Category: Orthopedics
Keywords: Gout (PubMed Search)
Posted: 4/10/2011 by Brian Corwell, MD
(Updated: 4/16/2011)
Click here to contact Brian Corwell, MD
Gout Part 2
Man CY, Cheung IT, Cameron PA, Rainer TH. Comparison of oral prednisolone/paracetamol and oral indomethacin/paracetamol combination therapy in the treatment of acute gout like arthritis: a double-blind, randomized, controlled trial. Ann Emerg Med. 2007;49:670-677.
Category: Orthopedics
Keywords: Knee Dislocation, Prosthetic (PubMed Search)
Posted: 4/9/2011 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Knee dislocations are uncommon, and prosthetic knee dislocations even rarer. Some general facts about prosthetic knee dislocations are:
Wang CJ, Wang HE. Dislocation of total knee arthroplasty: a report of 6 cases with 2 patterns of instability. Acta Orthop Scand 1997;68:282-285.
Stiehl JB, Komistek RD, Dennis DA, et al. Fluoroscopic analysis of kinematics after posterior-cruciate-retaining knee arthroplasty. J Bone Joint Surg Br 1995;77:884-889.
Category: Orthopedics
Keywords: Gout, uric acid (PubMed Search)
Posted: 3/26/2011 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
GOUT part 1
Gout is an inflammatory arthritis that classically affects the first metatarsal phalangeal joint
Gout prefers cool ambient temperature hence gouty tophi prefer the great toe (one of the coldest parts of the body) and avoids "warmer" joints such as the hip and shoulder.
Remember that gout can affect other joints as well (elbow, wrist, knee and ankle) and can cause painful bursitis and tendonitis
Multiple joints can be involved simultaneously (leading to confusing with RA and OA)
The involved joint will often be red, hot, swollen and very painful leading to easy confusion with cellulitis and or a septic arthritis
Diagnose gout by demonstrating monosodium urate crystals in the synovial fluid.
**Remember previous pearl by Dr. Bond regarding the coexistence of gout with septic joint**
Serum uric acid levels are commonly elevated but can be normal or even low
Use caution with this test because asymptomatic hyperuricemia is much more common than gout
Category: Orthopedics
Posted: 3/12/2011 by Michael Bond, MD
(Updated: 3/19/2011)
Click here to contact Michael Bond, MD
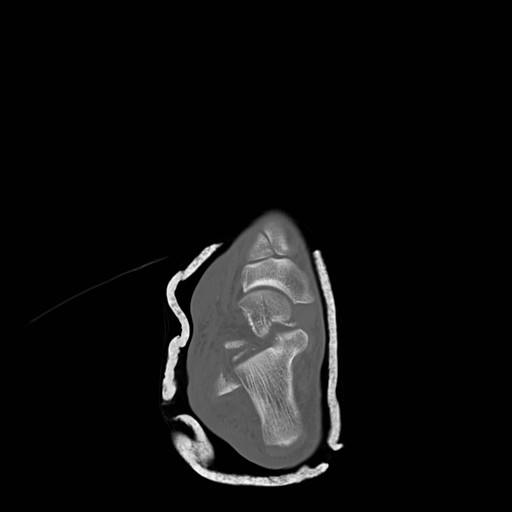
Talar Neck Fractures
Have a high rate of avascular necrosis (AVN), nonunion, and arthritis. Almost all require ORIF


Category: Orthopedics
Keywords: nerve entrapment, ulnar nerve, elbow (PubMed Search)
Posted: 3/12/2011 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Cubital Tunnel Syndrome aka Radial Tunnel Syndrome
Category: Orthopedics
Keywords: apophysitis, overuse injuries, heel pain, achilles (PubMed Search)
Posted: 2/26/2011 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Sever's disease ,aka calcaneal apophysitis, is a common overuse injury in the pediatric and adolescent population.
Occurs secondary to traction of the calcaneus that most often occurs in young athletes (8-12 yo)
-Avg. age of presentation is 11 years 10 months in boys & 8 years 8 months in girls
-Repetitive traction to the weaker apophysis, induced by the pull of the Achilles on its insertion
Hx: Heel pain that increases with activity (running, jumping).
-May involve one (40%) or both (60%) feet
PE: Tenderness of the posterior heel at the Achilles tendon insertion and ankle dorsiflexor weakness
Imaging: Radiography is often normal. When positive, show fragmentation and sclerosis of the calcaneal apophsis. NOTE: These findings are nonspecific and also are observed in asymptomatic feet.
http://t0.gstatic.com/images?q=tbn:ANd9GcQ9R-fx1iyhbhNJpNL2W72bWdK72_mRBLNX5DUDtcMfnDli-x7Ong
DDx: Includes osteomyelitis and tarsal coalition.
Tx: Rest from aggravating activities, NSAIDs, ice (both pre and post sport). When pain free a program of stretching (gastrocnemius-soleus), strengthening (dorsiflexors) and shoe inserts (heel cups, lifts, pads, or orthotics) can provide significant pain relief.
Category: Orthopedics
Keywords: radius, fracture, treatment (PubMed Search)
Posted: 2/19/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Distal Radius Fractures
Typically distal radius fractures are treated with closed reduction and splinting in the ED, followed by operative repair. This is done because it is felt that patients will have the best functional outcomes if the bones are restored to their normal anatomic alignment. However, two studies published in 2010 suggest differently.
The study by Neidenbach showed that after one year there was no difference in functional outcomes between patients that were just splinted in the ED in the position the fracture was found versus those that had closed reduction with splinting.
The second study by Ego showed that there was no difference in outcomes between those that underwent conservative treatment with closed reduction and splinting versus those that underwent operative repair.
The take home point from these studies for the EM physician is that most distal radius fractures can be splinted in the position found with them following up with an orthopaedist. There is probably little advantage to performing a closed reduction in the ED knowing that this procedure can use a lot of valuable time and resources.
Neidenbach P, Audige L, Wilhelmi-Mock M, Hanson B, De Boer P. The efficacy of closed reduction in displaced distal radius fractures. Injury. 2010;41(6):592-598.
Egol KA, Walsh M, Romo-Cardoso S, Dorsky S, Paksima N. Distal radial fractures in the elderly: operative compared with nonoperative treatment. J Bone Joint Surg Am. 2010;92(9):1851-1857.
Category: Orthopedics
Keywords: iliotibial band, knee pain (PubMed Search)
Posted: 1/22/2011 by Brian Corwell, MD
(Updated: 2/19/2011)
Click here to contact Brian Corwell, MD
Iliotibial band syndrome (ITBS)
http://footcarexpress.com/foot-orthotics/wp-content/uploads/2009/01/iliotibial-band-syndrome.jpg
Hx -
PE-
Tx
Category: Orthopedics
Keywords: Shoulder, Dislocation, FARES (PubMed Search)
Posted: 1/15/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
FARES Method for Reduction of Anterior Shoulder Dislocations.
This method that was recently highlighted in a publication had a ~78% success rate with the authors able to reduce the shoulder in an average of 2.36 ±1.24 minutes without having to give the patients any analgesics or sedatives. The technique is done by:
Consider trying this with your next shoulder dislocation. No single method of reduciton is 100% successful, but methods like this that only require a single provider and do not require analgesics are extremely helpful in improving patient flow as they do not utilize a lot of ED resources..
Category: Orthopedics
Posted: 1/8/2011 by Brian Corwell, MD
(Updated: 2/19/2011)
Click here to contact Brian Corwell, MD
Involves an avulsion of the flexor digitorum profundus (FDP) tendon from its insertion on the distal phalanx.
Ring finger is most commonly involved.
Usually occurs from a grabbing attempt (resulting in forced DIP extension during maximal FDP contraction) as would occur while attempting to grab someone’s jersey such as in football or rugby.
Clinically, there is normal passive DIP ROM with loss of active flexion. Examine this by asking the patient to flex the fingertip at the DIP while the PIP joint is held in extension.
*Remember that patients with a 90% full-thickness tendon laceration may still have normal (albeit painful) range of motion. The examiner must evaluation the strength of the tendon against resistance. This injury is commonly missed as it is diagnosed as a “jammed” finger.
Plain films may show a bony avulsion, but are often negative.
Treatment is primary repair especially with large bony fragments. Partial ruptures can be treated nonoperatively at the discretion of the hand surgeon.
Category: Orthopedics
Keywords: peroneal, tendon, subluxation (PubMed Search)
Posted: 1/1/2011 by Michael Bond, MD
Click here to contact Michael Bond, MD
Peroneal Tendon Subluxation: The Other Ankle Sprain
Roth et al. Peroneal tendon subluxation: the other lateral ankle injury. Br J Sports Med (2010) vol. 44 (14) pp. 1047-53
Category: Orthopedics
Keywords: Sports medicine, Sudden cardiac death, Commotio Cordis, Defibrillation (PubMed Search)
Posted: 12/25/2010 by Brian Corwell, MD
(Updated: 2/19/2011)
Click here to contact Brian Corwell, MD
Commotio Cordis
Emergency medicine & sports medicine physicians often cover sporting events where athletes are at risk of commotio cordis
Palacio LE, Link MS. Commotio Cordis. 2009.
Category: Orthopedics
Keywords: Septic Arthritis, Diagnosis (PubMed Search)
Posted: 12/18/2010 by Michael Bond, MD
(Updated: 12/19/2010)
Click here to contact Michael Bond, MD
Septic Arthritis
It is generally taught that if the synovial fluid white blood count (WBC) is less than 50,000 it is not septic, however, there is growing evidence that a clear delineation in the WBC between septic arthritis and inflammatory arthritis is not possible. In fact, inflammatory arthritis (rheumatoid and gout) actually increases your risk for septic arthritis and the two can coexist. Gram stains of the fluid only show organisms in 50% of those with septic arthritis so you also can not rely on them either. Inflammatory markers (CRP, ESR) can be elevated with inflammatory or septic arthritis so they too can not differentiate between the two.
In the end, because of the risk of permanent joint dysfunction, it is important to make the diagnosis on clinical grounds and treat empirically if you are unsure. Err on the sound of treatment. Serial joint aspirations to drain synovial fluid have the same outcomes as operative washout.
A recent article that discusses the concerns with making the diagnosis of septic arthritis is:
Mathews et al. Bacterial septic arthritis in adults. Lancet (2010) vol. 375 (9717) pp. 846-55
Mathews et al. Bacterial septic arthritis in adults. Lancet (2010) vol. 375 (9717) pp. 846-55
Category: Orthopedics
Keywords: cervical, neck, radiculopathy (PubMed Search)
Posted: 12/10/2010 by Brian Corwell, MD
(Updated: 12/18/2010)
Click here to contact Brian Corwell, MD
Cervical Radiculopathy
The most commonly affected level is C7 (31-81%), followed by C6 (19-25%), C8 (4-12%) and C5 (2-14%)
Anterior compression can selectively affect motor fibers
Posterior compression can selectively affect sensory fibers
-More common due to posterior lateral disc herniation or facet degeneration
Signs and symptoms: Sensory complaints (findings are in a root distribution) and possible weakness and reflex changes.
Wilbourn & Aminoff, 1998.
Category: Orthopedics
Keywords: spondyloysis, spondylosis, spondylolistesis, spondylitis (PubMed Search)
Posted: 12/4/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Dr. Corwell covered Spondyloysis in July 2010 https://umem.org/res_pearls_referenced.php?p=1134 but if you are like me you might have trouble remembering the differences between the following terms:
Category: Orthopedics
Keywords: Bursitis, heel pain (PubMed Search)
Posted: 11/27/2010 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Chief complaint: “Posterior heel pain”
http://www.aidmybursa.com/_img/ankle-retrocalcaneal-subcutaneous-bursitis.jpg
Retrocalcaneal bursitis
The retrocalcaneal bursa is located between the Achilles tendon and the posterior superior border of the calcaneus.
H&P: Inflammation and pain may follow repetitive dorsi/plantar flexion of the ankle (excessive running, jumping activities). Tenderness anterior and superior to the Achilles insertion on the heel.
Treatment: Minimize weight bearing. ½ inch elevation. NSAIDs.
Posterior calcaneal bursitis
This bursa is subcutaneous, just superficial to the insertion of the Achilles tendon.
H&P: Inflammation and pain may follow irritation from the upper border of the heel counter of a shoe. Posterior heel pain. Tender “bump” (the inflamed and swollen bursa) on the back of the heel.
http://podiatry.files.wordpress.com/2006/12/patient2.jpg
Treatment: Opened-heeled shoes, sandals, or placement of a “U-shaped” pad between the heel and the counter. NSAIDs. Advance to shoes with soft or less convex heel counters.
Category: Orthopedics
Keywords: Methylene Blue, Intra-articular, Joint (PubMed Search)
Posted: 11/21/2010 by Michael Bond, MD
Click here to contact Michael Bond, MD
Evaluation of Potential Intra-Articular Joint Lacerations
Skin and soft tissue injuries in proximity to a joint often prompt concern of whether the injury violated the joint space. Joint Space involvement is important to exclude as it can lead to septic joints and long term disability.
One easy way to determine if the joint capsule has been violated is to inject methylene blue into the joint and watch to see if any of the methylene blue extravasates through the soft tissue.
Indications for a methylene blue injection include:
There are no absolute contraindications. Though clearly the procedure does not need to be done when the injury highly suggests an open joint injury and the patient will require operative debridement and exploration.
To watch a video of a injection head to eMedicine by clicking http://emedicine.medscape.com/article/114453-overview
Shlamovitz, Gil. Injection, Intra-Articular Methylene Blue. eMedince, Accessed November 2010. http://emedicine.medscape.com/article/114453-overview
Category: Orthopedics
Keywords: Transverse Myelitis, spinal cord, MS (PubMed Search)
Posted: 11/13/2010 by Brian Corwell, MD
Click here to contact Brian Corwell, MD
Transverse Myelitis
A group of inflammatory disorders characterized by acute or subacute motor weakness, sensory abnormalities and autonomic (bowel, bladder, sexual) cord dysfunction.
Symptoms are usually bilateral but both unilateral and asymmetric presentations can occur.
Look for a well-defined truncal sensory level
-below which sensation of pain and temperature is altered or lost.
Causes: Autoimmune after infection or vaccination (60% of cases in children), direct infection, or a demyelinating disease such as MS. No cause is found in 15 – 30% of cases.
Incidence: Bimodal peak at 10-19 years and at 30-39 years.
Diagnostic testing: MRI of the ENTIRE spine to both rule out structural lesions and rule in an intrinsic cord lesion. If MRI is normal reconsider the original diagnosis.
Treatment: Steroids are first-line therapy. Dosing is controversial but generally involves high IV doses for 3-5 days (1000 mg methylprednisolone). Plasma exchange is second line for those who don’t respond to steroids.
Transverse Myelitis. Frohman EM, Wingerchuk DM. NEJM 2010 Aug 5;363(6):564-72.
Category: Orthopedics
Keywords: Spinal Epidural Abscess (PubMed Search)
Posted: 10/30/2010 by Michael Bond, MD
(Updated: 2/8/2026)
Click here to contact Michael Bond, MD
Risk Factors for Spinal Epidural Abscesses
Building on Dr. Corwell's pearl from last week concerning Spinal Epidural Abscess, risk factors for Spinal Epidural Abscesses other than IV drug abuse are:
The infection can occur via three routes 1) hematogenous spread 2) Direct Extension from a local infection such as osteoomyelitis, and 3) iatrogenic introduction which is thought to be responsible for 14-22% of the cases. A catheter in the epidural space for more than 2 days has a infection rate of 4.3%.
Marc Tompkins, Ian Panuncialman, Phillip Lucas, Mark Palumbo. Spinal Epidural Abscess The Journal of Emergency Medicine, Volume 39, Issue 3, September 2010, Pages 384-390
Category: Orthopedics
Keywords: EPIDURAL SPINAL CORD COMPRESSION, CAUDA EQUINA SYNDROME (PubMed Search)
Posted: 10/22/2010 by Brian Corwell, MD
(Updated: 2/8/2026)
Click here to contact Brian Corwell, MD
Epidural compression syndrome encompasses spinal cord compression, cauda equina syndrome, & conus medullaris syndrome.
Causes include:
Measurement of a post-void bladder residual volume tests for the presence of urinary retention with overflow incontinence (a common, though late finding) (sensitivity of 90%, specificity of 95%). Large post-void residual volumes (>100 mL) indicate a denervated bladder with resultant overflow incontinence and suggest significant neurologic compromise. The probability of cauda equina syndrome in patients without urinary retention is approximately 1 in 10,000.
Use this in your daily practice!!
The administration of glucocorticoids can minimize ongoing neurologic damage from compression & edema until definitive therapy can be initiated. The optimal initial dose and duration of therapy is controversial, with a recommended dose range of dexamethasone anywhere from 10 to 100 mg intravenously. Consider traditional dosing (dexamethasone 10 mg) for those with minimal neurologic dysfunction, & reserve the higher dose (dexamethasone 100 mg) for patients with profound or rapidly progressive symptoms, such as paraparesis or paraplegia.
1. Deyo RA, Rainville J, Kent DL. What can the history and physical examination tell us about low back pain? JAMA 1992;268:760–5.
2. Gregory D, Seto C, Wortley G, et al. Acute lumbar disk pain: navigating evaluation and treatment choices. Am Fam Physician 2008;78:835–42.
3. Loblaw DA, Laperriere NJ. Emergency treatment of malignant extradural spinal cord compression: an evidence-based guideline. J Clin Oncol 1998;16:1613–24.
