Category: Pediatrics
Keywords: pediatrics, sepsis, SIRS, septic shock (PubMed Search)
Posted: 4/5/2024 by Kelsey Johnson, DO
(Updated: 2/7/2026)
Click here to contact Kelsey Johnson, DO
Sepsis remains a leading cause of mortality in the pediatric population, and we have long been overdue for an update in recognizing and risk stratifying our pediatric patients.
Until now, pediatric sepsis screening guidelines have followed a framework modeled after the adult screening criteria from 2001 (Sepsis-2): Systemic Inflammatory Response Syndrome (SIRS). While attempts were made in 2005 to adjust these criteria to the pediatric population, data has shown poor specificity correlating to PICU admissions, need for critical interventions, end organ damage, and mortality.
As a reminder: Pediatric SIRS criteria: Temp >38.5 C or <36 C, tachycardia (or bradycardia if <1yr old), Tachypnea, leukocytosis/ leukopenia or >10% bandemia
In 2016, Sepsis-3 revised the criteria for sepsis and septic shock for the adult cohort by placing the focus on the presence of life-threatening organ dysfunction, which led to adopting criteria such as the SOFA and qSOFA scores to predict mortality risk.
Enter: The Phoenix Sepsis Score
An international, multidisciplinary task force convened by the Society of Critical Care Medicine in 2019 used evidence from an international survey, systematic review and meta-analysis to develop and validate a scoring tool intended to identify life-threatening organ dysfunction in children. Scoring tool was derived and validated retrospectively using an international, multi-center electronic medical record review of 3 million pediatric hospital encounters (excluding pre-term infants born <37 weeks and birth hospitalizations).
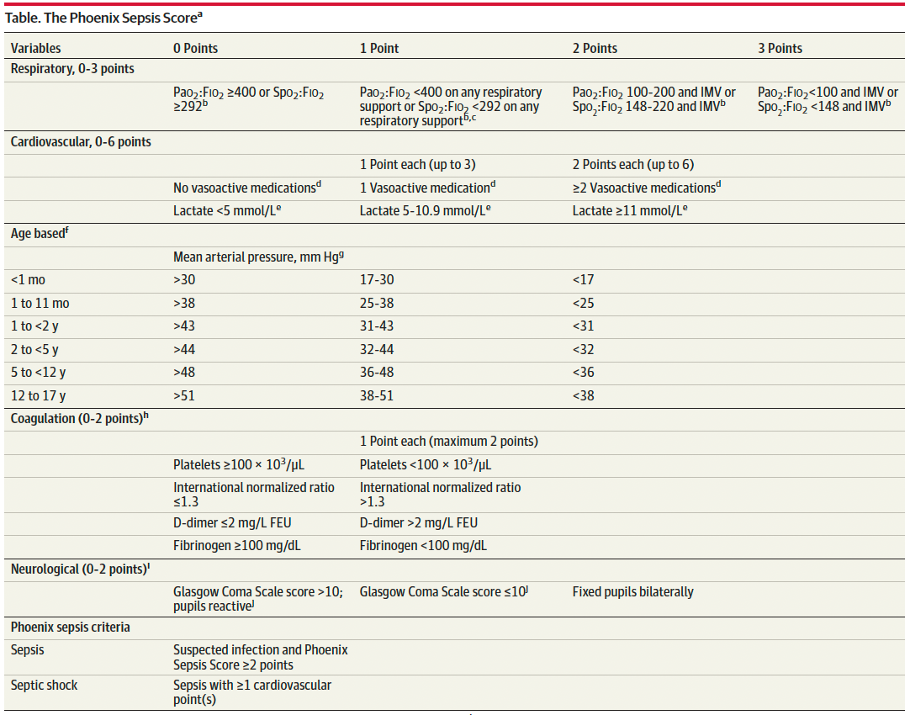
A Phoenix score of at least 2 carried a 7.1% risk of in-hospital mortality (in higher resource settings such as the USA).
Children with sepsis and organ dysfunction remote from the primary site of infection (eg respiratory failure in a child with meningitis) carried the highest mortality burden (8%) in this study.
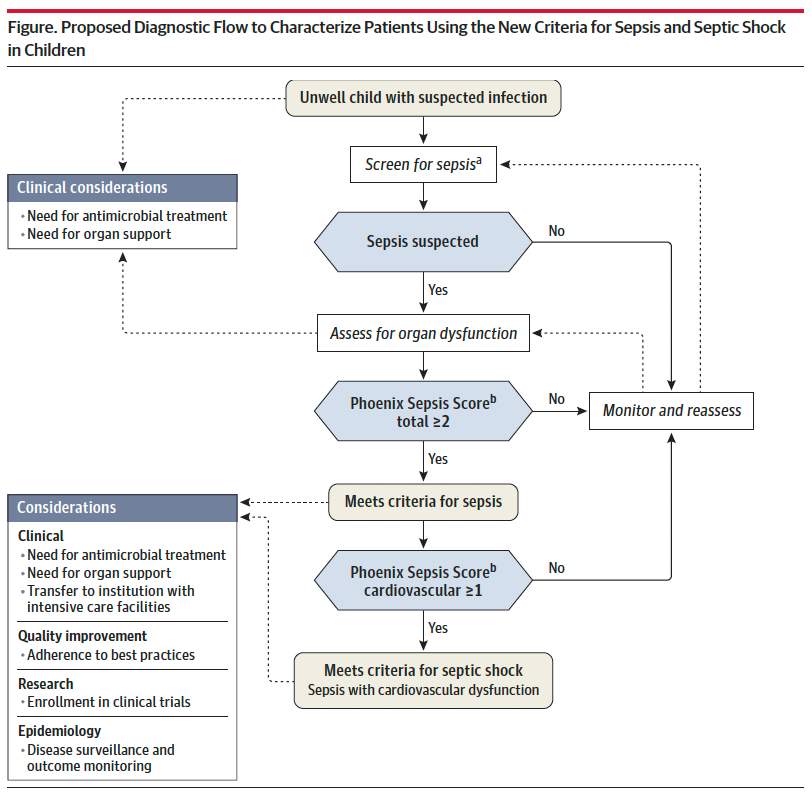
Sepsis is identified in children with suspected infection and an overall Phoenix score of 2 or more points, as this indicates potentially life-threatening organ dysfunction and thus carries higher mortality risk. Septic shock is identified by a score of 1 or more point(s) in cardiovascular dysfunction.
Lastly, it is important to recognize that this scoring criteria is NOT a sepsis screening tool, but rather should be applied when there is clinical suspicion for significant infection in the unwell child, or meeting sepsis screening criteria per your institutional criteria. Screening pediatric patients remains a clinical challenge, and there is not yet a reliable tool to apply to this population.
Bottom Line: Sepsis remains a significant cause of pediatric morbidity and mortality. The Phoenix Sepsis Score should be applied to the unwell child with suspected infection to identify sepsis and septic shock, thereby providing risk stratification and improving clinical care. Sepsis is defined by a Phoenix score of 2 or more and septic shock by a score of 1 or more in the cardiovascular category.
Schlapbach LJ, Watson RS, Sorce LR, et al. International Consensus Criteria for Pediatric Sepsis and Septic Shock. JAMA. 2024;331(8):665–674. doi:10.1001/jama.2024.0179
Category: Pediatrics
Keywords: Neonate, Newborn, resuscitation, NRP (PubMed Search)
Posted: 11/3/2023 by Kelsey Johnson, DO
(Updated: 2/7/2026)
Click here to contact Kelsey Johnson, DO
Term? Tone? Tantrum?
Immediately after delivery, your initial neonatal assessment should evaluate for:
- Appearance of full or late pre-term gestation (>34 weeks)
- Appropriate tone (flexed extremities, not floppy)
- Good cry and respiratory effort
Newborns meeting this criteria should not require resuscitation. They can be placed skin to skin on mother and allowed to breastfeed. Delayed cord clamping for 60 seconds is recommended, as data shows improved neurodevelopmental outcomes and iron stores in first year of life.
Neonates not meeting these criteria should be brought to the warmer for resuscitation, with the focus being on:
- Warm - via radiant warmer. Maintain temps 36.5 C – 37.5 C
- Dry - Neonates have thin skin and lose heat readily from evaporative loses
- Stim - tactile stimulation on the head, midline of the back and extremities to provoke a cry and encourage respiratory effort
Avoid routinely bulb-suctioning unless there is significant obstructing mucous, as this can increase vagal tone and result in bradycardia. If bulb suctioning is used, first suction the mouth before the nose.
Majority of resuscitations do not require additional support, however if heart rate is <100 or there is poor respiratory effort, the physician should initiate PPV.
PPV settings: PIP 20 PEEP 5 FiO2 21% Rate of 60 breaths per minute
Improvement in the neonate’s HR is the primary indicator of effective PPV!
If HR poorly responding (remains <100), ensure appropriate mask size, reposition, suction, and increase PIP (max 35) and FiO2.
If HR drops below 60, intubate with uncuffed ETT
- Prioritize adequate ventilation as this is the highest priority in neonatal resuscitation
- Initiate compressions at rate of 120/min.
- Epi dosing is 0.01-0.03 mg/kg q3-5 min
- ETT size estimation by gestational age:
25 weeks = 2.5, 30 weeks = 3.0, 35 weeks = 3.5, 40 weeks = 4.0
