
(Updated: 7/14/2024)
Click here to contact Robert Flint, MD
The Bova score has been validated to predict mortality and complications in hemodynamically stable patients with intermediate to high-risk pulmonary embolisms. There is some literature on using the Bova score to decide on thrombolytics/interventional therapy as well.
Scoring Criteria:
Interpretation:
Category: Trauma
Keywords: facial trauma, orbit, fracture (PubMed Search)
Posted: 7/7/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Patient struck in left eye. The patient was asked to look up during exam and this is the finding. What imaging modality would you order if so inclined, what is the injury, and what is the disposition/plan?

Concern for a left orbital “blowout” fracture with muscle entrapment. Also called the trapdoor fracture. CT is the imaging modality of choice not plain films. This injury requires emergent consultation with a face surgeon (plastics, ENT or oculoplastics.). Right orbital fracture in the photo below.
-668ade5e780f0.jpg)
1.https://www.researchgate.net/figure/Girl-with-blowout-fracture-of-the-left-orbit-and-enophthalmos_fig1_351847537
2.|The Lancet. VOLUME 395, ISSUE 10221, P370, FEBRUARY 01, 2020
Paul Geraeds Kemps, BSc Michaël Herman Frank, MD
Published: February 01, 2020DOI:https://doi.org/10.1016/S0140-6736(19)33223-4
Category: Orthopedics
Keywords: Hip fracture (PubMed Search)
Posted: 7/6/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Category: Trauma
Keywords: Ketamine intranadal fentanyl trauma pain (PubMed Search)
Posted: 6/30/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
192 trauma patients who were receiving pre-hospital fentanyl for moderate to severe pain were randomized to placebo or intranasal 50 mg ketamine as an adjunct for pain control. There was no difference between the two groups in decrease in pain scale.
The authors concluded: “In our sample, we did not detect an analgesic benefit of adding 50 mg intranasal ketamine to fentanyl in out-of-hospital trauma patients.”
Jason T. McMullan, MD, MS Christopher A. Droege, PharmD Kathleen M. Chard, PhD Kim Ward Hart, MA
Christopher J. Lindsell, PhD Richard J. Strilka, MD, PhD
Open AccessPublished:June 12, 2024DOI:https://doi.org/10.1016/j.annemergmed.2024.04.018
Category: Cardiology
Keywords: syncope, pre-syncope (PubMed Search)
Posted: 6/27/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
The systematic review of presyncope literature found that presyncope should be treated the same as syncope in terms of work up and disposition.
“In conclusion, the prevalence of short-term serious outcomes among ED patients with presyncope ranges from one in four to one in 20, with arrhythmia being the most common serious outcome. Our review indicates that presyncope may carry a similar risk to syncope, and hence, the same level of caution should be exercised for ED presyncope management as that of ED syncope.”
Serious outcomes among emergency department patients with presyncope: A systematic review
Hadi Mirfazaelian MD, MSc, Ian Stiell MD, MSc, FRCPC, Rasoul Masoomi PhD, Khazar Garjani MD, Venkatesh Thiruganasambandamoorthy MBBS, CCFP-EM, MSc
First published: 09 June 2024 Academic Emergency Medicine
Category: Pharmacology & Therapeutics
Keywords: alcohol use disorder, phenobarbital, naloxone, treatment (PubMed Search)
Posted: 6/23/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Two recommendations from the recent GRACE 4 publication in Academic Emergency Medicine to consider:
1. Use phenobarbital along with benzodiazepines in patients with moderate to severe alcohol withdrawal. The evidence isn’t robust but is positive when compared to benzos alone.
2. Adults with alcohol use disorder can benefit from anti-craving medications such as naloxone and gabapentin at time of discharge.
Guidelines for Reasonable and Appropriate Care in the Emergency Department (GRACE-4): Alcohol use disorder and cannabinoid hyperemesis syndrome management in the emergency department Bjug Borgundvaag PhD, MD, CCFP(EM), Fernanda Bellolio MD, MSc, Isabelle Miles MD, Evan S. Schwarz MD, Sameer Sharif MD, MSc, Mark K. Su MD, MPH, Kevin Baumgartner MD, David B. Liss MD, Hasan Sheikh MD, MPA, Jody Vogel MD, MSc, MSW, Emily B. Austin MD, Suneel Upadhye MD, MSc, Michelle Klaiman MD, FRCPC, DABAM, Robert Vellend, Anna Munkley, Christopher R. Carpenter MD, MSc
First published: 15 May 2024
Academic Emergency Medicine https://doi.org/10.1111/acem.14911
Category: Trauma
Keywords: troponin fall geriatric trauma (PubMed Search)
Posted: 6/20/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
A prospective European study of patients over age 65 presenting with a ground level fall obtained troponin levels to ascertain if myocardial infarction was a cause of the ground level fall. Troponin levels were elevated in a majority of patients however only 0.5% were defined as having a myocardial infarction. Of the 3% who died within 1 year, troponin was found to be higher than those that survived the one-year study period. The authors concluded “Our data do not support the opinion that falls may be a common presenting feature of MI. We discourage routine troponin testing in this population. However, hs-cTnT and hs-cTnI were both found to have prognostic properties for mortality prediction up to 1?year.”
Diagnostic and prognostic value of cardiac troponins in emergency department patients presenting after a fall: A prospective, multicenter study
Tanguy Espejo, Lukas Terhalle, Alexandra Malinovska MD, Henk B. Riedel MD, Laura Arntz MD, Livia Hafner, Karen Delport-Lehnen MD, Joanna Zuppinger MD,
First published: 26 March 2024
Academic Emergency Medicine
Category: Trauma
Keywords: hemorrhage, tourniquet, innovation, Delphi (PubMed Search)
Posted: 6/9/2024 by Robert Flint, MD
(Updated: 6/16/2024)
Click here to contact Robert Flint, MD
Appropriately, a great deal of time and energy is being expended to educate on the use of tourniquets to prevent mass hemorrhage. Are the current generation of tourniquets the best that we can have? These authors performed a Delphi study to assess needs with tourniquet design.
They concluded the next generation of tourniquets should have the following: “Capable of being used longer than 2 hours, applied and monitored by anyone, data displays, semiautomated capabilities with inherent overrides, automated monitoring with notifications and alerts, and provide recommended actions.”
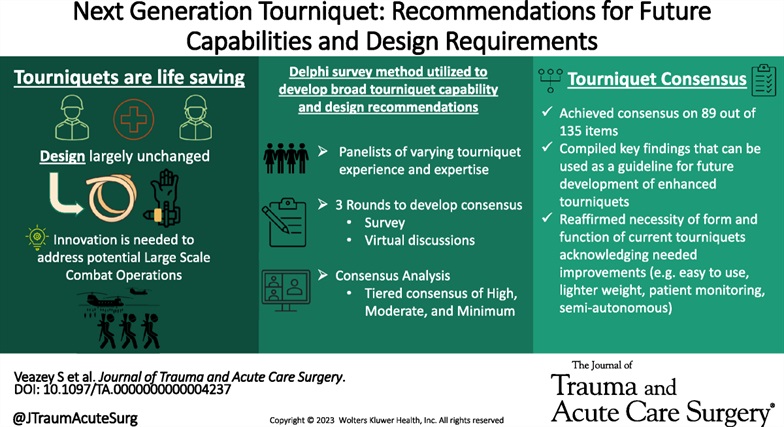
Veazey, Sena R. MS; Mike, Jared F. PhD; Hull, Darke R. BS; Ryan, Kathy L. PhD; Salinas, Jose PhD; Kragh, John F. Jr MD. Next-generation tourniquet: Recommendations for future capabilities and design requirements. Journal of Trauma and Acute Care Surgery 96(6):p 949-954, June 2024. | DOI: 10.1097/TA.0000000000004237
