Category: Pediatrics
Posted: 5/31/2024 by Rachel Wiltjer, DO
(Updated: 2/8/2026)
Click here to contact Rachel Wiltjer, DO
Histamine is present in mosquito saliva contributing to itch with bites, however, certain populations – including children – can experience an exaggerated reaction. Skeeter syndrome is a large, localized inflammatory reaction secondary to a mosquito bite that presents with warmth, swelling, and itching. There can occasionally be associated lymphadenopathy and fever as well. The rapid onset is what best differentiates it from cellulitis. Treatment is primarily symptomatic in nature, focused on relieving itch, with antihistamines and topical therapy. There may also be a role for prophylactic antihistamine usage at times when mosquito bites will be unavoidable in a patient known to have developed Skeeter syndrome previously. Other patients who may be affected include those with immunologic and autoimmune phenomena, those with underlying atopy, outdoor workers with frequent exposure, and those with new exposure to indigenous mosquitos.
Take Home: Consider insect (mosquito bite) when evaluating for cellulitis/infection in pediatric patients, with impressive skin findings but otherwise unremarkable exams. They present with rapid onset and itching instead of pain. This can be especially prominent in periorbital and auricular presentations.
Vander Does A, Labib A, Yosipovitch G. Update on mosquito bite reaction: Itch and hypersensitivity, pathophysiology, prevention, and treatment. Front Immunol. 2022 Sep 21;13:1024559
Category: Pediatrics
Keywords: psych, pediatric mental health, suicide (PubMed Search)
Posted: 5/17/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a cross sectional study examining insurance data to determine if there is seasonality related to ED visits and psychiatric hospitalizations related to suicidality.
Suicidality includes both suicidal ideation and suicide attempts (but not suicide). One survey showed that up to 12% of US adolescents reported serious thoughts of suicide. This study included 73,123 patients where 19.4% were direct inpatient admissions and 80.6% were ED visits, 44% of whom were subsequently admitted.
Metrics for suicidality in 10-18 year olds peaked in April and October with a nadir in June. Incidentally, in the Spring of 2020 when US schools closed due to COVID, there was a decrease in both ED visits and hospitalizations with April and May having the lowest rates across the study period.
School is believed to increase stress with risk factors such as bullying and peer pressure, academic and extracurricular stressors and poor sleep hygiene.
Bottom line: There has been an increase in adolescent suicidality over the recent years, many of whom present to the ED for evaluation. More mental health resources are needed, especially during the school year.
Bottom line: There has been an increase in adolescent suicidality over the recent years, many of whom present to the ED for evaluation. More mental health resources are needed, especially during the school year.
Category: Pediatrics
Posted: 4/5/2024 by Kathleen Stephanos, MD
(Updated: 5/10/2024)
Click here to contact Kathleen Stephanos, MD
Intranasal medications are an increasingly popular option for pediatric patients, particularly for analgesia and anxiolysis, with an increasing number of medications being used via the intranasal route of administration.
Fentanyl has been shown in prior studies to be a safe and effective pain management strategy for children, but is likely under utilized. In sickle cell patients, studies have shown that time to analgesia may improve outcomes including hospitalization.
In 2023, Rees et al. showed that in the sickle cell patient population IN fentanyl can be a very effective tool for patient's experiencing a Vaso-occlusive episode (VOE). This study looked at 400 children with a mean age of 14.6 years. Of these 19% received IN fentanyl.
Ultimately, the IN fentanyl patient population had a shorter time to initial administration of analgesia and a lower chance of admission to the hospital.
Notably, this was not a randomized study, so there is limitations in assessment of the causality of the lower discharge rates. However this is a tool that could likely be used more regularly in the pediatric sickle cell patient population to allow for more rapid pain management in the emergency department.
1. Payne J, Aban I, Hilliard LM, Madison J, Bemrich-Stolz C, Howard TH, Brandow A, Waite E, Lebensburger JD. Impact of early analgesia on hospitalization outcomes for sickle cell pain crisis. Pediatr Blood Cancer. 2018 Dec;65(12):e27420. doi: 10.1002/pbc.27420. Epub 2018 Aug 27. PMID: 30151977; PMCID: PMC6192851.
2. Rees CA, Brousseau DC, Ahmad FA, Bennett J, Bhatt S, Bogie A, Brown KM, Casper TC, Chapman LL, Chumpitazi CE, Cohen DM, Dampier C, Ellison AM, Grasemann H, Hatabah D, Hickey RW, Hsu LL, Bakshi N, Leibovich S, Patil P, Powell EC, Richards R, Sarnaik S, Weiner DL, Morris CR; SCD Arginine Study Group and PECARN. Intranasal fentanyl and discharge from the emergency department among children with sickle cell disease and vaso-occlusive pain: A multicenter pediatric emergency medicine perspective. Am J Hematol. 2023 Apr;98(4):620-627. doi: 10.1002/ajh.26837. Epub 2023 Feb 6. PMID: 36606705; PMCID: PMC10023395.
Category: Pediatrics
Keywords: UTI, antibiotic, duration (PubMed Search)
Posted: 4/19/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
This was a multicenter, randomized double blind, placebo controlled, non inferiority trial looking at children aged 2 months to 10 years with a diagnosis of urinary tract infection to see if the antibiotic course could be shortened from 10 days to 5 days in those patients who have clinically improved by day 5.
Children were prescribed amoxicillin/clavulanic acid, cefixime, cefdinir, cephalexin or trimethoprim-sulfamethoxazole and on day 6, after an in person visit were switched to placebo or continued the same antibiotic course.
A urine sample was collected on days 11-14 and treatment failure was defined as symptomatic urinary tract infection at or before this visit, asymptomatic bacteriuria, positive urine culture or gastrointestinal colonization with resistant organisms.
693 children were randomized in this trial. Children who received 5 days of antibiotics were more likely to have asymptomatic bacteriuria or a positive urine culture on days 11-14 (0.6 vs 4.2%). 28 children would need to be treated with a 10 day course to prevent one treatment failure with the 5 day course.
Bottom line: 10 days is still the ideal duration of treatment for a urinary tract infection, but the rate of failure of a 5 day course was low and the clinical significance of asymptomatic bacteriuria or a positive urine culture in an otherwise asymptomatic child is unknown.
Zaoutis et al. Short-Course Therapy for Urinary Tract Infections in Children The SCOUT Randomized Clinical Trial. JAMA pediatrics. published online June 26, 2023.
Category: Pediatrics
Keywords: Pediatrics, preparedness (PubMed Search)
Posted: 4/5/2024 by Kathleen Stephanos, MD
(Updated: 4/12/2024)
Click here to contact Kathleen Stephanos, MD
In early 2023 Newgard et al published an article in JAMA which looked at pediatric readiness in ED's across the county. This study showed that there was a significant increase in pediatric mortality in patients who presented to EDs with lower readiness scores (<87 out of 100) when compared to those with higher readiness scores. And this translated to not just the time in the ED, but up to a year after they are seen in an ill-prepared ED. This number equated to an estimated total of 1,500 preventable deaths in children in the US each year.
Notably this does NOT look at what designation your hospital has for pediatrics (so being a level 1 pediatric trauma center does not automatically give you any points). This is based on having the physical materials needed for each age group, plans in place for specific patient age groups and evaluations (lower radiation doses for children in CT, using an US before CT for appendicitis evaluation, etc), and a person/people in place to review cases and ensure everyone is up to date on pediatric related training.
Want to check YOUR score? Go to https://www.pedsready.org/
Newgard CD, Lin A, Malveau S, et al. Emergency Department Pediatric Readiness and Short-term and Long-term Mortality Among Children Receiving Emergency Care. JAMA Netw Open. 2023;6(1):e2250941. doi:10.1001/jamanetworkopen.2022.50941
Category: Pediatrics
Keywords: pediatrics, sepsis, SIRS, septic shock (PubMed Search)
Posted: 4/5/2024 by Kelsey Johnson, DO
(Updated: 2/8/2026)
Click here to contact Kelsey Johnson, DO
Sepsis remains a leading cause of mortality in the pediatric population, and we have long been overdue for an update in recognizing and risk stratifying our pediatric patients.
Until now, pediatric sepsis screening guidelines have followed a framework modeled after the adult screening criteria from 2001 (Sepsis-2): Systemic Inflammatory Response Syndrome (SIRS). While attempts were made in 2005 to adjust these criteria to the pediatric population, data has shown poor specificity correlating to PICU admissions, need for critical interventions, end organ damage, and mortality.
As a reminder: Pediatric SIRS criteria: Temp >38.5 C or <36 C, tachycardia (or bradycardia if <1yr old), Tachypnea, leukocytosis/ leukopenia or >10% bandemia
In 2016, Sepsis-3 revised the criteria for sepsis and septic shock for the adult cohort by placing the focus on the presence of life-threatening organ dysfunction, which led to adopting criteria such as the SOFA and qSOFA scores to predict mortality risk.
Enter: The Phoenix Sepsis Score
An international, multidisciplinary task force convened by the Society of Critical Care Medicine in 2019 used evidence from an international survey, systematic review and meta-analysis to develop and validate a scoring tool intended to identify life-threatening organ dysfunction in children. Scoring tool was derived and validated retrospectively using an international, multi-center electronic medical record review of 3 million pediatric hospital encounters (excluding pre-term infants born <37 weeks and birth hospitalizations).
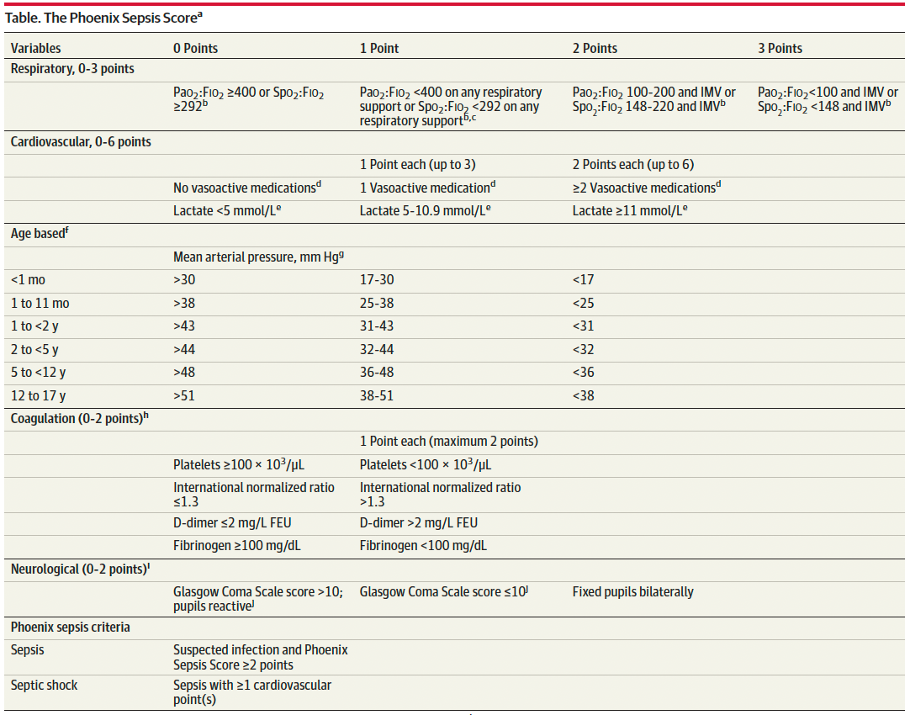
A Phoenix score of at least 2 carried a 7.1% risk of in-hospital mortality (in higher resource settings such as the USA).
Children with sepsis and organ dysfunction remote from the primary site of infection (eg respiratory failure in a child with meningitis) carried the highest mortality burden (8%) in this study.
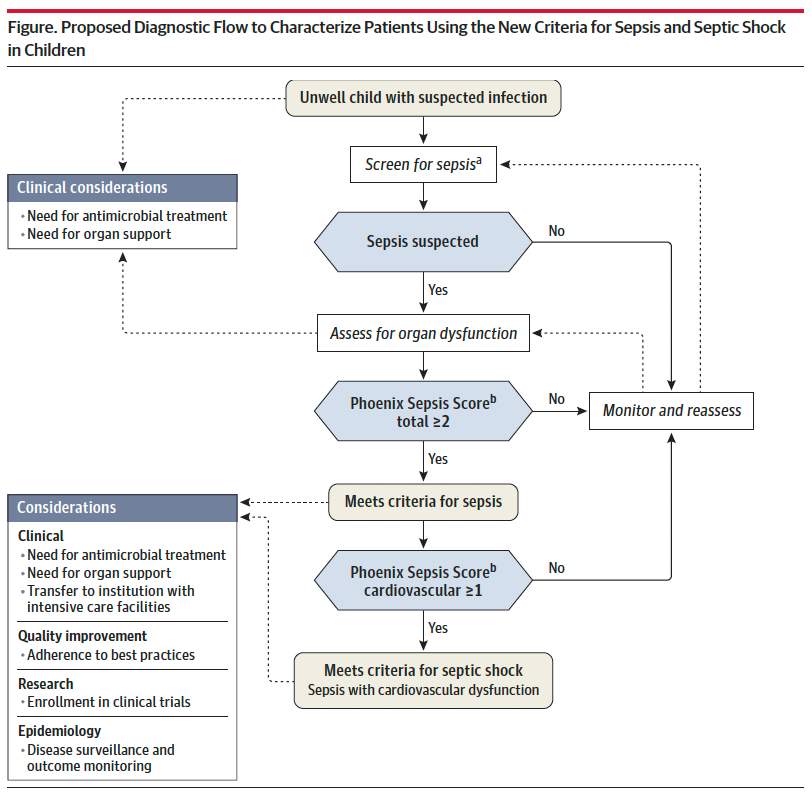
Sepsis is identified in children with suspected infection and an overall Phoenix score of 2 or more points, as this indicates potentially life-threatening organ dysfunction and thus carries higher mortality risk. Septic shock is identified by a score of 1 or more point(s) in cardiovascular dysfunction.
Lastly, it is important to recognize that this scoring criteria is NOT a sepsis screening tool, but rather should be applied when there is clinical suspicion for significant infection in the unwell child, or meeting sepsis screening criteria per your institutional criteria. Screening pediatric patients remains a clinical challenge, and there is not yet a reliable tool to apply to this population.
Bottom Line: Sepsis remains a significant cause of pediatric morbidity and mortality. The Phoenix Sepsis Score should be applied to the unwell child with suspected infection to identify sepsis and septic shock, thereby providing risk stratification and improving clinical care. Sepsis is defined by a Phoenix score of 2 or more and septic shock by a score of 1 or more in the cardiovascular category.
Schlapbach LJ, Watson RS, Sorce LR, et al. International Consensus Criteria for Pediatric Sepsis and Septic Shock. JAMA. 2024;331(8):665–674. doi:10.1001/jama.2024.0179
Category: Pediatrics
Posted: 3/29/2024 by Rachel Wiltjer, DO
Click here to contact Rachel Wiltjer, DO
Standard practice regarding various pediatric fractures has started to shift over the last several years, often to less restrictive means of treatment. Torus (buckle) fractures of the distal radius are one of the most common pediatric fractures and tend to heal very well with minimal intervention.
The FORCE study (FOrearm fracture Recovery in Children Evaluation), a multicenter study out of the UK, was conducted to compare rigid immobilization (splinting) to a soft bandage used as needed per family discretion for treatment of these fractures. There was no different in outcomes of self-reported pain, function, quality of life, complications, or school absences. UK orthopedic guidelines have been updated to reflect a recommendation against rigid immobilization as well as against any need for specialist follow-up. American guidelines are slower to follow suit, but in recent years have transitioned to an approach of a removable brace.
Take Home: Pediatric torus fractures of the distal radius likely do not require immobilization and can be managed with self-limited activity instead. Practice in the US is in flux, but it is reasonable to manage with a removable brace or soft dressing as well as pediatrician follow up.
Hussain, M, Perry, D, and Messahel, S. Summary of Recent Advances in Management of Torus Fracture of the Distal Radius in Children_. Arch Dis Child_. Epub ahead of print
Knight R, Dritsaki M, Mason J, Perry DC, Dutton SJ. The Forearm Fracture Recovery in Children Evaluation (FORCE) trial: statistical and health economic analysis plan for an equivalence randomized controlled trial of treatment for torus fractures of the distal radius in children. Bone Jt Open. 2020 Jun 9;1(6):205-213.
Category: Pediatrics
Keywords: Pediatric intubation, airway, cuffed, depth (PubMed Search)
Posted: 3/15/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
The gold standard for confirming ETT position is a chest xray, but this can often be delayed while the patient is stabilized. Many physicians will estimate ETT insertion depth to be 3x the ETT size, but this is based on selection of the correct tube. There are several other published formulas, including the PALS guidelines [age in years/2 + 12] which applies to children older than one year. In 1982, there was an article published that cited the formulas of [Height (cm) x 0.1 +5] or [Weight(kg)/5 + 12].
This was a retrospective study where the ideal position of cuffed ETT (from the front teeth) was determined by looking at post intubation xrays of 167 patients between 28 days and 18 years. The individual optimal ETT insertion depth was plotted against age, weight and height for all children. This study showed that there is not a fully linear relationship between age, height or weight which is a flaw of all of these formulas. Calculations using the patients’ weight performed the worst. Age based and height formulas performed the best.
Ebenebe et al. Recommendations for endotracheal tube insertion depths in children. Emerg Med J 2023; 0:1-5. epub ahead of print.
Category: Pediatrics
Posted: 2/29/2024 by To-Lam Nguyen, MD
(Updated: 3/1/2024)
Click here to contact To-Lam Nguyen, MD
You've heard of one kill pills such as calcium channel blockers, beta blockers, sulfonylureas, anti-malarials, but less commonly known is benzonatate, or tessalon perles.
Tessalon perles are not recommended for children under the age of 10. 1-2 capsules of benzonatate in children <2 years old have been reported to cause serious side effects including restlessness, tremors, convulsions, coma and even cardiac arrest rapidly after ingestion (within 15-20 minutes and death within a couple of hours). It is attractive to young children as it somewhat resembles a jelly bean.
Pearls on Tessalon Perles:
https://www.poison.org/articles/are-benzonatate-capsules-poisonous
Thimann DA, Huang CJ, Goto CS, Feng SY. Benzonatate toxicity in a teenager resulting in coma, seizures, and severe metabolic acidosis. J Pediatr Pharmacol Ther. 2012 Jul;17(3):270-3. doi: 10.5863/1551-6776-17.3.270. PMID: 23258970; PMCID: PMC3526931.
Category: Pediatrics
Keywords: myositis, acute kidney injury, problems walking, calf pain (PubMed Search)
Posted: 2/14/2024 by Jenny Guyther, MD
(Updated: 2/16/2024)
Click here to contact Jenny Guyther, MD
BACM stands for benign acute childhood myositis which is typically a benign, viral induced self limiting illness. This was a retrospective study looking at 65 patients in Italy to further characterize the characteristics of the disease.
In this study, the median patient age was 6 years with a male predominance. The incidence of BACM peaked in winter with a second peak in the fall. Patients presented with prodromal symptoms including fever, cough, coryza, sore throat and vomiting. The exam showed difficulty walking and myalgias with reproducible calf tenderness and preserved reflexes. Influenza B and A, COVID and other viral pathogens have been detected in these patients.
Lab work may show an elevated creatinine kinase, AST and potassium. WBC and CRP may also be elevated. The median CK value was 943 U/L and on average normalized within one week. Other studies have shown median CK values in the 3300s. Treatment includes hydration to promote CK clearance and prevent complications including acute kidney injury related to rhabdomyolysis. Recurrent myositis or CK values > 5000 U/L should have screening tests for muscular dystrophy and metabolic disorders.
Attainaese et al. Benign acute children myositis: 5 year experience in a tertiary pediatric hospital. European Journal of Pediatrics, published online July 18 2023.
Category: Pediatrics
Keywords: pediatrics, fever, neonate, preterm (PubMed Search)
Posted: 2/9/2024 by Kathleen Stephanos, MD
Click here to contact Kathleen Stephanos, MD
It is an often asked question: should I consider the corrected or the chronologic age when determining the need for fever evaluation in a pediatric patient? The 2021 AAP guidelines for the well appearing febrile neonate are widely accepted and apply to neonates under 60 days. These highly practical guidelines are, unfortunately, not applicable to pre-term neonates. The question often becomes what age to use for a pre-term neonate- the age they actually are, or the age they would be if they had completed a full term gestation.
Hadhud et al attempted to clarify the age utilized in a retrospective review. This looked at febrile 448 pre-term neonates evaluated for fevers. It found that those patients with both a corrected and chronologic age over 3 months had a 2.6% rate of serious bacterial infections or SBI (UTI, bacteremia or meningitis), those with a corrected age under 3 months but a chronologic age over 3 months had a 16.7% rate of SBIs, and those with both a corrected and chronologic age of under 3 months had a 33.3% rate of SBI.
Overall, these rates of infection are higher than the typically reported in febrile neonates, supporting that pre-term neonates have a much higher risk of infections overall. Ultimately, pre-term neonates should be carefully assessed and a more thorough evaluation is typically warranted in this patient population even if they have reached the generally accepted 60 day marker by chronologic age- use the corrected age.
Hadhud M, Gross I, Hurvitz N, Ohana Sarna Cahan L, Ergaz Z, Weiser G, Ofek Shlomai N, Eventov Friedman S, Hashavya S. Serious Bacterial Infections in Preterm Infants: Should Their Age Be "Corrected"? J Clin Med. 2023 May 1;12(9):3242. doi: 10.3390/jcm12093242. PMID: 37176683; PMCID: PMC10178985.
Category: Pediatrics
Keywords: Bouncebacks, high risk discharges, gastroenteritis, death (PubMed Search)
Posted: 1/19/2024 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Revisits back to the ED within 3 days of the initial visit represent a standard quality measure. A critical ED revisit was defined as an ICU admission or death within 3 days of ED discharge. This study looked at 16.3 million children who were discharged from various EDs over a 4 year period and found that 0.1% (18,704 patients) had a critical revisit and 0.00001% (180 patients) died.
The most common diagnosis at the initial visit of those patients coming back with a critical revisit included: Upper respiratory infections, gastroenteritis/nausea/vomiting and asthma.
The most common critical revisit diagnosis were: asthma, pneumonia, cellulitis, bronchiolitis, upper respiratory infections, respiratory failure, seizure, gastroenteritis/nausea/vomiting, appendectomy and sickle cell crisis. Among the patients who died, 48.9% were younger than 4 years. Patients with complex medical problems and patients seen at a high volume center were more likely to have a critical ED visit.
Bottom line: These ED revisits may not have been related to missed diagnosis (with the exception of appendicitis), but rather due to the natural progression of certain disease processes. Patients with these diagnoses may benefit from careful reassessment, targeted patient education, more specific return precautions and closer outpatient follow up.
Cavallaro et al. Critical Revisits Among Children After Emergency Department Discharge. Annals of Emergency Medicine. 2023. epub ahead of print.
Category: Pediatrics
Keywords: fever, SBI, infants (PubMed Search)
Posted: 12/15/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Urinary tract infection (UTI) is the leading cause of fever without a source in infants younger than 3 months. This data was collected from patients who presented to the emergency department with fever without a source over a 16 year period. Out of 2850 patients, 20.8% were diagnosed with a UTI, the majority of which grew E coli. Of those patients who were diagnosed with UTI, these patients were more likely to have a history of renal/GU problems, have a fever of at least 39C (38% vs 29%) or poor feeding (13% vs 8.7%). However, 48% had none of these risk factors. Also 6.1% of patients with a febrile UTI had another invasive bacterial infection. These patients were more likely to be < 1 month, be "irritable" per parents and have an elevated procalcitonin and CRP.
Bottom line: A lack of risk factors can not exclude a UTI in febrile infants < 3 months. A diagnosis of UTI also does not definitively exclude an additional invasive bacterial infection in a subset of these children.
Lejarzegi, Ainara MD*; Fernandez-Uria, Amaia MD*; Gomez, Borja MD, PhD*; Velasco, Roberto MD, PhD†; Benito, Javier MD, PhD*; Mintegi, Santiago MD, PhD*. Febrile Urinary Tract Infection in Infants Less Than 3 Months of Age. The Pediatric Infectious Disease Journal ():10.1097/INF.0000000000003947, April 24, 2023. | DOI: 10.1097/INF.0000000000003947
Category: Pediatrics
Posted: 12/1/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
Since Christmas is coming up, let's talk about Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency, also known as Christmas disease)
Deficiencies in Factors VIII and IX are the most common severe inherited bleeding disorders.
Pathophysiology:
Clinical Manifestations:
Lab findings and diagnosis
Genetics
Classification
trauma to induce bleeding
Treatment
Summary:
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 1, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Category: Pediatrics
Posted: 12/1/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
Since Christmas is coming up, let's talk about Hemophilia A (factor VIII deficiency) and Hemophilia B (factor IX deficiency, also known as Christmas disease)
Deficiencies in Factors VIII and IX are the most common severe inherited bleeding disorders.
Pathophysiology:
Clinical Manifestations:
Lab findings and diagnosis
Genetics
Classification
trauma to induce bleeding
Treatment
Summary:
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 2, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Kliegman R, Stanton B, St. Geme JW, Schor NF, Behrman RE. Nelson Textbook of Pediatrics. Edition 20. Elsevier; 2016. Accessed December 2, 2023. https://search.ebscohost.com/login.aspx?direct=true&db=cat01362a&AN=hshs.004567758&site=eds-live
Category: Pediatrics
Keywords: POCUS, Pediatrics, Lung Ultrasound, Bronchiolitis (PubMed Search)
Posted: 11/20/2023 by Alexis Salerno Rubeling, MD
Click here to contact Alexis Salerno Rubeling, MD
Acute bronchiolitis (AB) is a common cause of respiratory tract infections in infants. A recent study looked at the application of Point-of-Care Lung Ultrasound (LUS) in infants <12 months who presented with symptoms of AB.
They scored infant lungs using a cumulative 12-zone system. With the below scale:
0 - A lines with <3 B lines per lung segment.
1 - ≥3 B lines per lung segment, but not consolidated.
2 - consolidated B lines, but no subpleural consolidation.
3 - subpleural consolidation with any findings scoring 1 or 2.
They found that infants with higher LUS scores had increased rates of hospitalization and length of stay.
Here are some tips for ultrasounding a pediatric patient:
Smith JA, Stone BS, Shin J, Yen K, Reisch J, Fernandes N, Cooper MC. Association of outcomes in point-of-care lung ultrasound for bronchiolitis in the pediatric emergency department. Am J Emerg Med. 2023 Oct 21;75:22-28. doi: 10.1016/j.ajem.2023.10.019. Epub ahead of print. PMID: 37897916.
Category: Pediatrics
Keywords: pediatric trauma, transport, time to destination (PubMed Search)
Posted: 11/17/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Hosseinpour H. Interfacility Transfer of Pediatric Trauma to Higher Levels of Care: The Effect of Transfer Time and Level of Receiving Trauma Care. Journal of Trauma and Acute Care Surgery. Epub ahead of print.
Category: Pediatrics
Keywords: Neonate, Newborn, resuscitation, NRP (PubMed Search)
Posted: 11/3/2023 by Kelsey Johnson, DO
(Updated: 2/8/2026)
Click here to contact Kelsey Johnson, DO
Term? Tone? Tantrum?
Immediately after delivery, your initial neonatal assessment should evaluate for:
- Appearance of full or late pre-term gestation (>34 weeks)
- Appropriate tone (flexed extremities, not floppy)
- Good cry and respiratory effort
Newborns meeting this criteria should not require resuscitation. They can be placed skin to skin on mother and allowed to breastfeed. Delayed cord clamping for 60 seconds is recommended, as data shows improved neurodevelopmental outcomes and iron stores in first year of life.
Neonates not meeting these criteria should be brought to the warmer for resuscitation, with the focus being on:
- Warm - via radiant warmer. Maintain temps 36.5 C – 37.5 C
- Dry - Neonates have thin skin and lose heat readily from evaporative loses
- Stim - tactile stimulation on the head, midline of the back and extremities to provoke a cry and encourage respiratory effort
Avoid routinely bulb-suctioning unless there is significant obstructing mucous, as this can increase vagal tone and result in bradycardia. If bulb suctioning is used, first suction the mouth before the nose.
Majority of resuscitations do not require additional support, however if heart rate is <100 or there is poor respiratory effort, the physician should initiate PPV.
PPV settings: PIP 20 PEEP 5 FiO2 21% Rate of 60 breaths per minute
Improvement in the neonate’s HR is the primary indicator of effective PPV!
If HR poorly responding (remains <100), ensure appropriate mask size, reposition, suction, and increase PIP (max 35) and FiO2.
If HR drops below 60, intubate with uncuffed ETT
- Prioritize adequate ventilation as this is the highest priority in neonatal resuscitation
- Initiate compressions at rate of 120/min.
- Epi dosing is 0.01-0.03 mg/kg q3-5 min
- ETT size estimation by gestational age:
25 weeks = 2.5, 30 weeks = 3.0, 35 weeks = 3.5, 40 weeks = 4.0
Category: Pediatrics
Keywords: trauma arrest, ROSC, blunt, penetrating (PubMed Search)
Posted: 10/20/2023 by Jenny Guyther, MD
(Updated: 2/8/2026)
Click here to contact Jenny Guyther, MD
Selesner L, Yorkgitis B, Martin M, et al. Emergency department thoracotomy in children: A Pediatric Trauma Society, Western Trauma Association, and Eastern Association for the Surgery of Trauma systematic review and practice management guideline. J Trauma Acute Care Surg. 2023;95(3):432-441. doi:10.1097/TA.
Category: Pediatrics
Posted: 10/6/2023 by To-Lam Nguyen, MD
Click here to contact To-Lam Nguyen, MD
- Magnets move through the GI tract at different rates and become lodged in adjacent loops of intestine. Adjacent bowel segments can stick together when the magnets attract each other through the bowel walls which can cause obstruction, perforation, fistula formation, and necrotic bowel.
- Obtain xray to identify ingested metallic object(s)
- Any object lodged in the esophagus should be emergently removed by a pediatric gastroenterologist.
- Once an object is past the stomach and beyond the reach of endoscopy, affected patients need to be watched carefully for signs of obstruction or peritonitis, either occurrence requiring the prompt consultation of a pediatric surgeon.
- Enhancement of magnet movement through the GI tract may be aided by a laxative such as polyethylene glycol, but there is no clear data that this approach speeds the passage of the magnet. There is no clear guidance on how frequently to obtain abdominal radiographs to determine movement or passage of ingested magnets.
- More frequently lodge in esophagus due to seize and cause electric urn on contact
- Complications include perforation or fistula formation
- Honey or liquid ulcer medication carafate can slow extent of esophageal injury
- Current recommendations from National Button Battery Hotline: caregiver to give 2 teaspoons of honey every 10 minutes while en route to hospital
- Causes caustic contact to vocal cords, which leads to acute laryngospasm
- Airway compromise, if to occur, occurs rapidly. If after brief obs period, it does not appear, it is very unlikely to be a late occurance.
- Corrosive on GI tract. pH of detergents range from 7-9.
- Any child with difficulty swallowing, drooling, stridor, and recurrent vomiting should have GI consulted for endoscopy
Tiki Torch Oil
- Tiki torch oil looks like apple juice (the container looks similar too)
- Lamp oil ingestion (hydrocarbons) can cause excessive drowsiness, lung injury, difficulty breathing
- Preventing accidental tiki torch oil ingestion: NEVER use torch fuels near area where food or drinks are served, keep out of reach and out of sight of young children, and only buy bottle of torch fuels with child-resistant cap and make sure to replace cap securely after every single use
Hydrogen Peroxide
- 35% hydrogen peroxide has become more popular as food-grade or nutraceutical product (food additive purportedly used for medicinal purposes)
- When hydrogen peroxide reacts with HCl in the stomach, it liberates large volumes of oxygen causing immediate frothy emesis and systemic absorption of oxygen. Gastric oxygen, once absorbed, passes through the portal vein to liver causing gas embolisms in liver
- Preferred evaluation of kids with known ingestion and acute vomiting should image by noncontrast limited upper abdominal CT (to reduce radiation exposure) to assess bubble burden.
- There is no consensus on what is considered a significant air embolism burden that would require hyperbaric treatment
- A single tablet of buprenorphine, or a single dissolvable gel strip of its formulation as Suboxone has been lethal to children.
- Prescribing intranasal naloxone spray to the family of patients on buprenorphine (and methadone as well) is potentially lifesaving to the patient, should they take too much, but also for children in their homes who may accidentally eat a single tablet or chew on what appears to be a “gummy” product, a dissolvable formulation of Suboxone.
- Pediatricians doing anticipatory safety guidance to parents at the 9-month-old to 1-year-old health supervision visit should ask about opiates and medication-assisted therapy present in the home or used by caregivers (especially grandparents) and should offer to write a prescription for naloxone nasal spray
https://publications.aap.org/pediatricsinreview/article/42/1/2/35444/Pediatric-Ingestions-New-High-Risk-Household
