Category: Trauma
Posted: 5/12/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Hemodynamic instability in trauma patients is most often associated with hemorrhagic shock, however, there is an entity known as brain injury associated shock (BIAS). BIAS is thought to be associated with catecholamine surges secondary to brain injury. BIAS is found in both isolated head injury pts as well as multi-trauma patients. Studies have identified BIAS in 13% of adult trauma patients and up to 40% of pediatric major trauma patients.
We know hypotension in brain injury worsens outcome. We should assume hemorrhagic etiology until we prove otherwise. Once we suspect BIAS and have excluded hemorrhagic etiology our strategy should switch to blood pressure support using non-blood product management.
Partyka C, Alexiou A, Williams J, Bliss J, Miller M, Ferguson I. Brain Injury Associated Shock: An Under-Recognized and Challenging Prehospital Phenomenon. Prehospital and Disaster Medicine. Published online 2024:1-6. doi:10.1017/S1049023X24000359
Category: Trauma
Keywords: trauma, blunt, cardiac injury, shock, thoracic (PubMed Search)
Posted: 5/5/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
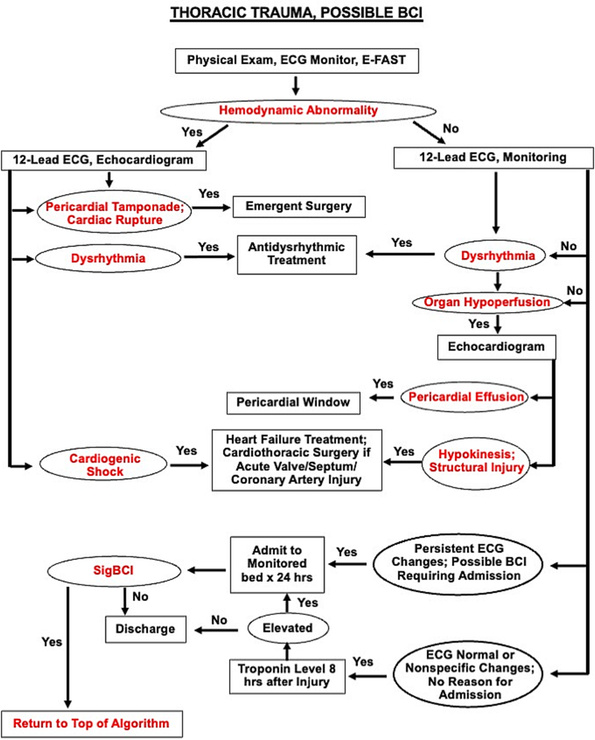
Blunt Cardiac Injury is a continuum from asymptomatic, not clinically relevant to catastrophic, life ending disease . Consider blunt cardiac injury in patients with significant force to the chest wall or sudden deceleration injuries (motor vehicle crashes, motorcycle crashes, falls from height etc.). This algorithm is helpful when working up patients suspected of having significant blunt cardiac injury.
Biffl, Walter L. MD; Fawley, Jason A. MD; Mohan, Rajeev C. MD. Diagnosis and management of blunt cardiac injury: What you need to know. Journal of Trauma and Acute Care Surgery 96(5):p 685-693, May 2024. | DOI: 10.1097/TA.0000000000004216
Category: Trauma
Posted: 4/24/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
A small study retrospectively looking at recorded calls to a level 1 trauma center transfer line specifically looking at patients who died or were discharged to hospice without surgical intervention found only 10% had goals of care discussed prior to transfer. Most were brain hemorrhage patients.
As a transferring facility, clearly outlining goals of care and addressing futility of care can have a major impact on trauma transfers and the cost and family burden associated with transfers.
Trenga-Schein, Nellie BA; Zonies, David MD, MPH, MBA, FACS, FCCM, FACHE; Cook, Mackenzie MD, FACS
Journal of Trauma and Acute Care Surgery 96(4):p 583-588, April 2024. | DOI: 10.1097/TA.0000000000004215
Category: Trauma
Posted: 4/21/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
PECARN has a decision tool to identify blunt trauma patients under age 18 who are low probability for important intra-abdominal injuries. The questions to ask are:
Answering no to all yields <0.1% chance of intra-abdominal trauma requiring intervention. (See MedCalc link for other calculations)
A prospective validation study in the Lancet yielded 100% sensitivity and negative predictive value in 7542 patients under age 18
This tool can likely be used to guide imaging choices in pediatric blunt abdominal trauma patients
Category: Trauma
Posted: 4/14/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This study looked at survival pre and post implementation of an airway guideline for prehospital traumatic brain injury (TBI) patients who received positive pressure airway interventions. The guideline “focused on the avoidance and aggressive treatment of hypotension and 3 airway-related goals: (1) prevention or treatment of hypoxia through early, high-flow oxygen administration; (2) airway interventions to optimize oxygenation or ventilation when high-flow oxygen was insufficient; and (3) prevention of hyperventilation or hypocapnia by using ventilation adjuncts (ie, rate timers, flow-controlled ventilation bags, end-tidal carbon dioxide monitoring).”
Post implementation, survival to admission increased in all severity levels of TBI and in the most severely injured, survival to discharge improved.
Useful for those involved in prehospital education and as a reminder for in hospital airway management in TBI patients.
Gaither JB, Spaite DW, Bobrow BJ, et al. EMS Treatment Guidelines in Major Traumatic Brain Injury With Positive Pressure Ventilation. JAMA Surg. 2024;159(4):363–372. doi:10.1001/jamasurg.2023.7155
Category: Trauma
Keywords: Trauma, blood pressure, shock index, predictor, mortality (PubMed Search)
Posted: 4/8/2024 by Robert Flint, MD
Click here to contact Robert Flint, MD
Traditionally, a systolic blood pressure (SBP) of 90 has been used as a marker of severe illness in trauma patients. This study looked at a large database and found shock index (SI) and systolic blood pressure were the best predictors of early mortality in trauma patients.
They found:
prehospital SI 0.9 and SBP 110,
ED SI 0.9 and SBP 112,
and
in elderly
prehospital SI 0.8 SBP 116
ED SI 0.8 SBP 121
were the cutoffs to predict early mortality.
We should rethink our protocols and approach to trauma patients using a higher systolic blood pressure than 90. Also note elderly had a different number than younger trauma patients.
April MD, Fisher AD, Rizzo JA, Wright FL, Winkle JM, Schauer SG. Early Vital Sign Thresholds Associated with 24-Hour Mortality among Trauma Patients: A Trauma Quality Improvement Program (TQIP) Study. Prehosp Disaster Med. 2024 Apr 2:1-5. doi: 10.1017/S1049023X24000207. Epub ahead of print. PMID: 38563282.
Category: Trauma
Keywords: Marker, penetrating trauma, radiopaque (PubMed Search)
Posted: 4/7/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Using radiopaque markers such as paperclips to mark penetrating wounds prior to radiographs has been taught in trauma bays for decades. This article points out there is no evidence to support this practice and is purely based on expert opinion. With the heavy use of CT imaging to assess wound tracks, the use of markers on plain films appears to be of limited utility.
Sarfaraz K, Nemeth J, Bahreini M. The use of radiopaque markers is medical dogma. Acad Emerg Med. 2024 Feb;31(2):193-194. doi: 10.1111/acem.14858. Epub 2024 Feb 6. PMID: 38112251.
Category: Trauma
Keywords: Alcohol, withdrawal, trauma, protocol, sparing (PubMed Search)
Posted: 3/24/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This study compared admitted trauma patients with alcohol withdrawal or those at risk of withdrawal before and after a benzodiazepine sparing protocol (using clonidine and gabapentin) was initiated. They found a lower daily CIWA score and significantly less lorazepam use in the benzodiazepines sparing group. This sparing protocol appears to be safe and effective.
McCullough, Mary Alyce MD; Miller, Preston R. III MD; Martin, Tamriage MD; Rebo, Kristin A. PharmD; Stettler, Gregory R. MD; Martin, Robert Shayn MD; Cantley, Morgan PharmD; Shilling, Elizabeth H. PhD; Hoth, James J. MD, PhD; Nunn, Andrew M. MD
Journal of Trauma and Acute Care Surgery 96(3):p 394-399, March 2024. | DOI: 10.1097/TA.0000000000004188
Category: Trauma
Keywords: Geriatric trauma, outcome, hospice (PubMed Search)
Posted: 3/17/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This was a database study of nearly 2 million trauma patients over age 65 who were discharged looking at all levels of trauma centers. The authors found:
“Dominance analysis showed that proportion of patients with Injury Severity Score of >15 contributed most to explaining hospice utilization rates (3.2%) followed by trauma center level (2.3%), proportion White(1.9%), proportion female (1.5%), and urban/rural setting (1.4%).”
Level one centers had the lowest level of discharge to hospice. The authors felt: “As the population ages, accurate assessment of geriatric trauma outcomes becomes more critical. Further studies are needed to evaluate the optimal utilization of hospice in end-of-life decision making for geriatric trauma.”
Fakhry, Samir M. MD, FACS; Shen, Yan PhD; Wyse, Ransom J. MPH; Garland, Jeneva M. PharmD; Watts, Dorraine D. PhD
Journal of Trauma and Acute Care Surgery 94(4):p 554-561, April 2023. | DOI: 10.1097/TA.0000000000003883
Category: Trauma
Posted: 3/10/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This secondary analysis of the NEXUS head injury data found patients over 65:
-sustained more significant injuries than younger pts
-presented more frequently with occult injuries
-when they required neurosurgery intervention only 16% went home, 32% were discharged to rehab facility and 41% died
-mechanism of injury was most commonly fall from standing
-mortality rates were highest for fall from ladder and auto vs. pedestrian injuries
The authors concluded: “Older blunt head injury patients are at high risk of sustaining serious intracranial injuries even with low-risk mechanisms of injury, such as ground-level falls. Clinical evaluation is unreliable and frequently fails to identify patients with significant injuries. Outcomes, particularly after intervention, can be poor, with high rates of long-term disability and mortality.”
William R. Mower, Thomas E. Akie, Naseem Morizadeh, Malkeet Gupta, Gregory W. Hendey, Jake L. Wilson, Lorenzo Pierre Leonid Duvergne, Phillip Ma, Pravin Krishna, Robert M. Rodriguez,
Blunt Head Injury in the Elderly: Analysis of the NEXUS II Injury Cohort,
Annals of Emergency Medicine,
2024,
Category: Trauma
Posted: 3/3/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This is a retrospective study looking at traumatic brain injury patients comparing those with and without pre-existing psychiatric illness at the time of injury. Those with pre-existing illness had longer hospital stays, longer ICU stays and more frequent readmissions.
Benavides F, Liporaci J, Getchell J, et al. Effects of pre-existing psychiatric illness on traumatic brain injury outcomes: A propensity-matched cohort study. Trauma. 2024;0(0). doi:10.1177/14604086231187157
Category: Trauma
Posted: 2/29/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This meta analysis did not find convincing evidence for or against seizure prophylaxis for admitted moderate to severe traumatic brain injury pts. They recommend Levetiracetam over other medications again on weak evidence.
Frontera, J.A., Gilmore, E.J., Johnson, E.L. et al. Guidelines for Seizure Prophylaxis in Adults Hospitalized with Moderate–Severe Traumatic Brain Injury: A Clinical Practice Guideline for Health Care Professionals from the Neurocritical Care Society. Neurocrit Care(2024). https://doi.org/10.1007/s12028-023-01907-x
Category: Trauma
Keywords: Hip fracture l, hemoglobin l, mortality (PubMed Search)
Posted: 2/25/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
In this study, geriatric hip fracture patients with a hemoglobin less than 7.1 had higher mortality, especially in those over age 79, even when controlling for other factors such as ASA Physical status class, anti-platelet use, etc.
Bruce K, Mangram A, Sucher JF_, et al_
Consequences of anemia in geriatric hip fractures: how low is too low?
Trauma Surgery & Acute Care Open 2024;**9:**e001175. doi:10.1136/tsaco-2023-001175
Category: Trauma
Keywords: Pelvic binder, trauma, survival, mortality (PubMed Search)
Posted: 2/18/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This retrospective study of 66 trauma patients who had pelvic fractures attempted to determine if prehospital applied pelvic binders had an impact on mortality. There were 3 cohorts: appropriately applied binders (14), inappropriately applied (14 not at the level of the greater trochanter), and none applied (38). Survival for applied was 92% and those without was 81% which was not statistically significant. The authors concluded: “In conclusion, our study found that the use of prehospital pelvic binders did not show a significant effect on patient outcomes for those with unstable pelvic fractures. Instead, injury severity score (ISS) emerged as the most significant predictor of survival.”
Previous studies have shown regular education is needed on proper use of binders. We should continue to educate on appropriate positioning and the use of pelvic binders. For me, this study is not large enough to convince that we should go away from binder use. We need more data before we abandon the pelvic binder.
Alonja Reiter, André Strahl, Sarina Kothe, Markus Pleizier, Karl-Heinz Frosch, Konrad Mader, Annika Hättich, Jakob Nüchtern, Christopher Cramer,
Does a prehospital applied pelvic binder improve patient survival?,
Injury,
2024,
111392,
ISSN 0020-1383,
Category: Trauma
Keywords: Ct, head injury, geriatric (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/4/2024)
Click here to contact Robert Flint, MD
In this prospective study looking at geriatric patients with unknown head injury vs. known head injury, the unknown head injury group had an ICH 1.5%, neurosurgical intervention 0.3% and delayed ICH 0.1% when compared to known head injury (10.5%, 1.2% and 0.7% respectively). The authors concluded that the risk of ICH was high enough in uncertain head injury patients to warrant scanning.
Turchiaro ML Jr, Solano JJ, Clayton LM, Hughes PG, Shih RD, Alter SM. Computed Tomography Imaging of Geriatric Patients with Uncertain Head Trauma. J Emerg Med. 2023 Dec;65(6):e511-e516. doi: 10.1016/j.jemermed.2023.07.009. Epub 2023 Jul 26. PMID: 37838489.
Category: Trauma
Keywords: Prediction, surprise question, trauma, mortality (PubMed Search)
Posted: 1/28/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
The question “Would I be surprised if the patient died within the next year” has been validated as a tool to predict patients with a limited life expectancy. This study looked at trauma team members’ ability to use this question to predict one year mortality. Trauma team members over estimated mortality in this study.
Hoffman, Melissa Red MD, ND; Slivinski, Andrea DNP, APRN; Shen, Yan PhD; Watts, Dorraine D. PhD; Wyse, Ransom J. MPH; Garland, Jeneva M. PharmD; Fakhry, Samir M. MD, FACS; the Surprise Question in Trauma Research Group. Would you be surprised? Prospective multicenter study of the Surprise Question as a screening tool to predict mortality in trauma patients. Journal of Trauma and Acute Care Surgery 96(1):p 35-43, January 2024. | DOI: 10.1097/TA.0000000000004151
Category: Trauma
Keywords: elder, Trauma, delirium, confusion (PubMed Search)
Posted: 1/14/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Imagine lying in a bed staring at the ceiling and these fuzzy faces looking down on you clearly saying something to you but you can't hear them while your hip and pelvis are hurting worse than anything you have ever felt. That's what many of our fall from standing elderly patients experience in emergency departments on a regular basis. Do not remove glasses or hearing aides from your elderly patients. Work with our EMS colleagues to make it a practice to bring glasses and hearing aides along from the scene. Speak slowly and get close to their ear to help if necessary. That confusion, delirium or dementia you assume this patient has is actually just hearing impairment and poor vision.
Category: Trauma
Posted: 1/7/2024 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
Approaching patients based on their frailty, not their age, leads to better medical decision making. A recent best practice guideline from the American College of Surgeons sums up frailty:
“It is well recognized that aging is associated with physiological decline, but this decline is not uniform across all individuals or even across one individual’s organ systems. Frailty is a geriatric syndrome, clinically distinct from age, comorbidity, and functional disability, characterized by age- associated depletion of physiological reserves that leads
to a state of augmented vulnerability to physical stressors and a diminished ability to recover from illnesses.” A trauma specific frailty index exists to identify these high risk patients.
BEST PRACTICES GUIDELINES
GERIATRIC TRAUMA
MANAGEMENT
November 2023
Trauma
Programs
American College of Surgeons
https://www.facs.org/media/ubyj2ubl/best-practices-guidelines-geriatric-trauma.pdf
Category: Trauma
Posted: 12/24/2023 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
NEXUS criteria for blunt chest trauma patients who are over 14 years old, not intubated:
>60 years old
rapid deceleration defined as fall > 6 meters or motor vehicle crash >64 km/hour
chest pain
intoxication
abnormal alertness or mental status
distracting painful injury
tenderness to chest wall palpation
If abnormal chest X-Ray proceed to chest CT. Negative predictive value of 99.9% excluding major injury.
Category: Trauma
Posted: 12/17/2023 by Robert Flint, MD
(Updated: 2/9/2026)
Click here to contact Robert Flint, MD
This commentary offers another reminder that there is significant bias in which trauma patients receive alcohol testing when that decision is made on a case by case basis. Age, sex, socioeconomic, race, injury pattern, all have been shown to influence provider ordering. Trauma systems should have pre-defined ordering criteria to eliminate this bias. The importance of gathering this testing information is to provide intervention and treatment to those in need. First we have to identify all patients in need.
Vanessa Cubas1, David N Naumann Addressing biases in alcohol testing for trauma patients: what is the solution? Emergency Medicine Journal. Volume 40 Issue 11. https://doi.org/10.1136/emermed-2023-213419
