Category: Critical Care
Keywords: heat stroke, critical care, acute kidney injury, seizures, neurological (PubMed Search)
Posted: 7/19/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Heat stroke is hyperthermia (>41.6 Celsius / 106 Fahrenheit) plus neurologic findings (e.g., altered mental status, seizures, coma, etc.); it also causes systemic inflammation response syndrome (i.e., cytokine release), coagulation disorders (e.g., thrombosis in end organs) and tissue abnormalities (e.g., acute kidney injury and rhabdomyolysis)
Two classifications exist:
Treatment includes:
Despite the most aggressive therapy, up to 30% survivors may have permanent neurologic or multi-organ system dysfunction months to years after recovery
Leon, L. Heat stroke: role of the systemic inflammatory response. Journal of Applied Physiology 2010 Dec;109(6):1980-8
http://emedicine.medscape.com/article/166320-overview
Follow me on Twitter: @criticalcarenow or Google +: @haney mallemat
Category: Visual Diagnosis
Posted: 7/10/2011 by Haney Mallemat, MD
(Updated: 8/28/2014)
Click here to contact Haney Mallemat, MD
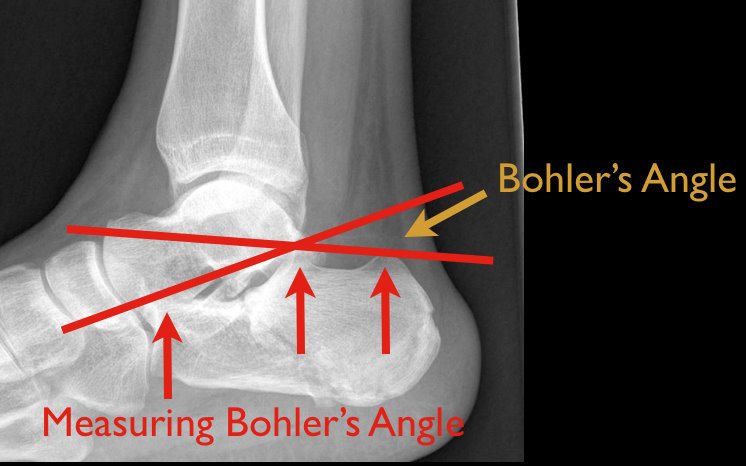
48 year old male following 15 foot fall onto both feet. What is the diagnosis?
…and why is it called the “Lover’s Fracture”?

Answer: Calcaneus fracture; historically called the “Lover’s Fracture” for “lovers” jumping out of bedroom windows to evade suspicious spouses and landing directly on their feet.
Calcaneus fractures
Rosen's Emergency Medicine: Online Edition
Follow me on Twitter @criticalcarenow
Category: Airway Management
Keywords: thyroid, hyperthyroid, hypothyroid, amiodarone (PubMed Search)
Posted: 7/5/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Amiodarone is a class III anti-arrhythmic for tachyarrhythmias
Although most patients remain euthyroid on amiodarone, 4-18% develop thyroid disease months to years after exposure.
Amiodarone-induced thyroid disease occurs because amiodarone is structurally similar to triiodothyronine and thyroxine and each 200mg tablet contains 75 mg of iodine.
Two types of amiodarone-induced thyroid disease:
Amiodarone-induced hypothyroidism (AIH)
Amiodarone-induced thyrotoxicosis (AIT)
Padmanabhan H. Amiodarone and Thyroid Dysfunction. South Med J. 2010 Sep; 103 (9): 922-30
Follow me on Twitter @criticalcarenow
Category: Visual Diagnosis
Posted: 6/27/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
49 y.o. female on Trimethoprim/sulfamethoxazole presents with rash and oral mucus membrane lesions. Diagnosis?

Answer: Steven-Johnson Syndrome
French LE. Toxic epidermal necrolysis and Stevens Johnson syndrome: our current understanding. Allergol Int. Mar 2006;55(1):9-16
Schöpf E. Toxic epidermal necrolysis and Stevens-Johnson syndrome. An epidemiologic study from West Germany. Arch Dermatol. 1991;127(6):839.
Roujeau JC. Severe adverse cutaneous reactions to drugs. N Engl J Med. 1994;331(19):1272.
Follow me on Twitter @criticalcarenow
Category: Critical Care
Keywords: AKI, critical care, ICU, cancer, renal failure, acute kidney injury (PubMed Search)
Posted: 6/21/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Cancer patients admitted to ICUs with AKI or who develop AKI during their ICU stay have increased risk of morbidity and mortality. AKI in cancer patients is typically multi-factorial:
Causes indirectly related to malignancy
Septic, cardiogenic, or hypovolemic shock (most common)
Nephrotoxins:
Aminoglycosides
Contrast-induced nephropathy
Chemotherapy
Hemolytic-Uremic Syndrome
Causes directly related to malignancy
Tumor-lysis syndrome
Disseminated Intravascular Coagulation
Obstruction of urinary tract by malignancy
Multiple Myeloma of the kidney
Hypercalcemia
Because AKI increases the already elevated morbidity and mortality in these patients, prevention (e.g., using low-osmolar IV contrast, avoiding nephrotoxins), early identification (e.g., strict attention to urine output and renal function), and aggressive treatment (e.g., early initiation of renal replacement therapy) is essential.
Benoit D. Acute kidney injury in critically ill patients with cancer. Critical Care Clinics 2010 Jan; 26(1): 151-79
Follow me on Twitter @Criticalcarenow
Category: Visual Diagnosis
Posted: 6/12/2011 by Haney Mallemat, MD
(Updated: 6/13/2011)
Click here to contact Haney Mallemat, MD
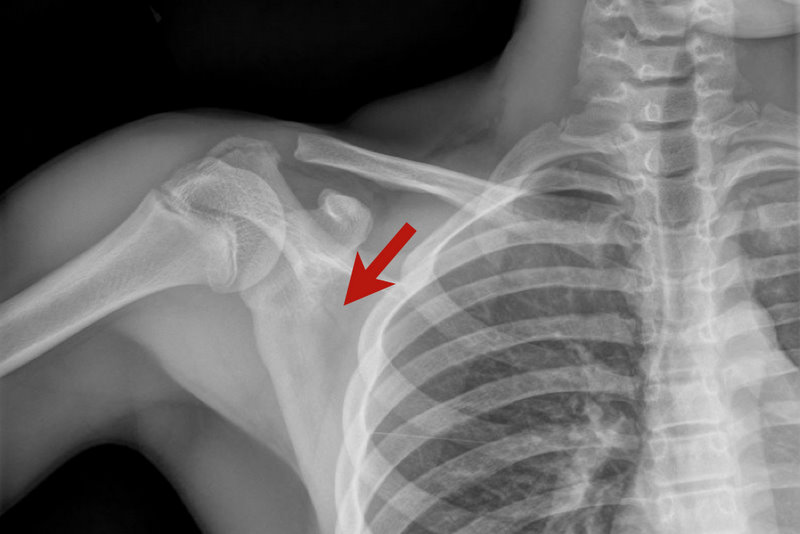
13 y.o. with shoulder trauma (during basketball game). Arm held in adduction and exquisite scapular tenderness. Diagnosis?
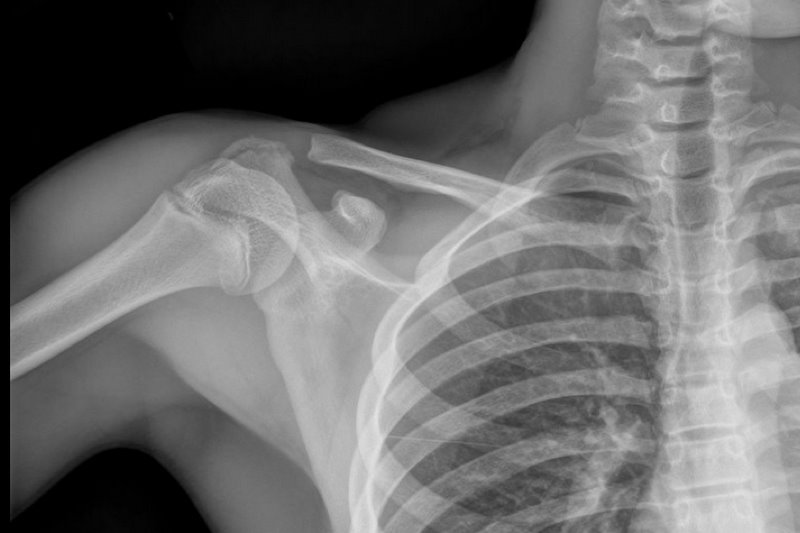
Answer: Scapular Fracture
Scapular Fracture
Uncommon (1% of all fractures)
Extensive force required; high probability of associated injuries (pneumothorax, shoulder dislocation).
5 types: body/spine, acromion, neck, glenoid, and coracoid
Arm held in adduction and pain with shoulder movement; may mimic rotator cuff tear.
Obtain X-rays (AP shoulder and lateral scapula) or CT (if displaced).
Conservative management for non-displaced fractures; Orthopedic reduction for displaced fractures.
Complications include post-traumatic arthritis or bursitis.
NSAIDs are first-line analgesics.
Rosen P, Barkin R. Emergency Medicine: Concepts and Clinical Practice. Mosby Year Book; 2010:573-574.
Zlowodzki M, Bhandari M, Zelle BA, Kregor PJ, Cole PA. Treatment of scapula fractures: systematic review of 520 fractures in 22 case series. J Orthop Trauma. Mar 2006;20(3):230-3.
Category: Critical Care
Keywords: uremia, bleeding, ddavp, estrogens, epogen, cryoprecipitate (PubMed Search)
Posted: 6/6/2011 by Haney Mallemat, MD
(Updated: 6/7/2011)
Click here to contact Haney Mallemat, MD
Bleeding associated with uremia is a spectrum, from mild cases (e.g., bruising or prolonged bleeding from venipuncture) to life-threatening (e.g., GI or intracranial bleed). The exact pathologic mechanisms are not understood, but are likely multi-factorial (e.g., dysfunctional von Willebrand’s Factor (vWF) and factor VIII, increased NO, etc.)
Besides dialysis, treatments for uremic bleeding include:
Hedges, SJ. Evidence-based treatment recommendations for uremic bleeding.NatClinPractNephrol.2007 Mar;3(3):138-53.
Category: Visual Diagnosis
Posted: 5/30/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
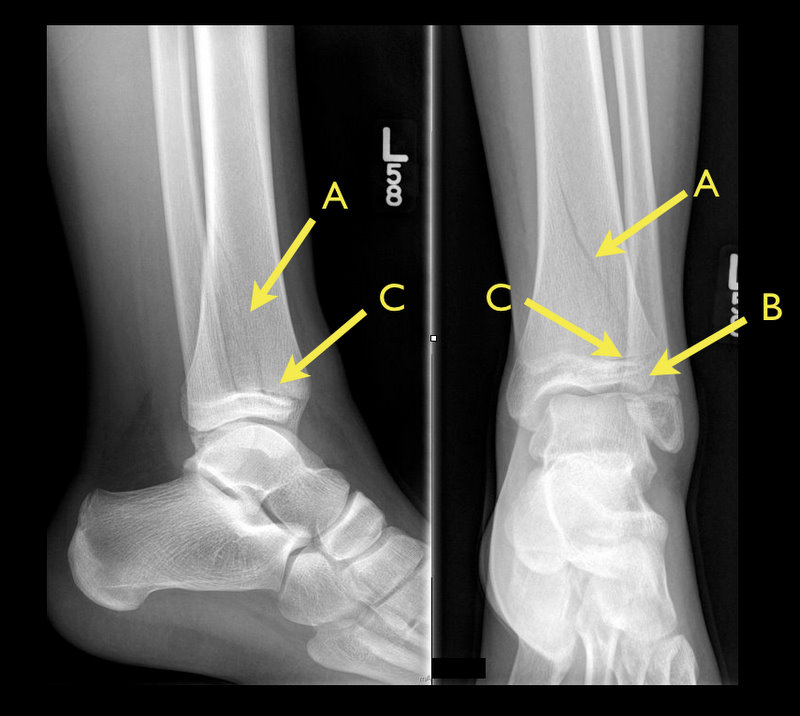
13 y.o. female with ankle pain following fall down escalator. What's the diagnosis? (Hint: Look very closely)
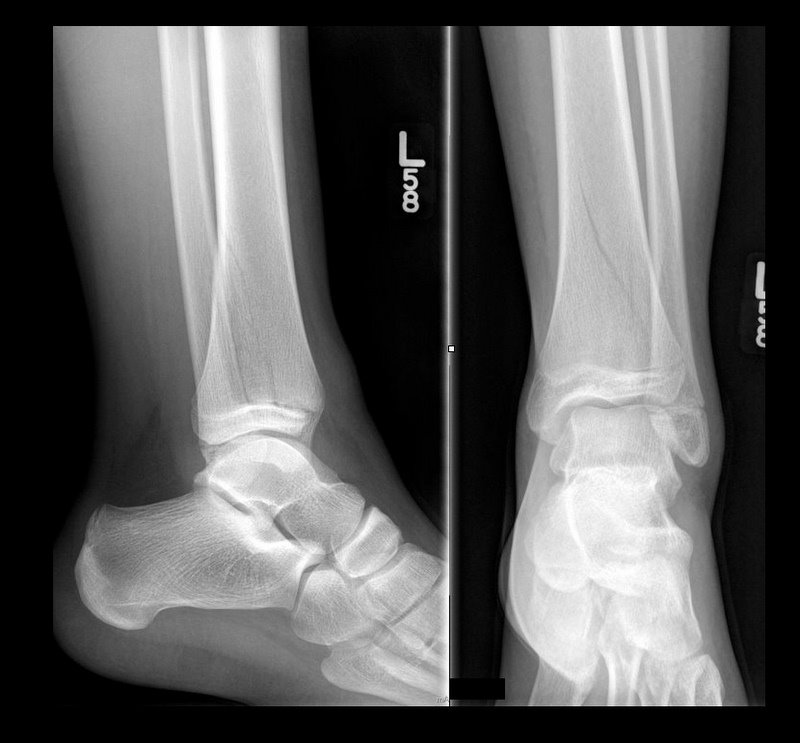
Answer: Tri-plane ankle fracture
Tri-plane Fractures (Submitted and written by Dr. Michael Santiago)

Category: Critical Care
Keywords: neutropenia, sepsis, abdominal pain, necrotizing enterocolitis (PubMed Search)
Posted: 5/23/2011 by Haney Mallemat, MD
(Updated: 5/24/2011)
Click here to contact Haney Mallemat, MD
TIP: Suspect when abdominal pain presents 10-14 after chemotherapy (when PMNs are lowest).

Blijlevens NM, et al. Mucosal barrier injury: biology, pathology, clinical counterparts and consequences of intensive treatment for haematological malignancy: an overview. Bone Marrow Transplant 2000 Jun;25(12):1269-78
http://emedicine.medscape.com/article/375779-overview
Category: Visual Diagnosis
Posted: 5/23/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
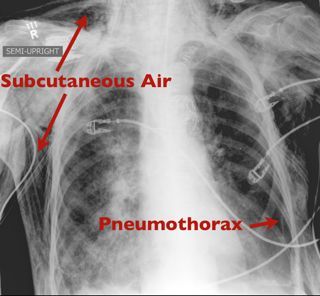
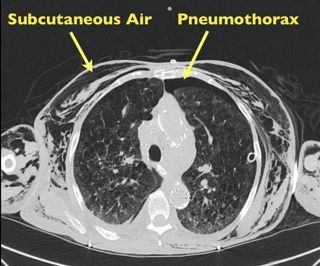
50 yo female s/p motor vehicle crash. Diagnosis?
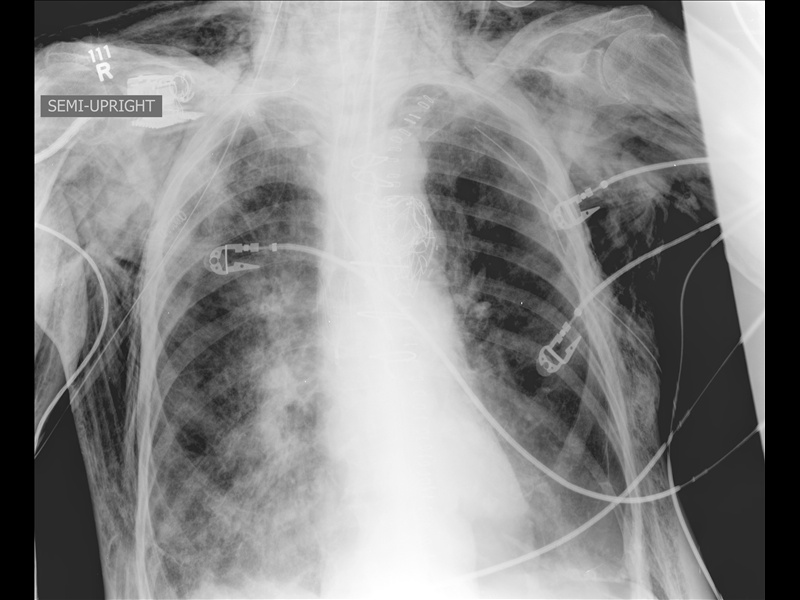
Answer: Pneumomediastinum from pneumothorax
Pneumomediastinum
Mediastinal air has multiple causes:
Listen for Hamman's sign ("crunching" with cardiac auscultation) and feel for crepitus (distinct feeling on palpation).
Treat the precipitating cause.
Usually resolves without mediastinal decompression; air travels along tissue planes decompressing increased mediastinal pressure.
Category: Critical Care
Keywords: Clostridium difficile, diarrhea, critical, ICU, sepsis, abdominal pain, vanocmycin,metronidazole, fidaxmicin (PubMed Search)
Posted: 5/10/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Although oral metronidazole is indicated for mild to moderate Clostridium difficile associated diarrhea, oral vancomycin should be considered first-line therapy in critically-ill patients with moderate to severe disease. Vancomycin dosing should begin at 125mg PO q6 and increased to 250mg q6 if poor enteral absorption exists. Consider adding metronidazole IV if either reduced enteral absorption or severe disease exists.
Recently, fidaxomicin has been shown to be non-inferior to oral vancomycin in the treatment of mild to moderate C. difficile. While promising, the study population was not critically-ill and extrapolation should be avoided.
Riddle, D. Clostridium difficile infection in the intensive care unit. Infect Dis Clin North Am. 2009 Sep;23(3):727-43.
Category: Visual Diagnosis
Posted: 5/9/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
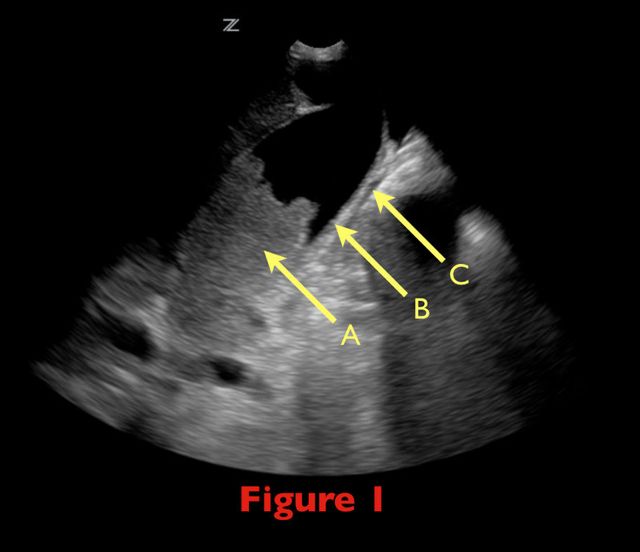
70 yo female from nursing home with fever. RUQ ultrasound is shown below. Diagnosis?

Acalculous Cholecystitis
Acalculous cholecystitis is due to gallbladder (GB) wall ischemia and GB stasis (reduced GB contraction from reduced PO intake)
which all leads to “sludging” (Figure 1; A), thickened GB walls (B), and pericholecystic fluid (C).
Risk factors include critical illness (especially sepsis), acute cholecystitis, total parenteral nutrition, diabetes, and GB dysmotility.
Treatment includes antibiotics covering enteric / biliary pathogens and cholecystectomy (if a surgical candidate) or percutaneous
cholecystostomy if unsuitable for the OR.
Complications include perforation, GB gangrene, and extrabiliary abscess.
Category: Critical Care
Keywords: sepsis, shock, antimicrobials, combination, antibiotics (PubMed Search)
Posted: 4/26/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
A mortality benefit from combination antimicrobial therapy has not been clearly demonstrated in sepsis. However, when only the most severely-ill patients (i.e., septic shock) are considered in subgroup analysis, there appears to be a mortality benefit to using two antimicrobials against a suspected organism.
Combination antimicrobial therapy may reduce mortality through three mechanisms.
Always obtain appropriate cultures before initiating therapy. Although identification and susceptibility of the organism may take some time, eventually narrowing antimicrobial therapy to monotherapy in the ICU is still recommended.
Abad, C. Antimicrobial Therapy of Sepsis and Septic Shock: When are Two Drugs Better Than One? Crit Care Clinic 27 (2011) e1-e27.
Category: Visual Diagnosis
Posted: 4/25/2011 by Haney Mallemat, MD
(Updated: 2/8/2026)
Click here to contact Haney Mallemat, MD
Patient presents with the following X ray after yawning. Diagnosis?

Diagnosis: Mandibular Dislocation
The link below demonstrates an interesting alternative to the traditional reduction method; prospective randomized trails are pending.
Thanks to Dr. George Kochman for the image and Dr. Christopher Doty (EM Program Director at SUNY Downstate / Kings County Hospital Center) for the video.
Category: Critical Care
Keywords: Vancomycin, Daptomycin, Linezolid, MRSA, gram positive, infections, sepsis, pneumonia (PubMed Search)
Posted: 4/12/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Vancomycin is often started empirically for gram-positive and MRSA coverage. Although effective and generally well-tolerated, emerging resistance and side-effect profiles limit its use in some patients. Two alternatives are Linezolid and Daptomycin.
Linezolid
Daptomycin
Alder, J. The Use of Daptomycin for Staphylococcus Aureus Infection in the Critical Care Medicine. Crit Care Clin 24(2008); 349-363.
Category: Visual Diagnosis
Posted: 4/10/2011 by Haney Mallemat, MD
(Updated: 4/11/2011)
Click here to contact Haney Mallemat, MD
60 y/o male transferred from local rehab facility c/o abdominal pain.

Ogilvie's syndrome / Acute colonic pseudo-obstruction (ACPO)
Syndrome of decreased GI motility believed to be an autonomic imbalance (specifically, parasympathetic suppression) predominantly in the cecum and right colon. ACPO is also commonly due to narcotic overuse / abuse.
Differential diagnosis:
Abdominal XR:
Treatment:
Fazel A, Verne GN. New solutions to an old problem: Acute colonic pseudo-obstruction. JClin Gastroenterol 2005; Vol 39(1): 17-20.
Ozkurt H, Yilmaz F, et al. Acute colonic pseudo-obstruction (Ogilvie's syndrome): radiologic diagnosis and medical treatment with neostigmine. Report of 4 cases. Am J of Emer Med 2009; Vol 27: 757.e1 - 757e4.
Category: Critical Care
Keywords: bilevel ventilation, bipap, cpap, respiratory failure, respiratory distress, copd, acute pulmonary edema (PubMed Search)
Posted: 3/29/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Emergency Medicine physicians are gaining experience with non-invasive ventilation (i.e., Bi-level ventilation and continuous positive-pressure ventilation) in managing respiratory distress and failure. Although NIV is commonly used across a variety of pathologies, the best data exists for use with COPD exacerbation and cardiogenic pulmonary edema (CHF, not an acute MI)
Although other indications for NIV have been studied, the data is less robust (eg., smaller study size, weak control groups, etc.). If there are no contraindications, however, many experts still support a trial of NIV in the following populations:
Failure to clinically improve during a NIV trial should prompt invasive mechanical ventilation.
Keenan, S. et al. Clinical practice guidelines for the use of noninvasive positive-pressure ventilation and noninvasive continuous positive airway pressure in the acute care setting. CMAJ. 2011 Feb 22;183(3):E195-214. Epub 2011 Feb 14.
Category: Visual Diagnosis
Posted: 3/27/2011 by Haney Mallemat, MD
(Updated: 3/28/2011)
Click here to contact Haney Mallemat, MD
25 year old male presents after falling from 10 feet and landing on right shoulder. Diagnosis?

Yes...the shoulder is dislocated, but did you notice anything else? (see figure 1)
Glenoid Fossa Fracture: (Image submitted by Dr. George Kochman)
Fractures of the glenoid fossa occur when the head of the humerus collides with the glenoid margin; classically, by a laterally directed force. Although less than 10% of glenoid fossa fractures result in significant displacement, surgical repair is indicated if:

Schmidt, J. Scapular Fracture. eMedicine. January 12, 2011.
http://emedicine.medscape.com/article/826084-overview
Category: Critical Care
Keywords: pulmonary physiology, critical care, respiratory alkalosis (PubMed Search)
Posted: 3/15/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
Many changes in pulmonary physiology occur during pregnancy. These changes are generally well tolerated but can become problematic when pathologic states arise.
Here are a few examples of the normal changes and potential consequences:
Progesterone increases tidal volume and respiratory rate.
“Normally" a mild respiratory alkalosis pH 7.4-7.47, PaCO2 28-32, and bicarbonate 17-22 (renal compensation).
Low metabolic reserve with systemic illness.
Weight gain, anasarca, and breast size reduces chest wall elasticity.
Potential for restrictive physiology and reduced lung volumes.
Can be challenging to to mechanically ventilate due to decreased compliance and intra-thoracic pressure
Mechanical displacement of abdominal and thoracic contents by growing uterus.
Reduced lung volumes leading to reduced oxygen reserve and decreased apnea time.
Aim higher if placing chest tube (avoid abdominal contents)
Uterine pressure on stomach can increase aspiration risk and pulmonary injury.
Chestnutt, A. Physiology of Normal Pregnancy. Crit Care Clinic 20 (2004) 609-615
Category: Visual Diagnosis
Keywords: lung, ultrasound, pneumonia, hepatization, sonogram, air bronchograms (PubMed Search)
Posted: 3/13/2011 by Haney Mallemat, MD
Click here to contact Haney Mallemat, MD
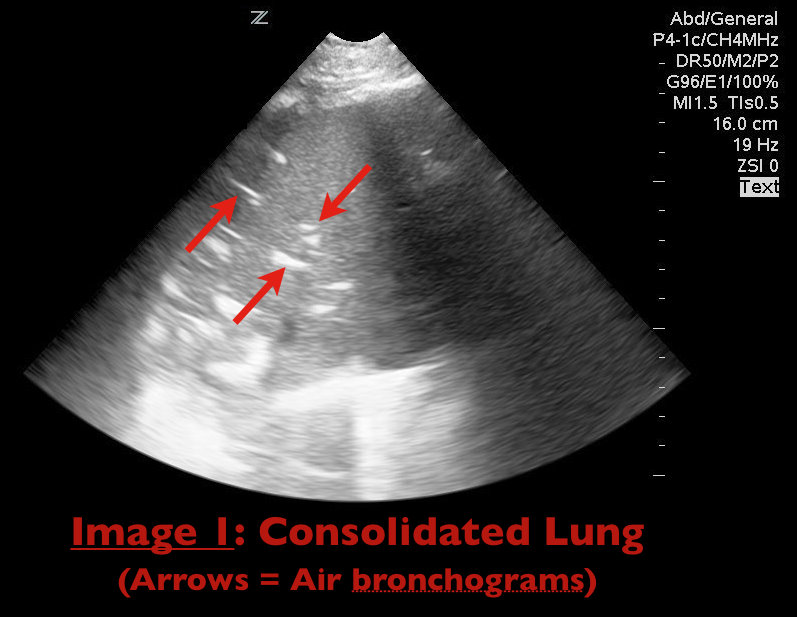
65 yo female with breast cancer presents with dyspnea and CXR shown below. Diagnosis? Can anything help clarify the diagnosis?
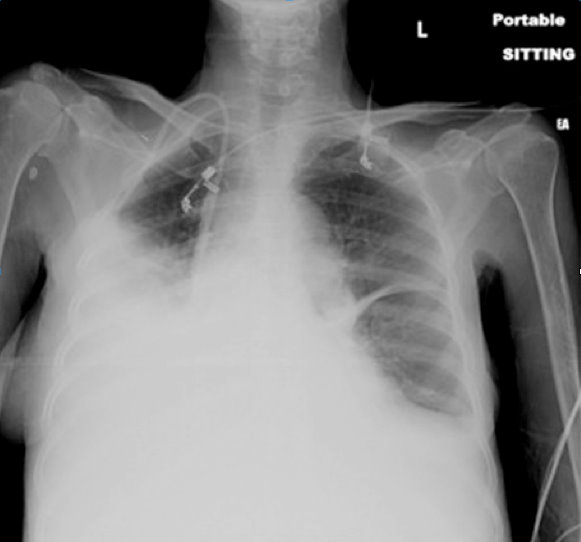
The CXR shows an opaque right hemithorax, consistent with a pleural effusion, a large consolidation, or both. Ultrasound of the lung can clarify this ambiguity.
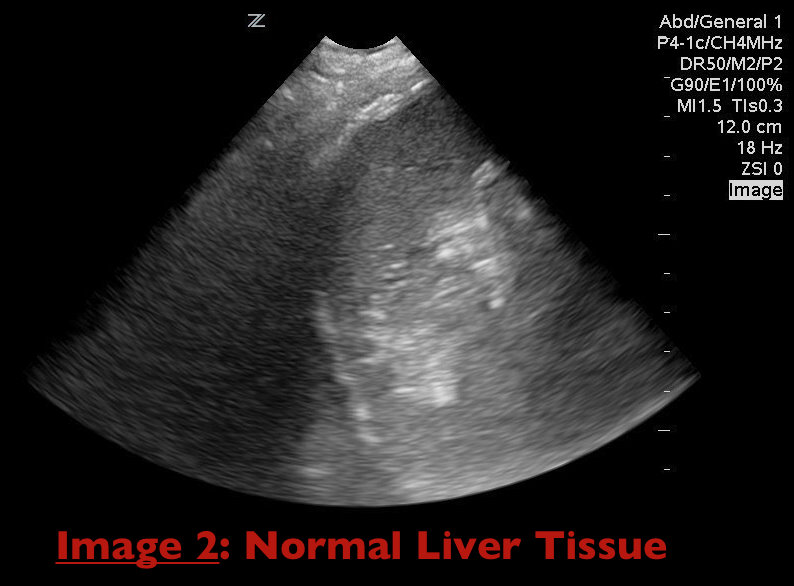
Consolidation of lung parenchyma (e.g., pneumonia) appears isoechoic to liver tissue on ultrasound and air bronchograms appear as hyperechoic areas within the consolidated lung parenchyma (Image 1). Together these findings are termed "hepatization" of the lung as consolidated lung appears similar to liver parenchyma on ultrasound (Image 2).
Durant, A. Nagdev, A. Ultrasound detection of Lung Hepatization. West J Emerg Med. 2010 September; 11(4): 322-323.
